Public health action through community partnership: Epidemiological and cultural insights after the 2015-2016 mumps outbreak in the Kimberley, Western Australia
Original article (peer reviewed)Eastwood A, Haenga M, Kelly G, Bin Demin J, King T, Lewis P, Davies P, Morgan-Dann R, Masuda L, Banks A, Ward J (2018)
Corresponding author: Eastwood A, A/Public Health Manager, Kimberley Population Health Unit, Department of Health, 5/9 Napier Terrace, PO Box 525, Broome 6725, email: Ashley.Eastwood@health.wa.gov.au
Suggested citation:
Eastwood A, Haenga M, Kelly G, Bin Demin J, King T, Lewis P, Davies P, Morgan-Dann R, Masuda L, Banks A, Ward J (2018) Public health action through community partnership: Epidemiological and cultural insights after the 2015-2016 mumps outbreak in the Kimberley, Western Australia. Australian Indigenous HealthBulletin 18(4) Retrieved [access date] from
Abstract
Objective
We integrated epidemiological and cultural insights in reviewing the public health response to a mumps outbreak declared in the remote Kimberley region of Western Australia in April 2015.
Methods
An iterative process of engagement culminating in co-authorship with an Aboriginal Reference Group (ARG) of our outbreak responses, reflections and future directions.
Results
This mumps outbreak was found to affect predominantly Aboriginal teenagers and young adults with pre-existing high mumps vaccination coverage. Outbreak declaration invoked campaigns to implement a booster dose of MMR (Measles, Mumps Rubella) vaccine irrespective of previous vaccination history to people aged 8 to 35 years who were contacts of cases, extended household members, or who resided in nine remote Aboriginal communities. In town settings and regional centres, 8 to 35 year olds in targeted households who had cultural links and frequent movement to and from the affected nine communities were also offered booster MMR vaccine. Following 3,102 MMR vaccines, transmission was effectively halted. In collaboration with the ARG, a fuller picture of particular opportunities for transmission and geographic spread afforded through sports events, Native Title meetings, royalty meetings, funerals and cultural ceremonies was retrospectively gained. The ARG also identified how to strengthen Aboriginal participation in future public health outbreak measures.
Conclusions
Retrospective sharing by the ARG of their knowledge of cultural dimensions of remote Aboriginal communities clearly enlightened the Public Health Team’s understanding of communicable disease transmission across the region.
Implications
Future outbreaks will be better managed in a culturally secure way.
Download PDF version (434KB)
Introduction
Community engagement with Indigenous peoples living in rural and remote Australia about communicable diseases brings unique cross-cultural challenges [1]. Strategies to build both evidence and better community engagement are needed [2]. To date, such collaborative strategies have not been a systematic feature of communicable disease control in the Kimberley region of Western Australia (WA).
Mumps has been nationally notifiable in Australia since 2001. Low rates of notification have been observed over the past 15 years until the national notification rate rose dramatically during 2007 due to a large mumps outbreak characterised by intense and sustained local transmission primarily affecting Aboriginal people not only in the Kimberley region but across the Northern Territory (NT) [3-6]. Outbreaks in vaccinated populations have also been reported internationally [7-13]. Continual adjustment of immunisation policy is required. In 2015, the Australian Immunisation Schedule listed mumps vaccination as part of the Measles, Mumps, Rubella vaccine (MMR vaccine) for administration twice in a person’s life: the first MMR vaccine is scheduled for 12 months and the second at 18 months (the latter combined with varicella) (MMRV vaccine) [14]. In the Kimberley, early childhood vaccination coverage is typically > 90% [15].
On 31 March 2015, a case of mumps was notified to the Public Health Team (PHT) in the Kimberley Population Health Unit (KPHU) ahead of four more subsequently investigated and confirmed. By 14 April 2015, KPHU had sufficient epidemiological evidence to declare a mumps outbreak on 17 April 2015 which lasted until October 2016. Acknowledging our desire to better comply with cultural safety as a core principle in outbreak report writing with Aboriginal peoples [16], cultural learnings were formally obtained for the first time in collaboration with an Aboriginal Reference Group (ARG) who received and considered key epidemiological findings and decisions taken during the outbreak’s course. Our collective experience is co-authored here.
Procedures
Epidemiology of the 2015-2016 mumps outbreak in the Kimberley
To review the epidemiology of the 2015-2016 mumps outbreak, we retrieved regional disease outbreak reports and epidemiological curves (‘epi curves’) produced during the mumps outbreak and reviewed all documentation including minutes of meetings, public communications and internal notes.
Consultations with the Aboriginal Reference Group (ARG)
An Aboriginal Reference Group (ARG) was essential to deepen our understanding of the transmission of mumps in the Kimberley and to inform the design of future measures to interrupt disease transmission during outbreaks more effectively. GK and JBD compiled an initial list of names to ensure a broad representative ARG following consultation with Aboriginal leaders and Aboriginal health staff. Aboriginal executives in senior positions in local services including the WA Country Health Service (WACHS) and Aboriginal community-controlled health services (ACCHOs) as well as Nindilingarri Cultural Health Services, Nirrumbuk Aboriginal Corporation and other local community-controlled companies were then added. Consultations then occurred with 24 Kimberley Aboriginal people ranging in age, language group, kinship, seniority and place of residence. These occurred via group meetings where possible or by individual contact through face to face interviews, telephone calls and emails, creating a virtual ARG despite the distances of the region. This ARG provided a deep cultural insight into the social dynamic of the outbreak using a strengths-based lens and the cultural appropriateness of our response from an entirely Aboriginal perspective. Responses were initially categorised into themes by AE and discussed by all authors. A core of ARG members also co-authored this publication.
Because ARG members were from diverse backgrounds, all meetings began with an overview of key epidemiological concepts including ‘case’, ‘incidence’, ‘outbreak’ and ‘attack rate’ as well as ‘vaccination efficacy’, ‘vaccination effectiveness’, ‘population coverage’, ‘boosters’ and ‘denominators’. We explained to the ARG some of the putative reasons for mumps outbreaks in highly vaccinated populations including (1) waning immunity even after completion of recommended vaccination courses (2) potentially reduced cross protection from existing immunity (whether sustained or not) obtained from the phylogenetically distinct genotype A Jerryl Lynn strain in the vaccine when a person’s immune system was confronted by the genotype G wild type virus (3) suboptimal vaccine effectiveness (4) some unknown inherited attribute causing Aboriginal people to have a lower immune response to mumps vaccination and/or (5) postulated differences in disease transmission due to social circumstances, colonial legacies and disempowerment creating environments of high mobility and settings of intense exposure. We shared our main epidemiological findings with the ARG also explaining the rationale for each key decision including community-wide mass vaccination initiatives. With respect to community-wide mass vaccination initiatives, we also explained why the indicator of success would be the number of cases of mumps occurring more than four weeks after such an initiative (‘postvaccination Phase 2’) [17].
In turn, the ARG shared with PHT members their knowledge of Aboriginal communities, their cultural practices, cultural and kinship links, travel between communities and into regional centres, seasonal population fluctuations, daily pressures and impacts of successive government policies. This ARG identified strengths in communities, emphasised opportunities to work ‘with’ communities and reflected on the specific features of the public health response which would benefit from further strengthening.
Ethics
Data variables such as case vaccination status and sero-typing had been collected and confirmed during outbreak management by public health staff. Ethics approval to initiate formal consultation with the ARG and publish findings was obtained from WA Country Health Service (WACHS) Human Research Ethics Committee [Reference Number 2016/02 approved 17 February 2016]; WACHS Site Specific Assessment approved 14 January 2016 and Aboriginal Health Council of Western Australia Reference Number HREC 691 approved 10 February 2016. KAHPF Research Committee endorsed 15 January 2016.
Main findings
Early outbreak experience
There were no locally acquired cases of mumps in the Kimberley from 2009 until March 2015. Early notifications were assessed using the Surveillance Case Definitions for Notifiable Infectious Diseases and Related Conditions in Western Australia [18]. On 17 April 2015, KPHU declared a mumps outbreak on the basis of five confirmed cases in the one community providing the necessary epidemiological criteria (Figure 1). Prior to that date, public health advice had been consistent with that for a sporadic case. As explained to the ARG, public health recommendations for sporadic cases in the Kimberley comprised voluntary isolation of cases and vigilance with respect to age-appropriate ‘catch-up’ mumps vaccinations for any child overdue in the household or named close contacts. Nearly all (22/24) ARG members described isolation of sporadic cases as problematic given shared living conditions and obligations to visiting family members as well as household density and cultural commitments such as law, sorry camps sporting events, and governance obligations including Native Title meetings. If linguistically appropriate information on routes of transmission could be provided, Aboriginal people would develop their own locally effective and culturally appropriate methods of protecting others. So informed, infectious people would be more likely to adopt personal strategies to prevent transmission e.g. sitting on the periphery of a group, coughing and sneezing hygiene, handwashing, not sleeping in rooms with young children and/or elderly people.
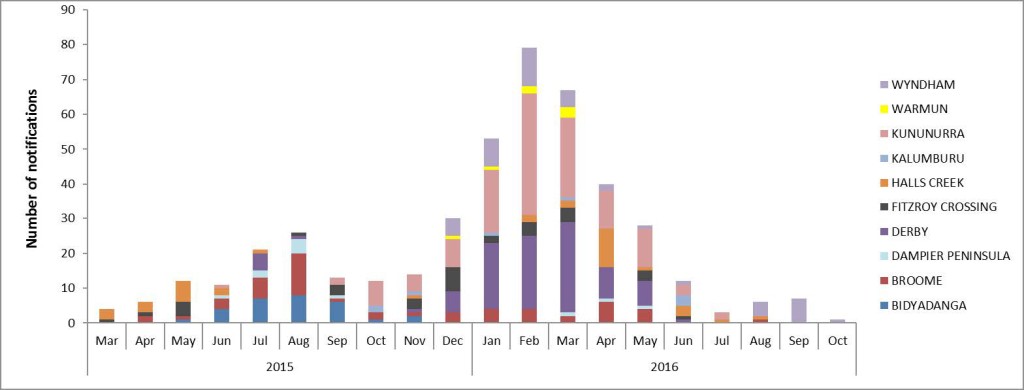
Figure 1: Epicurve of the Kimberley Mumps Outbreak March 2015 to October 2016 by locality
The ARG were also shown the temporal and geographical transmission of mumps across the region in map and epicurve form (Figure 1). Their insights in response included the seasonal movement of people to towns during the wet season (November 2015 to March 2016) and recollections of sports events, Native Title meetings, royalty meetings, funerals, cultural ceremonies and festivals. Movement patterns within the region have been explored [19-21]. Members of the ARG shared their knowledge of unmapped transport routes between communities, into other regions and across the NT border. Previously unknown kin and cultural links between communities in the west Kimberley to those in the east Kimberley were revealed. As one ARG member stated, ‘once it’s in the Kimberley, it will get everywhere’.
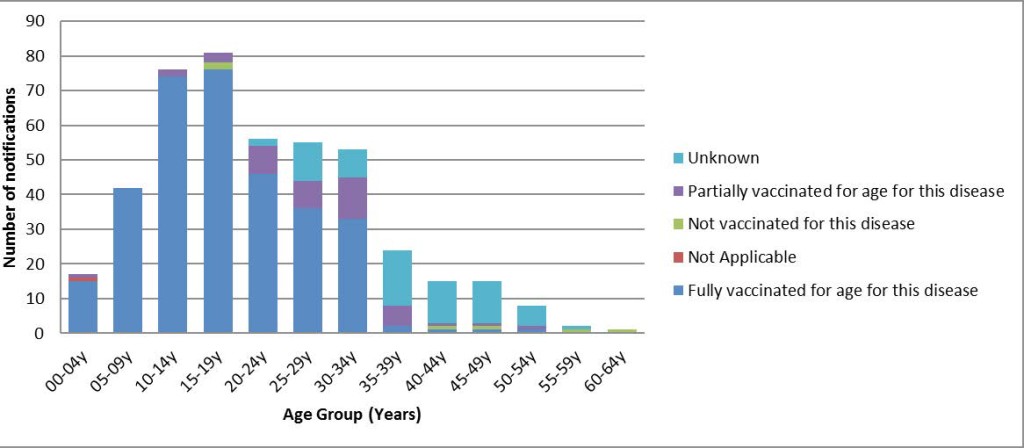
ARG participants expressed considerable interest in understanding the biological mechanisms for mumps vaccination, why vaccinated people were affected and why those people were primarily Aboriginal people. As shown in Table 1, 74% of cases from March 2015 to October 2016 were ‘fully’ vaccinated; 11% ‘partially’ vaccinated and 1% not at all (vaccination status unknown for 14%). The ARG also appreciated learning more about why mumps could occur in a highly vaccinated population. The epidemiological picture of the Kimberley mumps outbreak was presented to the ARG in chronological order. Figure 1 shows the age distribution of Kimberley cases. Table 2 shows the vaccination status and heritage of all outbreak cases. Vaccine status was associated with age (Figure 2). Widespread transmission was observed across the Kimberley as well as in other regions in country WA with metropolitan cases in Perth occurring in boarding schools attended by Kimberley students [22].
Table 1. Vaccination status of mumps cases in the Kimberley March 2015 to October 2016
| Vaccination Status | Non-Aboriginal | Aboriginal | Total | % Fully Vaccinated |
|---|---|---|---|---|
| Fully vaccinated for age for this disease | 21 | 309 | 330 | 74 |
| Not Applicable | 1 | 1 | 0 | |
| Not vaccinated for this disease | 3 | 3 | 6 | 1 |
| Partially vaccinated for age for this disease | 5 | 42 | 47 | 11 |
| Unknown | 15 | 46 | 61 | 14 |
| Grand Total | 44 | 401 | 445 | 100 |
Table 2. Aboriginal and gender status of 445 notified cases of mumps in the Kimberley from March 2015 to October 2016
| Gender | Non-Aboriginal | Aboriginal | Grand Total |
|---|---|---|---|
| Female | 26 | 194 | 220 |
| Male | 18 | 207 | 225 |
| Grand Total | 44 | 401 | 445 |
Figure 2. Vaccination status of confirmed mumps cases by age group
Public health outbreak response
Upon declaring the outbreak, PHT co-ordinated all public health responses. At that time, there were no available regional, state or national guidelines with which to structure public health responses to a mumps outbreak. This was addressed immediately by drafting local procedures to aid decision-making which were later adopted state-wide. PHT continued to release Public Health alerts to clinicians as well as multimedia alerts to communities.
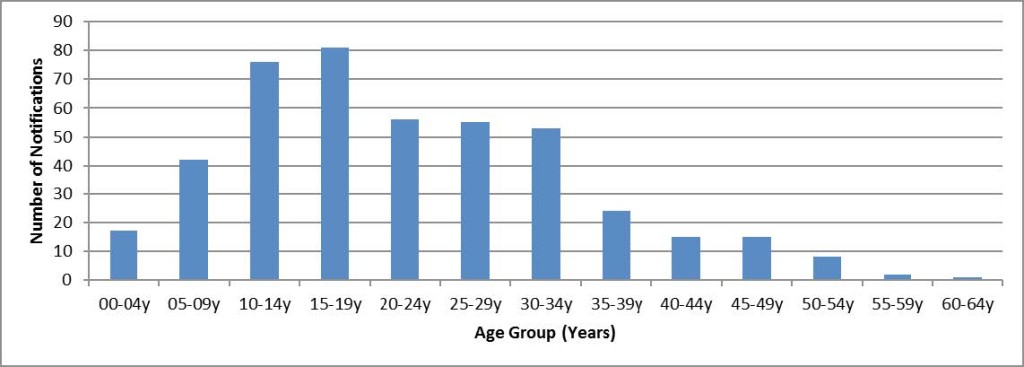
We next showed the ARG how early epidemiological features of the outbreak informed decisions about the target age group in the Kimberley for household, neighbourhood and community-wide mass booster initiatives (See Figure 3). From published outbreak reports [6,12,17,22-24] we had hypothesised early that waning immunity was a major contributing factor to the mumps outbreak in this highly vaccinated population. Postulating that incremental waning of immunity occurs and that protection declines five years after the second dose of MMR, we concluded that the age group for a targeted booster should be 8 to 35 years. Prior to 2013, MMR2 could be given at school entry at the minimum age of 3 years and 6 months. People aged 35 years and older were expected to have been exposed to circulating wild type mumps viruses and therefore received natural boosting of immunity if not also to have had mumps infection as a child.
Figure 3. Mumps Cases by Age Group March 2015 to October 2016
Booster vaccination of close household contacts was invoked for any first case in a remote community or town setting. For every case, circumstances of the household first were assessed by primary health care (PHC) staff to identify ‘close contacts’. Being a ‘close contact’ was defined as anyone who lived in the same house or had slept in the house in the two days before and five days after the case’s onset of symptoms. Once identified, each close contact aged between 8 years and 35 years was informed by PHC staff of their risk and offered mumps vaccination irrespective of their vaccination status. Benefits and harms of vaccination in this context were explained. Close contacts were informed that the vaccination would not protect them if they had already caught mumps and were pre-symptomatic but that it would help in future contact with an infected individual after 4 weeks.
Mass mumps vaccination initiatives
Whenever a second or further case(s) had occurred in a remote community setting within the incubation period of the initial case but not epidemiologically linked as a ‘close contact’, the PHT was required to assess whether or not to extend MMR vaccination to everyone in the community aged between 8 and 35 years of age. By contrast, when cases occurred in regional towns where there is very porous people traffic between specific houses based on kinship although not necessarily throughout the entire town, PHT assessed whether to offer booster vaccination to everyone in targeted households within the specified age group according to specific criteria appropriate to the Kimberley as described later.
As recommended by the Centre for Disease Control (CDC) in the United States at that time [25], large-scale mumps ‘booster vaccination’ at community level should be considered when there is evidence that there may be a sufficient number of individuals in that defined population group susceptible to mumps infection. At the time of the 2015-2016 Kimberley mumps outbreak, CDC did not routinely recommend a third dose of mumps-containing vaccine for mumps outbreaks in highly vaccinated populations [25]. Rather, criteria for deciding whether this would be useful included:
- two-dose vaccination coverage at least 90%;
- intense exposure settings likely to facilitate transmission (such as schools, colleges, correctional facilities, congregate living facilities, close-knit communities) or healthcare settings;
- high attack rates (in the US, >5 cases per 1,000 population)
- evidence of ongoing transmission for at least two weeks in the target population (that is the population with the high attack rates) [25]
In our discussions with the ARG, we explained why a third or booster dose of MMR was offered either for targeted households only or designated community-wide mass vaccination initiatives. PHT made the decision about community-wide mass vaccination using specific epidemiological and social criteria in consultation with CDCD when required. As explained to the ARG, community-wide mass vaccinations were undertaken only after careful consideration of rationale, engagement of the local primary health care service, local environmental health (EH) service and community consultation. Although mindful that the international literature was mixed in terms of the likely net benefit for remote Aboriginal communities, the PHT concluded that benefits of booster MMR vaccination in an outbreak where there were intense exposure conditions exceeded harms at both individual and population levels. The prolonged Kimberley outbreak of 2007-2008 did not invoke booster initiatives [6]. In response to that outbreak, only catch-up vaccinations had been offered for those overdue or with unknown vaccination status [6]. The PHT also considered timing of large social gatherings including sorry business and law business, known usually to local community members.
Once it was decided that an entire remote community or circumscribed town neighbourhood required mass vaccination, extensive planning and co-ordination took place with local services and the PHT. Planning details were recorded including geographic footprints to be targeted and estimates of age-specific denominators. Data collection sheets were distributed. Vaccine stocks augmented. Health promotion material and posters were developed and distributed. Individuals in affected communities who were offered vaccination were informed that they could still develop mumps if they had already been infected and were incubating the virus asymptomatically at the time of vaccination. Outcome data were recorded including occurrence of mumps among recipients of the mumps vaccine and its timing: specifically, anyone developing symptoms or signs of mumps within four weeks of booster vaccination was either already incubating at the time of vaccination or symptomatic from the vaccine itself (post-vaccination phase 1). Anyone developing symptoms or signs of mumps after four weeks was deemed a case due to ‘booster vaccine failure’ (post-vaccination phase 2) [17]. If parotitis occurred within four weeks of vaccination, laboratory testing using buccal swab PCR was encouraged to discriminate between infection with wild type genotype G and vaccine derived genotype. Genotyping was performed on four PCR samples where parotitis occurred within four weeks of vaccination. All were found to be wild type genotype G confirming mumps infection. Known cases did not need to be immunised during these booster initiatives.
Community-based mass vaccination initiatives were feasible only in isolated communities because resources could be galvanised through local primary health care staff deployment and local partnerships. Furthermore, the social fluidity in remote communities seemed to be qualitatively different to those living in towns. By contrast, planning for and implementation of mass vaccination initiatives in ‘town-based initiatives was confined to contiguous houses, neighbourhoods or streets depending upon the social circumstances of the case, their kinship connections and those meeting criteria for a ‘close contact’. Local environmental health teams and cultural navigators provided contemporaneous knowledge of households connected to affected remote communities and kinship and cultural complexes to identify which households required MMR booster due to increased susceptibility to transmission whether due to cultural and geographic connections or household size.
As a consequence of these decisions, there were 3,102 MMR vaccines administered from March 2015 to September 2016. Of these, 1,187 were administered in pre-planned community-wide mass vaccination initiatives in 9 remote communities (see Table 3). With respect to the proportion of the population aged 8 to 35 years of age who were provided booster vaccination in each community, Table 3 shows this ranged from 36% to 100% based on denominator data from the 2011 Australian Bureau of Statistics Census. Booster dose effectiveness in preventing further cases four weeks or later from vaccination was convincing. As explained to the ARG, three out of the nine communities had no mumps cases after a four week period (Table 3). Four out of the nine communities had 1-3 cases after a four-week period. That one community meeting criteria for community-wide vaccination twice had low booster vaccination coverage (36%) in the first public health response and had 12 cases after a four-week period from its first booster initiative (Table 3).
Table 3. Results for community-wide mass vaccinations of people aged 8-35 years in remote Kimberley communities
| Code | Date | Estimated population of 8-35 year olds# | N vaccines administered | Proportion of targeted population vaccinated | Number of new mumps cases >4 weeks from initiatives |
|---|---|---|---|---|---|
| BA | Early May 2015 | 260 | 316 | 100% | 1 |
| BI | Early May 2015 | 105 | 68 | 65% | 0 |
| M | Early May 2015 | 66 | 45 | 68% | 2 |
| BIA
1st booster initiative |
Early July 2015 | 288 | 82 | 36% | 12 |
| BIA second booster initiative | Late July 2015 | 288 | 150 | 81%* | 10 |
| LA | Late July 2015 | 152 | 178 | 100% | 0 |
| AY | Late July 2015 | 129 | 111 | 86% | 2 |
| LB | Late July 2015 | 84 | 67 | 80% | 0 |
| BB | Late July 2015 | 109 | 116 | 100% | 3 |
| K | Late November 2015 | 244 | 154 | 63% | 5 |
- # denominators estimated from the 2011 ABS census.
- *the coverage rate is estimated by adding the number of vaccines given on the first community vaccination initiative (n=82) to those given during the second community booster initiative (n=150) Total vaccines given = 232
Overall, 20 cases of mumps developed in any person four weeks or more after a community-based or targeted household booster initiative. Twelve of these occurred in one community where community wide vaccination was attempted on two occasions separated by a period of 2 weeks. On the first attempt, only 82 people were vaccinated out of an estimated population of 288 8-35 year olds due to staff vacancies at the primary health care clinic that day which limited workforce capacity to deliver vaccinations. This equated to a vaccination coverage rate of 36%. On the second occasion, a further 150 people were vaccinated. The total vaccination coverage after the second community-wide vaccination was 81%.
Microbiology and typing
On 22 April 2015, KPHU had been advised by PathWest that the genotype found in all PCR swabs as taken by clinicians up to that time was genotype G. For the first six months of the outbreak, all throat or buccal swabs that were collected and successfully genotyped showed infection with genotype G. This outbreak genotype was not the same as genotype J seen earlier in 2007 [6]. Across WA, transmission with genotype G continued with new cases of at least 28 cases per week at the outbreak peak almost exclusively in highly vaccinated Aboriginal children, teenagers or adults to age 45 years (Armstrong, personal communication, 18 November 2015). Where genotyping had occurred, all cases developing mumps within 4 weeks of receiving an MMR booster had genotype G.
Outbreak resolution
The Kimberley mumps outbreak was declared over in October 2016 once two incubation periods had lapsed since the last reported case. In the later months of 2016, there were typically fewer than four cases per week in the region with all confirmed as being epi-linked to an index case. Further, one household that had refused to participate earlier in vaccination accounted for these later cases. State-wide analyses as presented initially in 2016 including adjusted attack rates for immunized and unimmunised groups before and after targeted and community-wide initiatives will add to epidemiological understanding [22].
Success factors and future improvements
Public health action worked particularly well when:
- community engagement was initiated by people already known to the community
- local Aboriginal environmental health staff were highly visible
- local planning, discussion and communication occurred through inter-sectoral collaborations at the local level with PHC, schools, major employers and environmental health services
- community leaders and elders were educated about this specific mumps outbreak and themselves took up the key roles of advocate, health educator and cultural navigator.
By contrast, poorer community engagement and reliance on communications through unfamiliar FIFO (Fly in Fly out) public health staff or new PHC staff who may have not fully understood cultural dimensions of public health practice in the Kimberley compromised impact.
Additional ARG reflections
As shown in Box 1, recurring themes in ARG reflections to support public health action included the importance of community awareness of mumps as a communicable disease and the rationale for outbreak actions; attention to jargon-free communication and the value of pre-existing linkages to community organisations. There was also spontaneous recognition of the role of environmental determinants. Publicly available statistics consistently show high housing population density across the region (from 6.1 in Halls Creek to 6.7 in Broome) [26]. Aspects of social mobility and transience among Aboriginal people for cultural and kinship reasons are poorly understood by non-Aboriginal people [27-30]. Examples brought to our attention by the ARG included the entire abandonment of houses in one small community after the suicide of a young person. All those who left their homes needed to find a place to live with family and friends already living in crowded conditions. Other social and cultural events including rodeos, races, lore organised through Kimberley Aboriginal Law and Cultural Centre (KALACC), unique place-based festivals such as Shinju Matsuri in Broome (www.shinjumatsuri.com.au) or Mowanjum (www.mowanjumarts.com/festival) and anniversary meetings involve large movements of people across and beyond the Kimberley. Although we are confident that tacit knowledge of the requisite preparations to mitigate public health risks of such events is extensive, there are as yet no codified procedure or best practice guideline written from a public health perspective about how remote communities, organisers and local environmental health services might best prepare for such events. Community conflicts will also precipitate people movements as families might choose to relocate temporarily from tense situations.
Box 1 Themes emerging from ARG consultations
Awareness of mumps as a disease and outbreak actions
- ARG members perceived that many Aboriginal people knew what mumps was (“big lump in the neck”), some recalled being sick as a child and others had been recently informed during the public health response and circulated health promotion materials. Interviews discovered accurate knowledge of transmission: catching it ‘from sharing, sneezing, coughing’ or ‘sharing drinks and smokes’ although others stated: ‘don’t know how you get it’.
- Behaviours to reduce transmission were known but difficult to implement in a ‘sharing’ community where food and cigarettes are shared. It was seen that confining individuals to home was generally not feasible as visitors were frequent: ‘can’t stop people from going to gatherings-they have to go”, “You can’t say no” “You gotta share-very hard to tell em”
- Not sharing or isolating children could offend people as these actions were not part of cultural norms.
Importance of education and consistent outbreak messages expressed in a jargon-free way
- High rates of routine immunisation were seen as a good thing but the quality of messages during the outbreak needed to be improved: ‘You have to give people the information” “they need the information to be explained in a way they can understand”,’ or ‘Keep educating and explaining how you catch it-people will get the message eventually’
- Community meetings during outbreaks were encouraged by the ARG for future public health messages: ‘talk to young mother’s groups, talk to young mothers’; ‘put notices around at office, shop, Centrelink, men’s group’; ‘talk to the school, get messages home through kids, teach kids about hand washing, sneezing into their arm’
- It was emphasised that clinic staff already well-known to the community should be visible and provide health promotion sessions with teachers and education assistants: ‘If you are part of the community people know you and trust you-they will listen’
- Using family strengths was recommended: ‘get family groups together’
- Use of Aboriginal organisations to get messages out to the wider community and use of Facebook or community radio was acknowledged as very effective in remote communities to share news and key health messages.
- The ARG emphasised the importance of ‘face to face’ contact with people using ‘grass-level’ language especially through known local staff including environmental health workers located in communities: ‘make sure the people you are working with have all the info and facts because they can spread the word around the community’ and ‘using the local mob from around here makes it easier’
- The ARG emphasised the need for very early communications: ‘if you have more warning go in and talk to communities before any public health action’.
- The ARG also identified the importance of ‘back room consultations’ in which local people themselves discussed and ‘translated’ to each other the meaning of highly complex health information originally delivered by a professionally qualified health professional to a parent or carer. The ARG suggested the need for ‘cultural brokers’ in every community to act as the ‘go-between’ and to translate information into local language or more easily understood vernacular
- Recommended resources to use for public health action included posters, pictures, cartoons and not using ‘too many words or high English-a lot of people can’t read’; more pictures for kids and old people.
- The importance of target groups to give specific information to was emphasised – as was the importance of repeated advice in the context of a continuous relationship. High rates of health staff ‘churn’ and the disadvantages of new faces and new people affected outbreak management on the ground.
Other key learnings from ARG members
- Improve communication between health and non-health related agencies servicing Aboriginal remote areas including intersectoral meetings with government, Aboriginal Medical Services and NGOs with untapped potential to contribute such as bus patrols like Kullari Patrol in Broome. (http://mama.org.au/kularri-patrol-services/),Prescribed Body Corporates (PBCs), Cultural and Language centres, Ranger Groups, Land Councils, and Traditional Owner Groups such as Yawuru.
- Discuss relevant information with people at large gatherings or prior to these gatherings
- Work with Aboriginal organisations and groups to effectively distribute culturally appropriate information and advice
- Find out when large gatherings are occurring and warn people in advance.
- Use local Aboriginal people to help with identifying culturally appropriate material/resources (Rangers, local clinic employees, community councils etc.)
- Recognise that communities are similar but not the same, so what may work in one may not work in another.
- Increase school talks for children/teachers/parents/caregivers regarding health issues.
- Increase involvement of environmental health services
Discussion and recommendations
Across the Kimberley, there are approximately 200 remote Aboriginal communities ranging in size from small family-based communities to others as large as 600 to 1,000 people [31]. In addition, there are five large towns in which there are residential areas with conventional suburban layouts where larger numbers of Aboriginal people typically live, namely Broome, Derby, Fitzroy Crossing, Halls Creek and Kununurra. We advocate investing in local collaborations which are sustained, respected and reliable in the urgency of an outbreak. Such a strengths-based approach would shift responsibility for health outcomes more directly to communities who are re-empowered and better supported. Features of modern Aboriginal life represent strength for culture, community engagement and future public health action. Comprehensive PHC is uniquely placed to nurture these features [32]. Once charged with responsibility for supporting local social and environmental infrastructure, PHC could facilitate the necessary meetings and discussions to produce strong and local community partnerships with service providers. ‘Outbreak templates’ could be discussed in advance through these meetings, explaining essential steps before, during and after an outbreak. We are particularly attracted to the concept of appropriately remunerated ‘community health consultants’ who are resourceful Aboriginal people and respected in each community, able to transfer health knowledge and mobilise health action. Over time, their influence and impact would raise health knowledge and re-empower communities so that ‘third world’ diseases would no longer afflict remote Aboriginal communities. Such ideas should be further co-designed with Aboriginal people such as this ARG.
By taking a deliberate step to share outbreak data with an ARG before report-writing, this project has set a precedent for collaborative debriefing of an outbreak response. Nearly half of the resident population in the Kimberley is Aboriginal [31]. In New Zealand, a Treaty of Waitangi-based framework for health promotion emphasizes governance, control and equality in outbreak management [16]. While recognising many differences between Australia and New Zealand with respect to their respective Indigenous peoples, the principle of cultural safety in outbreak management is universal [16]. A proactive public health outbreak response should begin with the foresight that an infectious disease will transmit quickly because of the continual travel of Aboriginal people and deeply entrenched cultural mores to share food, shelter and transport. Finally, it is difficult to conclude otherwise that the impact of government policies and decisions that are made without consultation and participation in the decision-making by Aboriginal people has had an impact on their health and wellbeing, increasing their risk of communicable disease. Contemporary examples brought to our attention included outsourcing of community and housing repairs, development and imposition without adequate consultation of public policy decisions about housing access and abolition of Community Development Employment Projects (CDEP) which had otherwise provided communities with workforce and resources to address local priorities. Contributing to overcrowding in houses poorly designed and in disrepair, these examples largely outside of community control created circumstances rife for exposure to communicable disease.
Acknowledgments
All authors acknowledge Aboriginal elders past and present, and emerging Aboriginal leaders, future descendants and the continuing relationship of Aboriginal people to the country and its waters. We acknowledge that these lands were never ceded to Europeans and that ancient jurisdictions survive. We also acknowledge that the benefits now enjoyed by some as a result of European colonisation of the continent of Australia have been at the expense of incalculable suffering to others. By forging stronger and more respectful partnerships with Australia’s First Peoples, we look forward to contributing to a better nation. Culture is compass. We thank Dr Kerr Wright and Martin Cutter from the Kimberley Aboriginal Medical Services (KAMS) and Dr Gary Dowse and his team at CDCD in Perth for support.
References
- Massey PD, Pearce G, Taylor KA, Orcher L, Saggers S, Durrheim DN. Reducing the risk of pandemic influenza in Aboriginal communities. Rural and Remote Health 2009; 9: 1290
- Quinn EK, Massey P, Speare R. Communicable diseases in rural and remote Australia: the need for improved understanding and action. Rural and Remote Health 2015: 15: 3371. Published online 21 September 2015
- Naidu L, Chiu C, Habig A, Lowbridge C, Jayasinghe S, Wang H, McIntyre P, Menzies R. Vaccine preventable diseases and vaccination coverage in Aboriginal and Torres Strait Islander people, Australia 2006-2010: Mumps. Communicable Diseases Intelligence Quarterly Report 2013: 37 Suppl: S23-S26
- Bag S, Dey A, Wang H, Beard F. Australian vaccine preventable disease epidemiological review series: Mumps 2008-2012. Commun Dis Intell 2015;39 (1):E10–E18.
- Dey A, Knox S, Wang H, Beard F, McIntyre F. Summary of national surveillance data on vaccine preventable diseases in Australia 2008-2011. Communicable Diseases Intelligence 2016; 40 Supplement: S30-S32
- Bangor-Jones RD, Dowse GK, Giele CM, van Buynder PG, Hodge MM, Whitty MM. A prolonged mumps outbreak among highly vaccinated Aboriginal people in the Kimberley region of Western Australia. Medical Journal of Australia 2009; 191: 398–401
- Ladbury G, Ostendorf S, Waegemaekers T, van Binnendijk, R, Boot H, Hahné S. Smoking and older age associated with mumps in an outbreak in a group of highlyvaccinated individuals attending a youth club party, the Netherlands, 2012. Euro Surveill 2014;19(16):20776.. Available from: http://www.eurosurveillance.org
- Savage E, Ramsay M, White J, Beard S, Lawson H, Hunjan R, et al. Mumps outbreaks across England and Wales in 2004:observational study. BMJ 2005;330(7500):1119-20. DOI:10.1136/bmj.330.7500.1119 PMID: 15891227
- Eriksen J, Davidkin I, Kafatos G, Andrews N, Barbara C, Cohen D, et al. Seroepidemiology of mumps in Europe (1996-2008): why do outbreaks occur in highly vaccinated populations? Epidemiol Infect 2013;141(3):651-66. DOI: 10.1017/S0950268812001136 PMID: 22687578
- Marin M, Quinlisk P, Shimabukuro T, Sawhney C, Brown C, Lebaron CW. Mumps vaccination coverage and vaccine effectiveness in a large outbreak among college students–Iowa, 2006.Vaccine 2008; 26(29-30):3601-7. DOI: 10.1016/j.vaccine.2008.04.075 PMID: 18539365
- Cordeiro, E., Ferreira,M., Rodrigues, F., Palminha, P., Vinagre, E., and Pimentel, J.P. (2015). Mumps outbreak among highly vaccinated teenagers and children in the Central Region of Portugal, 2012-2013. Acta Medica Portuguesa. 28, 435–441. doi: 10.20344/amp.5756
- Park SH. Resurgence of mumps in Korea. Infect Chemother. 2015 Mar;47(1):1-11. doi: 10.3947/ic.2015.47.1.1. Epub 2015 Mar 30
- Vygen S, Fischer A, Meurice L, Mounchetrou Njoya I, Gregoris M, Ndiaye B, Ghenassia A, Poujol I, Stahl JP, Antona D, Le Strat Y, Levy-Bruhl D, Rolland P. Waning immunity against mumps in vaccinated young adults, France 2013. Euro Surveill 2016; 21(10):30156. doi: 10.2807/1560-7917.ES.2016.21.10.30156
- NCIRS. Significant events in measles, mumps and rubella vaccination practice in Australia. http://www.ncirs.edu.au/assets/provider_resources/history/Measles-mumps-rubella-history-March-2016.pdf
- Western Australian Immunisation Strategy 2016–2020. Government of Western Australia. http://ww2.health.wa.gov.au/~/media/Files/Corporate/general%20documents/Immunisation/PDF/wa_immunisation_strategy_2016-2020.pdf
- IESR. Guidelines for the Investigation and Control of Disease Outbreaks. Porirua, New Zealand. Updated 2011
- Ogbuanu I, Kutty P, Hudson J et al. Impact of a third dose of measles-mumps-rubella vaccine on a mumps outbreak. Pediatrics 2012; 130 (6): e1567-e1574
- Communicable Disease Control Directorate (CDCD) Surveillance case Definitions for Notifiable Infectious Diseases and Related Conditions in Western Australia. (2013)
- Préaud M. Country, Law & Culture: Anthropology of Indigenous Networks from the Kimberley. Doctoral thesis submitted March 2009 available at: https://researchonline.jcu.edu.au/11819/
- Préaud M. Foundation and continuity: Kimberley Aboriginal geopolitics, in Australian Aboriginal Anthropology Today: Critical Perspectives from Europe 2014 [En ligne], mis en ligne le 13 juin 2014, Consulté le 27 septembre 2017. URL : http://actesbranly.revues.org/555
- Slater L. ‘Calling our Spirits Home’: Indigenous Cultural Festivals and the Making of a Good life. Cultural Studies Review 2010; 16 (1): http://epress.lib.uts.edu.au/journals/index.php/csrj/index
- Westphal D. Epidemiology and vaccine effectiveness during a large mumps outbreak in Western Australia. ESPID eLearning. Westphal D. May 12, 2016; 134425 http://espid.multilearning.com/espid/2016/34th/134425/darren.westphal.epidemiology.and.vaccine.effectiveness.during.a.large.mumps.html
- Kutty PK1, McLean HQ, Lawler J, Schulte C, Hudson JM, Blog D, Wallace G Risk factors for transmission of mumps in a highly vaccinated population in Orange County, NY, 2009-2010. Pediatr Infect Dis J 2014 Feb;33(2):121-5. doi: 10.1097/INF.0000000000000020.
- Livingston KA, Rosen JB, Zucker JR, Zimmerman CM.Mumps vaccine effectiveness and risk factors for disease in households during an outbreak in New York City. Vaccine 2014 Jan 9;32(3):369-74. doi: 10.1016/j.vaccine.2013.11.021. Epub 2013 Nov 16.
- Centers for Disease Control and Prevention (CDC). Manual for the Surveillance of Vaccine-Preventable Diseases: Chapter 9-1 Mumps. 5th edition. CDC, Georgia: 2012
- Environmental Health Needs Coordinating Committee (EHNS). Environmental Health Needs of Aboriginal Communities in Western Australia: The 2008 Survey and its Findings [Internet]. Perth (AUST): Western Australian Department of Health; 2008 [cited 2017; 19 November]. Available from: http://www.public.health.wa.gov.au/2/121/1/reports.
- Memmott P, Long S, Bell M et al. Between places: Indigenous mobility in remote and rural Australia. AHURI Positioning Paper 81 / 2004. University of Queensland.
- Prout S. On the move? Indigenous temporary mobility practices in Australia. CAEPR Working Paper 48 / 2008: ANU, Canberra
- Prout S, Yap M. Indigenous temporary mobilities and service delivery in regional service centres: A West Kimberley case study. CAEPR Working Paper 66 / 2010: ANU, Canberra
- Scott K. Not so easy: language for a shared history. In Griffith Review 2015; 47: Looking West. 200-214
- WA Government. Regional services reform Unit. Resilient families, Strong Communities: Key Insights from Consultations with remote Aboriginal communities in Western Australia.2016 http://regionalservicesreform.wa.gov.au/sites/regionalservicesreform.wa.gov.au/files/docs/RESOURCES/RSRU_Consultation%20Report.pdf?bcsi_scan_c221d61a0ea4ff4c=OY6XnnJUThzep42qQeahTvfrXOECAAAA4cK+FQ==&bcsi_scan_filename=RSRU_Consultation%20Report.pdf
- Davy, C., Cass, A., Brady, J., De Vries, J., Fewquandie, B., Ingram, S. et al. Facilitating Engagement through strong relationships between primary healthcare and Aboriginal and Torres Strait Islander peoples. Australian and New Zealand Journal of Public Health 2016; 40 (6): 535-541