Review of nutrition among Aboriginal and Torres Strait Islander people
ReviewLee A, Ride K (2018) Review of nutrition among Aboriginal and Torres Strait Islander people. Australian Indigenous
HealthInfoNet. From http://healthbulletin.org.au/articles/review-of-nutrition-among-aboriginal-and-torres-strait-islander-people
Introduction
About this review
Acknowledgements
Key facts
The context of Aboriginal and Torres Strait Islander nutrition
Australian dietary guidelines
Nutrition in pregnancy and the early years
Adult and community nutrition
Food security
Costs of poor diet and nutrition
Nutrition programs and services
Aboriginal and Torres Strait Islander nutrition workforce
Policies and strategies
Future directions
Concluding comments
Appendix 1. The Australian Dietary Guidelines
Appendix 2. The Aboriginal and Torres Strait Islander Guide to Healthy Eating
Appendix 3: Data sources and limitations
References
View PDF version (996 KB)
Introduction
The United Nations General Assembly has proclaimed a Decade of Action on Nutrition from 2016 to 2025 in recognition of the need to eradicate hunger and prevent all forms of malnutrition, including under-nutrition and over-nutrition, worldwide [2]. The Global nutrition report provides context for nutrition issues internationally and in Australia, including those of Aboriginal and Torres Strait Islanders [5].
Aboriginal and Torres Strait Islander people continue to suffer the worst health of all population groups in Australia, with a high burden of disease and low life expectancy [6-9]. The latest available estimates of life expectancy, released in 2013, show that the gap between Aboriginal and Torres Strait Islander and non- Indigenous Australians remains high at 10.6 years for men and 9.5 years for women [10]. A relatively large proportion of Aboriginal and Torres Strait Islander deaths are premature; during the 5-year period 2009–2013, around 81% of deaths among Aboriginal and Torres Strait Islander people occurred before the age of 75 years, compared with 34% of deaths for non-Indigenous people [6].
Poor nutrition is an important factor contributing to overweight and obesity, malnutrition, cardiovascular disease, type 2 diabetes, and tooth decay [11, 12]. Chronic diseases – such as cardiovascular disease, type 2 diabetes, chronic kidney disease and some cancers- are responsible for at least 75% of the mortality gap between Aboriginal and Torres Strait Islander and other Australians [8]. For example, Aboriginal and Torres Strait Islander people are 1.6 times more likely to die from cardiovascular disease and 3-4 times more likely to die from type 2 diabetes than other Australians. Yet these diseases are potentially preventable by modifying risk factors such as being overweight and obese, cigarette smoking, physical inactivity and poor nutrition [6, 10, 13]. Five of the seven leading risk factors contributing to the health gap between Aboriginal and Torres Strait Islander and non-Indigenous Australians – obesity, high blood cholesterol, alcohol, high blood pressure, and low fruit and vegetable intake – relate to poor diet [7]. Combined dietary factors contribute the greatest proportion (27.4%) of all risk factors assessed [7].
Poor diet and nutritional status of Aboriginal and Torres Strait Islander people are influenced by many factors, such as socio- economic disadvantage, and geographical, environmental, and social factors [11, 12].
Very few Aboriginal and Torres Strait Islander people meet dietary recommendations for intake of healthy foods [11, 14]. Also, 41% of their daily energy intake is derived from unhealthy ‘discretionary’ foods and drinks that are high in saturated fat, added sugar, salt and/or alcohol (‘junk’ foods), compared to 35% among non- Indigenous Australians [14-16].
The current poor nutritional health of Aboriginal and Torres Strait Islander people is in marked contrast to the situation prior to European settlement in Australia, when Aboriginal and Torres Strait Islander peoples were generally healthy and enjoyed a varied traditional diet low in energy density and rich in nutrients [12, 17].
About this review
The purpose of this review is to provide a comprehensive synthesis of key information on diet and nutrition among Aboriginal and Torres Strait Islander people in Australia to: (1) inform those involved or interested in Aboriginal and Torres Strait Islander health and nutrition; and (2) provide the evidence for those involved in policy, strategy and program development and delivery. The review provides general information on the historical, social and cultural context of nutrition, and the environmental and behavioural factors that contribute to poor diet and nutrition among Aboriginal and Torres Strait Islander people.
It provides detailed information on food, diet and nutritional health among Aboriginal and Torres Strait Islander people, and links to incidence and prevalence data of diet-related conditions; morbidity, mortality and burden of disease. This review highlights the importance of nutrition promotion and the prevention of diet- related disease, and provides information on relevant programs, services, policies and strategies that help improve food supply, diet and nutritional health among Aboriginal and Torres Strait Islander people. It concludes by discussing possible future directions for combatting the growing epidemic of diet-related ill health among Aboriginal and Torres Strait Islander people in Australia.
This review draws mostly on journal publications, government reports, national data collections and national surveys, the majority of which can be accessed through the HealthInfoNet’s Bibliography.
Edith Cowan University prefers to use the term ‘Aboriginal and Torres Strait Islander’ rather than ‘Indigenous Australian’ for its publications. However, when referencing information from other sources, our authors are ethically bound to utilise the terms from the original source unless they can obtain clarification from the report authors/copyright holders. As a result, readers may see these terms used interchangeably with the term ‘Indigenous’ in some instances. If they have any concerns they are advised to contact the HealthInfoNet for further information.
Acknowledgements
Special thanks are extended to:
- authors of relevant reviews published previously by the Australian Indigenous HealthInfoNet, particularly Dr Neil Thomson, Jennifer Brown and Sharon Thorpe, whose work has informed this current revision
- the anonymous reviewer whose comments greatly assisted finalisation of this review
- other staff at the Australian Indigenous HealthInfoNet for their assistance and support
- the Australian Government Department of Health for their ongoing support of the work of the Australian Indigenous HealthInfoNet.
Key facts
- Aboriginal and Torres Strait Islander people continue to suffer the worst diet-related health of all population groups in Australia.
- Diet-related chronic diseases – such as cardiovascular disease, type 2 diabetes, chronic kidney disease and some cancers – are responsible for at least 75% of the mortality gap between Aboriginal and Torres Strait Islanders and other Australians.
- In 2011, 13 dietary factors were identified as being risk factors for the Australian population (out of 29 risk factors). When combined, the joint effect of all dietary risks combined contributed 9.7% to the burden of disease for Aboriginal and Torres Strait Islander people.
- The nutrition burden among Aboriginal and Torres Strait Islander adults is underscored by malnutrition, which includes both over-nutrition (particularly over-consumption of unhealthy ‘discretionary’ foods) and under-nutrition (dietary deficiencies related to inadequate intake of healthy foods).
- In 2012-13, very few Aboriginal and Torres Strait Islander adults or children consumed adequate amounts of healthy foods consistent with recommendations of the Australian Dietary Guidelines. Furthermore, over two-fifths (41%) of total daily energy reported by Aboriginal and Torres Strait Islander people came from unhealthy foods and drinks classified as ‘discretionary’.
- The current situation is in marked contrast to the situation prior to European settlement of Australia. All available evidence suggests that Aboriginal and Torres Strait Islander Australians were traditionally healthy; enjoying varied dietary patterns of fresh plant and animal foods, low in energy density and rich in nutrients.
- Many historical, socioeconomic, environmental and geographic factors contribute to the current poor diet, nutrition and food security experienced by Aboriginal and Torres Strait Islander people.
- In 2012-13, 66% of Aboriginal and Torres Strait Islander people aged 15 years or older were classified as overweight (29%) or obese (37%); a further 30% were normal weight and 4% were underweight. In addition, 30% of Aboriginal and Torres Strait Islander children aged 2-14 years were overweight (20%) or obese (10%); 62% were in the normal weight range and 8% were underweight.
- Prevalence of poor pregnancy outcomes and infant malnutrition remains high in many areas. Low birthweight, failure to thrive and poor child growth are still serious concerns in many Aboriginal and Torres Strait Islander communities.
- In 2012-13, 83% of Aboriginal and Torres Strait Islander children aged 0-3 years had been breastfed, compared with 93% of non-Indigenous children. Of those who were breastfed, Aboriginal and Torres Strait Islander infants were less likely than non-Indigenous infants to have been breastfed for 12 months or more (12% compared with 21%).
- Based on self-reported usual serves of vegetables eaten per day, only 8% of Aboriginal and Torres Strait Islander people met the vegetable intake recommended in the Australian Dietary Guidelines. Mean reported vegetable intake was less than a third of the recommended amount.
- Based on self-reported usual serves of fruit eaten per day, 54% of Aboriginal and Torres Strait Islander people met the fruit intake recommended in the Australian Dietary Guidelines. Mean reported fruit intake was around half the recommended amount.
- One-quarter (25%) of grain (cereal) foods consumed by Aboriginal and Torres Strait Islander people were from wholegrain and/or high fibre varieties, compared to the recommended 50% or more.
- The average daily consumption of milk, yoghurt, cheese and alternatives for each age-sex group of Aboriginal and Torres Strait Islander people, with the exception of children aged 2-3 years and girls 4-8 years, was considerably lower than the respective recommend number of serves.
- The average daily consumption of lean meats and meat alternatives for each age-sex group of Aboriginal and Torres Strait Islander people, with the exception of girls 2-3 years, was less than the respective recommendations; intake was relatively high in remote areas.
- On average, Aboriginal and Torres Strait Islander people 2 years and over reported consuming an average of 75g (18 teaspoons) of free sugars per day, which equates to an average of 14% of dietary energy, nearly 50% more than World Health Organization (WHO) recommendations. Two-thirds of Aboriginal and Torres Strait Islander people’s free sugar intake came from sugary drinks.
- In 2011-2013, 22% of survey respondents said they had run out of food and couldn’t afford to buy more in the last 12 months. Aboriginal and Torres Strait Islander people in remote areas were more likely to run out of food than those in non- remote areas (31% and 20% respectively).
- The underlying causes of food insecurity in Aboriginal and Torres Strait Islander communities include factors such as low income and unemployment, inadequate housing, over- crowding, lack of educational opportunities, transport, high food costs, cultural food values, food and nutrition literacy, knowledge and skills.
- A range of general Australian Government Department of Health programs contribute to the prevention and management of diet-related disorders among Aboriginal and Torres Strait Islanders at a national level. However, since the expiry of the National Aboriginal and Torres Strait Islander nutrition strategy and action plan 2002-2010, there has been no national coordination of nutrition efforts in Australia.
- Several community-based nutrition programs have demonstrated positive outcomes in the past. The most effective programs have adopted a multi-strategy approach, addressing both food supply (availability, accessibility and affordability of foods) and demand for healthy foods. A major success factor is community involvement in (and, ideally, control of) all stages of program initiation, development, implementation and evaluation, to ensure the intervention is culturally appropriate and tailored to community needs.
- Programs to improve food supply have included a focus on: food retail outlets; local food production, such as school or community gardens; food provided by Aboriginal and Torres Strait Islander and community organisations; and food aid. Community store nutrition policies have been shown to be important influences on the food supply and dietary intake in remote areas.
- While nutrition education alone will not improve food security or dietary intake, it can be effective when combined with a range of other strategies to help people access healthy food, such as cooking programs, peer education, budgeting advice, and group-based lifestyle modification programs.
- A well-supported, resourced and educated Aboriginal and Torres Strait Islander nutrition workforce is essential for the success of nutrition interventions.
- There is a long history of effort to improve nutrition and food security among Aboriginal and Torres Strait Islander people, however there is no current national nutrition policy or strategy in place.
- Improving food supply and security to better prevent and manage poor nutrition and diet-related disease is vital to the current and future health of Aboriginal and Torres Strait Islander Australians. Food and nutrition programs play an important role in the holistic approach to improving health outcomes for Aboriginal and Torres Strait Islander people.
The context of Aboriginal and Torres Strait Islander nutrition
It is beyond the scope of this review to discuss in detail the underlying social and cultural determinants that influence the nutritional status of Aboriginal and Torres Strait Islander people. However many historical, socioeconomic, environmental and geographic factors contribute to the poor diet, nutrition and food insecurity currently experienced by Aboriginal and Torres Strait Islander people. Among these are: lower incomes; lower educational opportunities and attainment; higher rates of unemployment; disruption to family structures; poorer access to a healthy and affordable food supply; poorer access to health infrastructure, such as adequate housing, compared to the broader Australian community [11].
It has been estimated that between one-third and one-half of the health gaps between Aboriginal and Torres Strait Islanders and non-Indigenous Australians are associated with differences in socioeconomic position [8]. In particular, Aboriginal and Torres Strait Islander people suffer substantial disadvantage across a range of social determinants that underpin poor nutritional health status [11, 12, 18]. Among these are: lack of control over circumstances; poverty; lower income and unemployment; lower levels of education; disrupted family and community cohesion; social marginalisation; stress; substance abuse; inadequate and overcrowded housing; inadequate sanitation, water supplies and hygiene; limited access to transport; and incarceration, discrimination and racism.
Historical factors
Many historical factors continue to impact on the diets of Aboriginal and Torres Strait Islander people today. Although European settlement severely affected the retention of knowledge, access to, and use of traditional foods [12, 19], strong culture, values and a connection to the land contribute to the resilience of Aboriginal and Torres Strait Islander peoples today.
Traditional diet and health
Aboriginal people first arrived in Australia at least 50,000 years ago, with recent genetic evidence suggesting dates as early as 75,000 years ago, making Aboriginal Australians one of the oldest continuous populations living outside of Africa [20]. Hunter- gatherer life was usual until about 12,000 years ago, when human groups, including in Australia, started to experiment with plant production [21].
Aboriginal people had a strikingly detailed knowledge of their country, including the availability of water, and the impact of the annual cycle of seasonal changes on availability and lifecycle of particular plant and animal foods [12, 22-24]. Diets were omnivorous and could vary greatly from day-to-day and season- to-season. In many parts of the country, dietary patterns tended to be subsistence with occasional feasts, sometimes referred as ‘feast and famine’. The capacity to devour large quantities during abundance was an important survival strategy, along with minimizing ‘unnecessary’ energy expenditure, enabling excess energy to be stored as fat to help people survive times of food shortage [12, 24, 25].
Traditional Torres Strait Islander diets varied from island to island. Seafoods such as fish and shellfish were an important component of the diet, and turtle and dugong had a central place in cultural life, as did the keeping of pigs. Gardening was vital, not only for subsistence but to provide food for ceremonies and trade. Traditional crops included taro, yams, bananas and coconuts. Several plant foods were stored and preserved [12, 25].
Men and women both contributed importantly to food procurement. Women generally provided the subsistence diet: diverse plant foods, honey, eggs, small mammals, reptiles, fish, shellfish, crustaceans and insects. They usually obtained foods in groups with their children — passing on knowledge and skills to the next generation while the men tended to hunt for larger game (such as kangaroo, wallaby, emu, turtle, crocodile and dugong). It has been claimed that hunter-gatherers spent less time (three to five hours/day) ensuring their livelihood than agriculturalists and the full-time employed today, however food procurement and preparation was very energy-intensive [12, 24].
Animal foods:
All animals were potential food sources; mammals, birds, reptiles, insects and all marine species. Everything edible on an animal carcass was eaten and bones were chewed. One of the most striking features of wild animals is their leanness in comparison with meats from animals domesticated for human consumption; the fat in wild animals tends to be less saturated too [12, 24].
Plant foods:
Traditionally Aboriginal people consumed a very wide range of wild plant foods: tuberous roots, legumes, seeds (including wild rice), nuts, fruits, berries, nectars, flowers, gums, and lerp 1. Relative to their cultivated forms, wild plants tend to be high in dietary fibre and contain carbohydrate that is slowly digested, low in starch and sugars, and rich in many bioactive phytochemicals (e.g. flavonoids, polyphenols) with antioxidant and anti-inflammatory properties [12, 24].
Food preparation and patterns of intake:
Traditional food preparation generally resulted in minimal loss of nutrients. Many plant foods, such as fruits, bulbs, gums, flowers and nectars were consumed fresh and raw as they were collected. Foods were processed to help make them more digestible or palatable, for example, baking starchy tubers, grinding and roasting seeds and cooking meat. The most highly prized components of the traditional diet were the relatively few energy-dense foods high in fat or sugar, including land and marine animal fat, bone marrow, organ meats, eggs, fatty insects and honey. Food was usually eaten when it was available, with little wastage [12, 24].
Infant feeding:
Traditionally children were universally breastfed until they were about three to four years old. If the need arose, other lactating women would substitute for the mother. The age of weaning often depended on the arrival of a younger sibling [12, 26]. Young children were usually fed breastmilk and food on demand [12].
Health:
Traditional foods promoted physical health as well as cultural, spiritual and emotional health. Available information on the nutrition of Aboriginal and Torres Strait Islander people prior to European colonisation indicates that they were extremely lean, physically fit and strong [21-23, 27, 28]. In the most remote areas of Australia small groups continued to live as hunter-gatherers well into the 20th century; studies with these groups show they exhibit no evidence of the chronic diseases that plague others today [29]. For more information, see Box 1.
Box 1: Traditional foods and the benefits of a hunter-gatherer lifestyle
In remote Australia, many older Aboriginal people retain the knowledge and ability to live as hunter-gatherers. The health benefits of temporary reversion to traditional hunter gatherer life were illustrated by a small group of diabetic people in the West Kimberley in the early 1980s [1]. Among the dramatic health improvements seen, after only seven weeks “living off the land” in their traditional country they lost weight and their metabolic indicators and risk factors for diabetes and cardiovascular disease normalised. People rarely complained of hunger; although their diet was low in energy (1200 kcal/day) it was high in protein (54% energy), with 33% carbohydrate, and 13% fat. While reverting to a hunter-gatherer lifestyle is not a realistic option for the vast majority of Aboriginal and Torres Strait Islander people who live in towns and cities today, in some remote communities people do regularly hunt animal foods and collect plant foods to supplement the foods they buy from the store. The model of the hunter-gatherer diet and lifestyle can be used also as a benchmark, and as a guide to healthier patterns of eating and lifestyle.
Transitional diet post contact
After European settlement in 1788, there was decreased access to and availability of traditional foods, and Aboriginal people were increasingly forced to become dependent on introduced foods [12, 22, 23, 30]. These were primarily‘rations’ of flour, sugar, tea, tobacco and to a lesser extent meat (fresh, tinned or salted). The durability, transportability, low bulk, affordability and the simple cooking and storage facilities required for their preparation may still influence popularity of these foods today.
As hunter-gatherer life, although healthy, could also be very difficult, many Aboriginal people opted to visit or stay on cattle stations, missions and government settlements, where at least some food was provided on a regular basis. The available foods being high in fat and sugar, such as jam, sugar and tinned meat, also tended to reflect the most highly prized traditional foods. In particular, sugar was eagerly sought and was consumed in large quantities from early contact. Basic rations were supplemented with irregular quantities of fruit and vegetables from the local gardens in missions and government settlements, and where possible, with traditional bush food.
Communal dining rooms were established at many settlements and missions and tended to be the only option to obtain food, especially prior to 1969 when Aboriginal and Torres Strait Islander people did not receive all their wages in cash [12]. Communal feeding disrupted traditional food distribution, contributed to the loss of knowledge in food preparation and cooking methods and lessened responsibility for the economic management of food and the feeding of children.
Available dietary studies of Aboriginal people during these times showed low intakes of energy, protein and several micronutrients including calcium, iron, vitamin A, vitamin B12 and vitamin C, reflecting dietary patterns that were higher in flour, bread and poor quality meats, but lower in fruit, vegetables and dairy foods, than for other Australians [12].
Socioeconomic factors
Occupation, income and wealth play important roles in socioeconomic position, and also in health. Higher incomes support greater access to goods and services that provide health benefits, such as better food and housing, health care options, and preventative health activities. Loss of income through illness, disability or injury can adversely affect individual socioeconomic position and health [10].
The 2012-2013 Australian Aboriginal and Torres Strait Islander health survey (AATSIHS) examined associations between ‘dietary behaviour’ and employment status [31]. Reported fruit and vegetable intake were used as a proxy for dietary behaviour.
After age-adjustment, unemployed Aboriginal and Torres Strait Islander people were more likely to have an inadequate daily fruit intake (63%) and inadequate vegetable intake (98%) than those who were employed (54% and 94% respectively) or not in the labour force (60% and 95% respectively).
Aboriginal and Torres Strait Islander households have, on average, a weekly gross income which is $250 less than that of non- Indigenous households [6]. In the 2014-15 National Aboriginal and Torres Strait Islander social survey (NATSISS), the unemployment rate for Aboriginal and Torres Strait Islander people aged 15 years and over was 20.6%, much higher than the 12.7% for Australians as a whole [32].
Aboriginal and Torres Strait Islanders who are unemployed suffer greater risk of poor health through poor diet – such as lower levels of fruit and vegetable consumption – as well as higher rates of smoking and substance use compared with Aboriginal and Torres Strait Islanders who are employed [10]. However, there tends to be a higher prevalence of overweight and obesity among employed Aboriginal and Torres Strait Islander adults compared to those who are unemployed [10].
Educational attainment is associated with better health throughout life. The 2012-2013 AATSIHS examined associations between dietary behaviour and educational attainment [31]. Aboriginal and Torres Strait Islander people who had completed year 10 or below were more likely to consume inadequate amounts of fruit (59%) and vegetables (95%) than those who had completed year 12 or higher (54% and 93% respectively).
Affordability of healthy diets is affected by both household income and food prices. Purchasing a healthy diet is estimated to cost 20-31% of the disposable household income of low income families, compared with 14-18% for those on a median disposable income [33-35]. Food affordability is lowest in remote Aboriginal and Torres Strait Islander communities, as food prices are higher in remote locations than in urban areas, yet median income is lower in remote areas.
Since the early 1990s, surveys of the cost of a basket of foods have consistently shown that prices in remote Aboriginal and Torres Strait Islander communities are up to 50% more expensive than in the nearest capital cities [36]. There are also fewer opportunities to purchase advertised foods at discounted prices in remote areas [37, 38].
In remote Aboriginal communities, foods of relatively high energy density (such as oil and flour) tend to be cheaper per unit of energy than nutrient dense foods (such as most fruit and vegetables) [37], but are not always cheaper when price is assessed by nutrient density or by other units, such as weight [39]. Purchase of other items (such as cigarettes and alcohol) can also impact on the food budget [6].The exemption of 10% goods and services tax (GST) from basic, healthy foods in Australia helps to increase the affordability of healthy diets, especially among low socioeconomic households [34, 40].
Environmental factors
The physical environment in which many Aboriginal and Torres Strait Islanders live also has significant implications for nutritional status [6, 12]. The elimination of overcrowding and the provision of appropriately designed, constructed and maintained houses are essential for the safe storage, preparation and consumption of food [38]. Access to water for drinking and washing, and safe sewage and garbage disposal are critical to health [41].
According to the Australian Institute of Health and Welfare (AIHW) analysis of the 2012-13 AATSIHS, 15% of Aboriginal and Torres Strait Islander households reported living in a dwelling that was lacking at least one working facility such as a fridge or cooking facility, toilet, bath or shower [6]. In Aboriginal communities across Australia only 6% of houses have all of the functioning health hardware needed to store, prepare and cook food, such as cupboards, bench space, refrigeration and a functioning stove and sink [42].
According to the 2011 census, overcrowding is improving in Aboriginal households but around 13% of Aboriginal and Torres Strait Islander households were overcrowded compared to 3% of other households [6]. Overcrowding impacts around one in five people nationally and more than a third of Aboriginal and Torres Strait Islander people in remote areas [32].
Geographic factors
Although most Aboriginal and Torres Strait Islander people live in metropolitan and regional areas, a much larger proportion live in remote or very remote areas than do non-Indigenous people (21% compared with 2%) [6]. The relatively small proportion of Aboriginal and Torres Strait Islander people who live in remote areas experience 40% of the health gap of Aboriginal and Torres Strait Islander Australians overall [43].
One of the contributing factors is the reduced variety and quality of nutritious foods in remote communities in Australia [44-48]. Healthy food baskets also cost up to 50% more in remote areas than in major cities [36, 46, 49]. It has been estimated that 34-80% of the income of Aboriginal families in remote areas is needed for healthy diets – at least twice that required by non-Indigenous families in urban areas [30, 50]. Factors contributing to the higher costs of foods in rural and remote areas are: increased freight costs; higher store overheads (such as capital costs of building and maintaining long-term storage facilities and accountancy costs); the greater wastage of food stock [46]; some store management practices [47, 51]; and the reduced economies of scale for
purchasing and retailing in small remote communities [44, 52-55]. Healthy food items are less available in remote stores, particularly fresh fruit and vegetables, whole grain cereals, lean meats and low fat dairy products [44-46, 48, 56]. Communities in remote areas may also be without food for extended periods due to weather or road conditions, such as during the wet season, although recent Northern Territory (NT) market basket surveys suggest this may be improving [56].
Australian dietary guidelines
The Australian dietary guidelines [11] are presented in Appendix 1.
Although the Australian dietary guidelines are relevant to Aboriginal and Torres Strait Islander peoples, they also provide specific recommendations for this population group. Specific Aboriginal and Torres Strait Islander dietary recommendations include to enjoy traditional foods whenever possible, and when choosing store foods, to choose those most like traditional bush foods, such as fresh plant foods, wholegrain (cereal) foods, seafood, and lean meats and poultry.
The guidelines note that:
- lactose intolerance after the age of 3–5 years may be problematic in some areas or for some individuals, therefore alternative food sources of calcium are recommended in these cases
- consumption of traditional bush foods should be supported wherever possible
- breastfeeding should be encouraged and supported – the nutritional and immunological benefits of breastfeeding are particularly important in populations with a high prevalence of high risk infants, such as Aboriginal and Torres Strait Islander Australians
- children and adolescents require sufficient nutritious food to grow and develop normally and the growth of young children should be checked regularly.
The World Health Organization (WHO) recommends that both adults and children consume less than 10% of dietary energy from free sugars [57]. This is consistent with the Australian dietary guidelines, as most Australians following the guidelines would consume less than 5% of dietary energy from free sugars [58].
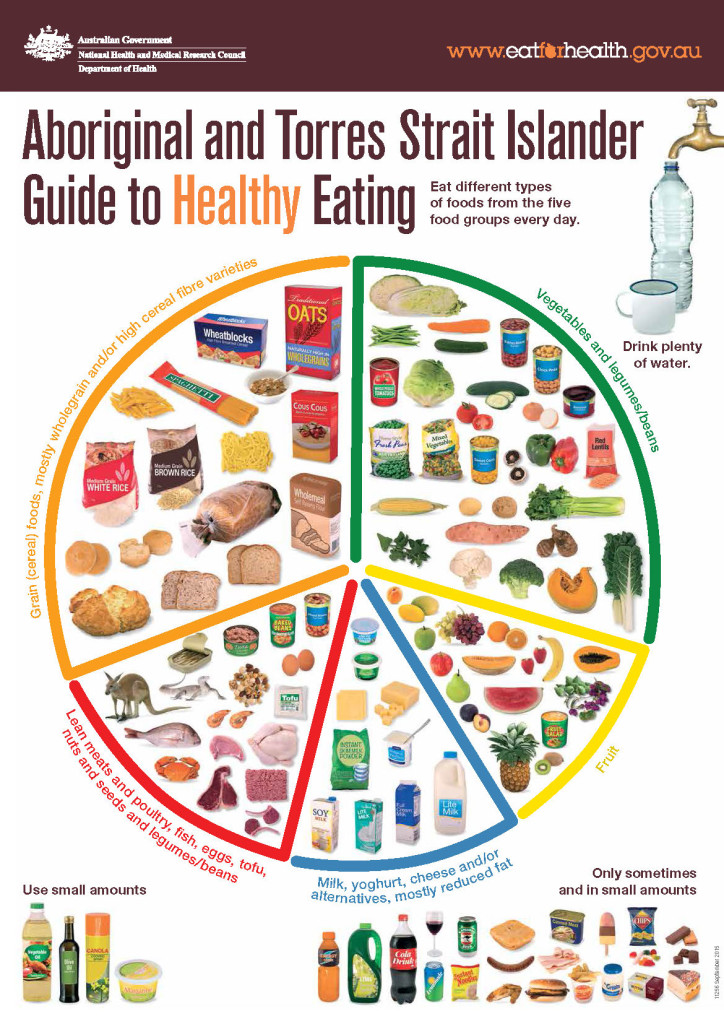
The graphic Aboriginal and Torres Strait Islander guide to healthy eating is included in Appendix 2.
Nutrition in pregnancy and the early years
Good maternal nutrition and healthy infant and childhood growth are fundamental to the achievement and maintenance of health throughout life. The potential intergenerational effects of poor health and nutritional status in early life, including the effect of gestational diabetes, have been well documented; the foundations of adult health are laid in utero and during the perinatal and early childhood periods [59-61].
Maternal and perinatal outcomes of Aboriginal and Torres Strait Islander mothers and their babies have consistently been shown to be poorer than those of non-Indigenous mothers [62]. Key factors include younger maternal age, remoteness and socioeconomic disadvantage.
From 2001 to 2014, the mortality rate for Aboriginal and Torres Strait Islander infants fell from 1,121 deaths per 100,000 births to 638 deaths per 100,000 births, a decrease of 43% [62]. This reflects improvement in the underlying rates of disease, as well as increased health-service utilisation, accessibility and effectiveness. The rate of decrease in mortality for Aboriginal and Torres Strait Islander infants was almost twice that for all infants; however Aboriginal and Torres Strait Islander infant mortality remains almost twice that of non-Indigenous infants [62, 63]. Aboriginal and Torres Strait Islander infant mortality rates vary across jurisdictions, from around six per 1,000 in South Australia (SA), to 13 per 1,000 in the Northern Territory NT [8].
Prevalence of poor pregnancy outcomes and infant malnutrition remains high in many areas and low birthweight, failure to thrive and poor child growth are still serious concerns in many Aboriginal and Torres Strait Islander communities [64]. Iron deficiency anaemia among young Aboriginal and Torres Strait Islander children is also common [12, 65]. For example, a recent clinical audit in Cape York found that 32% of the children aged from 6-24 months were anaemic at their last haemoglobin test [66].
Intra-uterine growth
Good nutrition prior to conception and during pregnancy is crucial, as it influences both the mother’s own health and that of her baby. Low dietary-energy intake, malnutrition, inadequate weight gain during pregnancy, and low pre-pregnancy weight can lead to intra-uterine growth retardation, which in turn can reduce birthweight [59]. Being overweight or obese during pregnancy contributes to an increased risk of complications (particularly for the mother) during pregnancy and delivery, including increased morbidity and mortality for both mother and baby [62]. Other factors that can negatively influence intra-uterine growth include substance use in pregnancy (particularly cigarette smoking and alcohol consumption) [6, 10, 62].
According to the study, Australia’s mothers and babies 2014, pregnant Aboriginal and Torres Strait Islander women were more likely to smoke cigarettes than non-Indigenous pregnant women (46% compared to 12%) [62]. Conversely, fewer Aboriginal and Torres Strait Islander women drink alcohol than non-Indigenous women (71% compared with 77% respectively) [67]. In 2011-12 Aboriginal and Torres Strait Islander women of child bearing age (18-44 years) were less likely to drink at low-risk levels than non-Indigenous women of child bearing age (28.4% compared with 42%), but more likely to drink at risky/high risk levels (11.6% compared with 9.5%) [67]. The prevalence of Fetal alcohol syndrome disorder (FASD) is high among indigenous populations internationally and has significant nutrition implications [68].
Birthweights
Birthweights below 2,500 grams – defined as ‘low birthweight’ – increase the risk of death in infancy and other health problems [6, 10, 62]. Low birthweight may be a result of fetal growth restriction, preterm birth, or a combination of the two [12]. The impact of maternal nutrition on birthweight was demonstrated in a study of 503 infants born to Aboriginal mothers in the Darwin region between 1987 and 1990 [69]. The study found that underweight mothers (with a body mass index (BMI) of less than 18.5)2 had five times the risk of having a low-birthweight baby and over two-and-a-half times the risk of their baby suffering intra-uterine growth retardation. Overall, the study found that 28% of cases of low birthweight and 15% of cases of growth retardation could be attributed to maternal malnutrition.
As discussed previously, many factors other than the nutritional health of the mother can influence birthweight; low birthweight can be considered a proxy indicator of the early start to socioeconomic disadvantage of Aboriginal and Torres Strait Islander children [10].
In 2013, babies born to Aboriginal and Torres Strait Islander mothers were twice as likely to be of low birthweight as babies born to other Australian mothers (12.2% compared with 6.1%) [62]. While the average rate of low birthweight babies born to Aboriginal and Torres Strait Islander mothers decreased slightly from 12.7% in 2000 to 12.2% in 2013 [13, 62, 70], there is wide variation throughout the country. The proportion of low birthweight babies with Aboriginal and Torres Strait Islander mothers has remained between 11.8% and 13.2%, and the proportion of those with non- Indigenous mothers has remained between 5.9% and 6.2% over this time [62].
Breastfeeding
The nutritional and immunological benefits of breastfeeding are particularly important in populations with a high prevalence of high risk infants – such as those of low birthweight or those born to diabetic mothers. Breastfeeding is particularly important in communities that may have limited access to a good quality water supply, limited financial resources and a high prevalence of infectious diseases; it is convenient, hygienic, requires no special equipment, and is significantly cheaper than bottle-feeding [11, 12, 17].
Breast milk is the natural and optimum food for babies and provides all the energy and nutrients that an infant needs for the first six months of life [11, 71]. Breastfeeding promotes sensory and cognitive development and protects the infant against sudden infant death syndrome (SIDS), asthma, infectious diseases and chronic diseases later in life. Exclusive breastfeeding aids a quicker recovery from illness and reduces infant deaths from common childhood illnesses such as diarrhoea or pneumonia. The Australian dietary guidelines recommendation is to ‘encourage, support and promote breastfeeding’. The National Health and Medical Research Council (NHMRC) recommends exclusive breastfeeding for around six months, and breastfeeding, with appropriate complementary foods, until 12 months of age and beyond, as long as the mother and child desire; while breastfeeding is recommended for 6 to 12 months and beyond, any breastfeeding is beneficial to the infant and mother [17]. The WHO recommends exclusive breastfeeding for six months followed by complementary feeding with continued breastfeeding for up to two years or beyond [71]. Breastfeeding contributes to the health of the mother by reducing the risk of ovarian and breast cancers and weight gain in later life [11, 17].
According to the 2012-13 AATSIHS, 83% of Aboriginal and Torres Strait Islander children aged 0–3 years had been breastfed, compared with 93% of non-Indigenous children [6]. Aboriginal and Torres Strait Islander children aged 0–3 years were 2.3 times more likely than non-Indigenous infants to have never been breastfed (17% compared with 7% respectively). Of those who had been breastfed, Aboriginal and Torres Strait Islander infants were more likely than non-Indigenous infants to have been breastfed for less than one month (16% compared with 10% respectively). Aboriginal and Torres Strait Islander infants were less likely than non-Indigenous infants to have been breastfed for 12 months or more (12% compared with 21% respectively). Breastfeeding rates of Aboriginal and Torres Strait Islander children aged 0–3 years did not vary significantly by remoteness, 82% in non-remote areas and 84% in remote areas were breastfed.
Similarly, according to the 2010 Australian national infant feeding survey, breastfeeding initiation levels were similar among Aboriginal and Torres Strait Islander and non-Indigenous mothers (87% and 90% respectively), but levels of exclusive breastfeeding declined more rapidly among Indigenous mothers (derived from [72]). At five months of age only 11% of Aboriginal and Torres Strait Islander babies were exclusively breastfed, compared with 27% of non-Indigenous babies.
A recent study of infant feeding behaviour among Aboriginal women in rural Australia [73] concluded that lack of intergenerational support, unsupportive social factors and the pervasive presence of infant formula produced strong barriers to breastfeeding. Previous studies also cited cracked or sore nipples, tiredness, a mother’s belief that she produces insufficient milk or very low infant birthweight as reasons for not breastfeeding, with similar reasons given among Aboriginal and Torres Strait Islander women as non-Indigenous women [12, 74].
Commencing in 2008-2009, the Footprints in time – the longitudinal study of Indigenous children collects data annually from 11 sites (rural, remote and urban) and up to 1,700 Aboriginal and Torres Strait Islander children around Australia [75]. Data on breastfeeding from this study showed that 80% of Aboriginal and Torres Strait Islander children had been breastfed at some time during their early years, and 22% of infants had been breastfed for at least 12 months. This study found that children living in more remote areas had been breastfed for a slightly longer period of time than those living in other areas [75].
Growth of infants and children
The growth of infants and children is an important marker of their health and development; disturbances in health and nutrition almost always affect growth [11]. Like poor growth in utero, poor growth in early childhood is associated with both short and long term health effects, including increased rate of acute infection and development of chronic diseases in later life [61, 76, 77]. Over-nutrition and obesity in infancy and childhood are also linked to poorer health outcomes [11]. Body size and growth velocity outside the ‘normal’ range during the early years of life are both associated with risk of overweight and obesity later in childhood and adulthood [11, 64, 78].
Healthy growth depends on a favourable combination of genetic and environmental influences [11, 12]. Environmental determinants of normal growth include good maternal health during pregnancy and healthy weaning and feeding practices. Growth can be hampered by under-nutrition (inadequate quantity of food and energy intake), malnutrition (inadequate quality of food), specific nutritional deficiencies, anaemia, infections and parasitic infestations.
Growth retardation among Aboriginal infants from around six months of age has been documented frequently since first assessed in the 1960s [11, 12, 17]. Many Aboriginal babies, characteristically lighter and smaller than non-Indigenous babies, were found to grow well over the first four to six months, followed by a fall-off in growth lasting until about three years of age. A similar overall pattern was also found for head growth [12]. This pattern of growth was thought to be a genetic characteristic, but studies subsequently demonstrated ‘normal’ growth in Aboriginal and Torres Strait Islander children exposed to reasonable living conditions [12, 64].
The general pattern of faltering growth appears to have persisted, at least in rural and remote areas of the NT and the Kimberley region of Western Australia (WA). Although there appears to have been some improvement since the 1960s [64, 79], there is a paucity of recent national data on growth of Aboriginal and Torres Strait Islander infants.
The recording of relatively poor growth of Aboriginal children living in remote areas of the NT resulted in the establishment in the late 1990s of the Growth Assessment and Action (GAA) Program, now called the Healthy Under 5 Kids Program [80]. More information about the program is included in Box 2.
A review of the program, undertaken in 2015, assessed at least one health measure in 3,497 of 3,850 (91%) children aged less than five years of age living in rural and remote communities; all data were available for less than 75% of children. Overall, the current levels continue the very gradual improvements in growth status that have occurred since the late 1990s [80].
According to the review, 15% of children were assessed as ‘stunted’ (more than two standard deviations below the median height for age of the reference population), 6% as ‘underweight’ (more than two standard deviations below the median weight for age) and 5% as ‘wasted’ (more than two standard deviations below the median weight for height) (Table 1). Of children between the ages of six months to five years, 17% were anaemic.
Table 1 Summary of results of the Healthy under 5 kids program, Northern Territory, 2015
| Characteristics | Resident children with characteristics | Total resident children measured | % Resident children measured with characteristic | Coverage (resident children measured / number of resident children) * |
|---|---|---|---|---|
| Stunted | 444 | 2,934 | 15% |
76% |
| Underweight | 193 | 3,458 | 6% | 90% |
| Wasted | 134 | 2,919 | 5% |
76% |
| Anaemic ** | 468 | 2,760 | 17% | 80% |
* Numbers in red indicate that coverage is less than 80%
** Children are not tested for anaemia until they are six months of age. Therefore the denominator for this calculation is the number of resident children aged between 6 and 59 months of age – 3,467.
Source: Northern Territory Department of Health Data Management and System Reporting Branch (2015) [3]
The factors contributing to the persisting growth deficiencies of many Aboriginal children are complex, but the most important are likely to be ‘persistently negative’ environmental factors – living in overcrowded, relatively unhygienic conditions, with poor food supply, repeated infections and poor nutrition [11, 12, 17].
Box 2: Healthy Under 5 Kids Program
The Healthy Under 5 Kids Program regularly provides information about the physical growth and nutrition of Aboriginal and Torres Strait Islander children in remote areas of the NT so that health service providers and policy makers can ensure that the right programs and policies are being put in place to address health needs from a population perspective. The report utilises data from all NT health service providers, including non-government organisations who have agreed to be part of the program [3]. Height and weight data are collated and analysed using the World Health Organization 2006 growth references [4] that identify how children should grow under optimal conditions, including optimal breastfeeding and appropriate introduction of solids from around six month of age [11]. Haemoglobin values are also assessed in children over six months of age and prevalence of anaemia calculated. For most metrics, cross-sectional population data are presented by age and by location. Trend data are also reported. For individual children, growth assessment is done by plotting weight and height over time on their growth chart. Individual needs can then be actioned by the health professional [3].
Overweight and obesity in childhood
There is increasing risk of overweight and obesity in childhood from both under-nutrition and over-nutrition in utero and infancy [5]. Increasing rates of overweight and obesity have been observed among Aboriginal and Torres Strait Islander children over the last two decades, particularly among Torres Strait Islanders [81]. A recent study of urban Aboriginal infants found that 37% were overweight or obese at two years of age [82]. A study of weight trends of children in New South Wales (NSW) shows the gap in weight status between Aboriginal and non-Indigenous children is widening. From 1997 to 2010, rates of excess weight and obesity rose 22.4% in Aboriginal children compared with 11.8% in non-Aboriginal children [83]. Further, the waist-to-height ratio, which indicates a greater lifetime risk of chronic diseases such as heart disease and type 2 diabetes, increased by more than 30% in the Aboriginal children [83]. In a large representative sample of Australian children aged 4–5 years, Aboriginal and Torres Strait Islander children were estimated to be 50% more likely to be overweight or obese compared to non-Indigenous children [84].
Anthropometric measurements of Aboriginal and Torres Strait Islander children were collected in the 2012-13 AATSIHS and body mass index (BMI3) calculated [67]. In 2012–13, 30% of Aboriginal and Torres Strait Islander children aged 2–14 years were overweight or obese (20% were overweight and 10% were obese), 62% were in the normal weight range and 8% were underweight. Combined overweight/obesity rates were similar for Aboriginal and Torres Strait Islander boys and girls (29% and 32% respectively). Rates of overweight and obesity among Aboriginal and Torres Strait Islander children tend to be higher than for all Australian children, although different age ranges and time periods makes comparison difficult; in 2014-15, 27.4% of non-Indigenous children aged 5-17 years were overweight or obese; 20.2% overweight and 7.4% obese [14].
A 2012 study of 277 Indigenous children aged 5-17 years in the Torres Strait in 2003 found that 46% were overweight or obese and 35% had abdominal obesity [85]. Girls had higher levels of abdominal obesity (50%) than boys (18%). The study also found a consistent association between overweight/obesity and low levels of physical activity.
Hardy and colleagues [83] found that from 1997 to 2010, overweight/obesity and waist hip ratio (WHR) increased more rapidlyin Aboriginalchildrenaged 5-16 yearsthaninnon-Aboriginal children in the same age-group in NSW. They identified lack of daily breakfast, excessive screen time and soft drink consumption as the major risk factors and suggested that encouraging strategies to limit screen time held promise.
Dietary intake of children
The 2012-13 National Aboriginal and Torres Strait Islander nutrition and physical activity survey (NATSINPAS) was the first national survey that assessed dietary intake in Aboriginal and Torres Strait Islander children. For this reason it is not possible to calculate trend data. NATSINPAS dietary intake data for Aboriginal and Torres Strait children are included with the adult and community data below.
Previous dietary studies in Aboriginal and Torres Strait Islander children have used self-reported dietary methods, but results have been considered unreliable, with large variance in intakes [86, 87]. However, available regional and community studies have consistently described low intakes of fruit and very low intakes of vegetables among Aboriginal and Torres Strait Islander children compared to dietary recommendations [11].
A recent study was undertaken to identify barriers to intake of fruit and vegetables among Aboriginal and Torres Strait Islander children in different settings throughout Australia [88]. The researchers analysed quantitative data from a longitudinal study of Aboriginal and Torres Strait Islander children and qualitative data from a key informant focus group. Almost half of the carers involved in the study (45%) reported a barrier to their child’s fruit and vegetable intake; dislike of fruit and vegetables was the most common barrier, reported by 33% of carers. Other barriers related to accessibility (7.4%), affordability (4.1%), lack of availability (<3.2%), quality (<0.7%), transport (<0.7%) and lack of preparation or storage facilities (<0.5%). Accessibility barriers were strongly related to remoteness. Within urban and inner regional areas, child and carer well-being, financial security, suitable housing and community cohesion were factors promoting access to fruit and vegetables. However, few factors associated with dislike were identified in the study [88].
Adult and community nutrition
The nutrition burden among Aboriginal and Torres Strait Islander adults is underscored by both over-nutrition (particularly over- consumption of unhealthy discretionary foods) and under-nutrition (dietary deficiencies related to inadequate intake of healthy foods) [5, 11, 14, 15, 89].
Burden of disease
Burden of disease analysis measures the impacts of diseases and injuries on a population, and the known risk factors for these diseases and injuries [7]. In the 2011 Burden of disease study, 13 dietary factors were identified as being risk factors for the Australian population (out of 29 risk factors). When combined, the joint effect of all dietary risks combined contributed 9.7% to the burden of disease for Aboriginal and Torres Strait Islander people. The contribution of dietary risk factors to the burden of disease was particularly notable in the 65 years and over age group, with a diet low in fruit contributing 4% to the burden for Aboriginal and Torres Strait Islander males and 3% for Aboriginal and Torres Strait Islander females. Around half of the health gap between Aboriginal and Torres Strait Islander people and non-Indigenous people (51%) is attributable to risk factors, with combined dietary factors contributing the greatest proportion of risk (27.4%) [7].
Dietary intake of Aboriginal and Torres Strait Islander groups
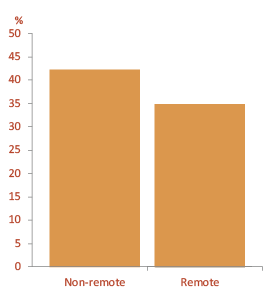
The dietary intake of Aboriginal and Torres Strait Islander people was estimated from self-reported 24-hour data collected for the first time nationally in the 2012-2013 NATSINPAS [14, 15]4. Reported dietary intakes were assessed by the ABS against relevant recommendations of the 2013 Australian dietary guidelines [11] and compared with reported intakes of non-Indigenous Australians (Figure 1) [14]. Key dietary data from the NATSINPAS are included below [14, 15].
Figure 1. Persons 2 years and over – average serves of Australian dietary guidelines food groups and discretionary foods by Indigenous status (a)(b), 2011-13
Notes:
(a) Based on Day 1: Day 1 intake refers to information collected from the first 24-hour dietary recall.
(b) From non-discretionary sources unless otherwise specified.
(c) A discretionary serve is defined as 500-600 kJ. Discretionary serves were derived by summing energy from discretionary foods and dividing by 550 kJ. Does not include meats that do not meet the Australian dietary guidelines criteria but are not flagged as discretionary.
Source: Australian Bureau of Statistics (2016) [16, 90]
Consumption of vegetables and legumes/beans
Aboriginal and Torres Strait Islander children (2-18 years) reported an average intake of 1.4 serves of vegetables a day and adults (aged 19 years and over) reported an average intake of 2.1 serves of vegetables per day [14]. Based on self-reported usual serves of vegetables eaten per day, only 8% of Aboriginal and Torres Strait Islander people met the recommended intake [15]. The average daily reported consumption of vegetable and legumes/beans serves for each age-sex group of Aboriginal and Torres Strait Islander people was markedly less than the respective recommendations. Females aged 15 years and over were more likely than their male counterparts to have eaten an adequate amount of vegetables (7% and 3% respectively) [91]. After age-adjustment, Aboriginal and Torres Strait Islander people aged 15 years or older were less likely than non-Indigenous people to be eating adequate amounts of vegetables (ratio 0.8) [14]. Aboriginal and Torres Strait Islander people living in non-remote areas were more likely than those in remote areas to have consumed some vegetables in the 24 hours prior to the survey (67% and 56% respectively) [92].
Consumption of fruit
Aboriginal and Torres Strait Islander children (2-18 years) reported an average intake of 1.6 serves of fruit a day and adults (aged 19 years and over) reported an average intake of one serve of fruit per day, which is half the recommended intake [14]. Based on self- reported usual serves of fruit eaten per day, 54% of Aboriginal and Torres Strait Islander people met the recommendations for usual serves [15]. Females were more likely than males to have eaten an adequate amount of fruit (57% and 51% respectively). Aboriginal and Torres Strait Islander people aged two years and over reported consuming around 1.2 serves of fruit per day compared with 1.5 serves per day in the non-Indigenous population. After age- adjustment, Aboriginal and Torres Strait Islander people aged 15 years or older were less likely than non-Indigenous people to be eating adequate amounts of fruit (ratio 0.9) [14]. Aboriginal and Torres Strait Islander people living in non-remote areas consumed more serves of fruit on average than those living in remote areas (1.3 serves compared with 0.9) and were more likely than those in remote areas to have consumed any fruit in the 24 hours prior to the survey (49% and 35% respectively) [92]. However, similar proportions of Aboriginal and Torres Strait Islander people living in remote and non-remote areas (around 50%) met the guidelines for daily serves of fruit [15]. Fruit juice made up about one-third (34%) of the fruit intake of Aboriginal and Torres Strait Islander adults, which is higher than recommended [12].
Consumption of grain (cereal) foods
Aboriginal and Torres Strait Islander people aged two years and over reported consuming an average of around 4.1 serves of healthy grain foods per day, compared with 4.5 serves among non-Indigenous Australians. Aboriginal and Torres Strait Islander people in remote areas consumed more serves of grain foods on average than those in non-remote areas (4.6 serves compared with
4.0 serves). One-quarter (25%) of grain foods consumed were from wholegrain and/or high fibre varieties, compared to the more than 50% recommended [14].
Consumption of milk, yoghurt, cheese and alternatives
Aboriginal and Torres Strait Islander people aged two years and over reported consuming an average of 1.2 serves of milk, yoghurt, cheese and alternatives per day, compared with 1.5 serves among non-Indigenous people [14]. Dairy milk was the most frequently consumed product (65%) followed by cheese (30%). Similar proportions of males and females (84% and 82% respectively), adults and children (81% and 84% respectively) and people in remote and non-remote areas (83%) reported consuming milk products and dishes. The average daily consumption of milk, yoghurt, cheese and alternatives for each age-sex group of Aboriginal and Torres Strait Islander people, with the exception of children aged 2-3 years and girls 4-8 years, was considerably lower than the respective recommend number of serves [14].
Consumption of lean meats and poultry, fish, eggs, tofu, nuts and seeds, and legumes/beans
Aboriginal and Torres Strait Islander people aged two years and over reported consuming an average of around 1.6 serves per day of healthy lean meats and poultry, fish, eggs, tofu, nuts and seeds and legumes/beans, which was slightly less than for non- Indigenous Australians (1.7 serves). Aboriginal and Torres Strait Islander people living in remote areas consumed more serves of this food group than those living in non-remote areas (2.0 serves compared with 1.4). Lean red meats made up almost half (49%) of the intake of foods in this group, and the contribution of lean red meats was higher for people living in remote areas compared with
non-remote areas (61% compared with 44%). The average daily consumption of lean meats and poultry, fish, eggs, tofu, nuts and seeds and legumes/beans for each age-sex group of Aboriginal and Torres Strait Islander people, with the exception of girls 2-3 years, was considerably less than the respective recommendations [14].
Water intake
Aboriginal and Torres Strait Islander people reported drinking an average of around one litre per day (997 ml) of plain water, including both bottled and tap water (compared with 1,073ml for non-Indigenous people). An additional 262 ml of water was reported consumed from other non-discretionary beverages such as tea and coffee. Plain water contributed just under half (48%) of Aboriginal and Torres Strait Islander peoples’ total beverage consumption, slightly less than that of non-Indigenous Australians (50%) [14].
Consumption of ‘healthy fats’ allowance
The healthy fats allowance is derived from unsaturated spreads and oils and/or the foods from which these are derived, such as nuts and seeds [11]. In 2012-13, Aboriginal and Torres Strait Islander people aged two years and over consumed an average 1.4 serves from the ‘healthy fats’ allowance, which is consistent with recommendations [11, 14].
Consumption of discretionary5 food and drinks
The Australian dietary guidelines recommend that discretionary foods and drinks should only be consumed sometimes and in small amounts [11]. However, over two-fifths (41%) of total daily energy in the foods and drinks reported consumed by Aboriginal and Torres Strait Islander people in 2012-13 came from foods and beverages classified as discretionary. This was higher than the proportion of total daily energy derived from discretionary foods and drinks in non-Indigenous Australians (35%).
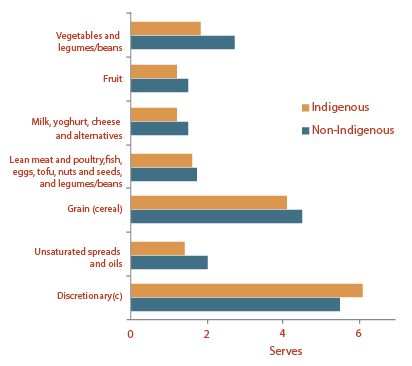
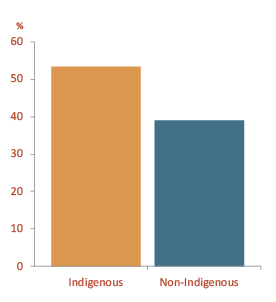
In terms of serves, Aboriginal and Torres Strait Islander people reported consuming an average of 6.1 serves of discretionary choices per day, which was higher than the non-Indigenous population average of 5.5 serves, for all age groups (Figure 2). In 2012-13, the leading contributors to discretionary choices among Aboriginal and Torres Strait Islander people were alcoholic beverages (10%), soft drinks (9.1%), potato products such as chips and fries (8.2%), pastries (7.1%), cakes and muffins (6.4%) and confectionary (6.3%) [14].
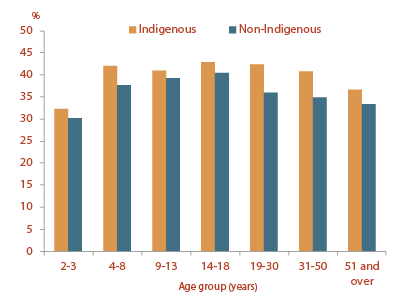
Aboriginal and Torres Strait Islander people living in remote areas obtained less energy from discretionary foods compared with those living in non-remote areas (35% and 42% respectively) (Figure 3). In particular, a lower proportion of Aboriginal and Torres Strait Islander adults living in remote areas reported consuming alcoholic beverages compared with those living in non-remote areas (14% compared with 20%) [15].
Figure 2. Proportion of energy from discretionary foods, by Indigenous status and age, 2012-13
Source: Australian Bureau of Statistics (2015) [15]
Figure 3. Proportion of energy from discretionary foods by remoteness, in Indigenous people, 2012-13
Source: Australian Bureau of Statistics (2015) [15]
Consumption of free sugars
The WHO recommends that both adults and children consume less than 10% of dietary energy from free sugars6 [57]. On average, Aboriginal and Torres Strait Islander people two years and over reported consuming an average of 75g (18 teaspoons) of free sugars per day, which equates to an average of 14% of dietary energy, nearly 50% more than WHO recommendations [93]. Added sugars made up the majority of free sugar intakes, with an average of 68g (16 teaspoons) consumed and an additional seven grams of free sugars coming from honey and fruit juice. The majority (87%) of free sugars were consumed from discretionary foods and drinks, with two- thirds (67%) of all free sugars coming from sugary drinks. The proportion of Aboriginal and Torres Strait Islanders who reported consuming sugary drinks was higher than non- Indigenous Australians in all age groups, especially children (Figure 4). Free sugar intake in Aboriginal and Torres Strait Islander groups was highest among older children and young adults, and higher in males than in females; teenage boys aged 14-18 years derived 18% of their dietary energy from free sugars [93]. Free sugar intake was 12g higher per day (3 teaspoons) among those living in non-remote areas than in remote areas. On average, Aboriginal and Torres Strait Islander people reported consuming 15g (around 4 teaspoons) more free sugars than non-Indigenous Australians. Aboriginal and Torres Strait Islander people consumed more free sugar per day than non-Indigenous Australians, with more derived from sugary drinks (67% compared to 51%).
Figure 4. Proportion of people consuming sweetened beverages, by Indigenous status, 2012-13
Source: Australian Bureau of Statistics (2015) [15]
Consumption of traditional bush foods
As a proxy measure of consumption of traditional bush foods, participants in the 2012-2013 NATSINPAS were asked about their consumption of foods that were naturally harvested or wild-caught, such as fish and seafood, wild harvested fruit and vegetables, reptiles and insects [15]. Aboriginal and Torres Strait Islander people in remote areas were more likely than their non- remote counterparts to eat non-commercially caught fin fish (7.8% and 1.8% respectively), crustaceans and molluscs (1.2% and 0.3% respectively), wild harvested meat (7.7% and 0% respectively) and reptiles (3.9% and 0.1% respectively). Aboriginal people living in remote NT communities reported frequent consumption of traditional foods [94].
Dietary change
The dietary patterns described in the NATSINPAS present a striking contrast to traditional Aboriginal and Torres Strait Islander diets [12, 22, 23]. Since European occupation of Australia in the late 18th century, the process of Aboriginal and Torres Strait Islander acculturation from a traditional hunter-gather life to a largely Westernised existence has been underscored by many social, political and environmental factors [11, 12]. Key components of dietary change are included in Table 2.
Table 2. Comparison of hunter-gatherer and contemporary Aboriginal and Torres Strait Islander diet
| Hunter–gatherer life | Contemporary life | |
|---|---|---|
| Energy intake | Adequate | Excessive |
| Energy density of the diet | Low | High |
| Nutrient density of the diet | High | Low |
| Physical activity level | High | Low |
| Protein content of diet | High | Low-moderate |
| Animal food intake | High | Moderate |
| Plant food intake | Moderate | Low |
| Carbohydrate intake | Moderate (slowly digested) | High (rapidly digested) |
| Complex carbohydrate intake | Moderate | Moderate |
| Sugars | Low | High |
| Dietary Fibre | High | Low |
| Fat | Low | High |
| Saturated fat | Low | High |
| Alcohol | Not available | Available |
| Sodium: potassium ratio | Low | High |
Source: Based on Lee A, O’Dea K (2015) [24]
Nutrient intake
Dietary intake reported in the 2012-2013 NATSINPAS was also analysed for key nutrients including sodium, folate, vitamin B12, calcium and iron [15].
Sodium (salt) consumption
According to the 2012-2013 NATSINPAS, the average daily amount of sodium in food reported consumed by Aboriginal and Torres Strait Islander people was 2,379mg (approximately one teaspoon of salt) [15]. This excludes salt added by consumers in household cooking or when preparing food. Sodium consumption was higher among males than females (2,638mg and 2,122mg respectively).
Almost half of Aboriginal and Torres Strait Islander people reported that they did not use salt in household cooking or preparing food (47%) [95]. This proportion was slightly higher for females than males (50% and 45% respectively), higher for people living in non-remote areas compared with those in remote areas (48% and 44% respectively) and for children aged 2-18 years compared with people aged 19 years or older (51% and 44% respectively). For those who used salt in household cooking or preparing food, fewer people used iodised salt than non-iodised salt (21% and 24% respectively). Recent modelling suggested that salt- reduction strategies could considerably reduce salt intake in remote Aboriginal and Torres Strait Islander communities without increasing risk of iodine deficiency at the population level [96].
The average reported daily sodium intake was similar for Aboriginal and Torres Strait Islander people and non-Indigenous people (2,379mg and 2,408mg respectively) [15]. Males recorded a higher consumption of sodium than females in both populations.
Folate consumption
The average daily amount of folate equivalents consumed by Aboriginal and Torres Strait Islander people from foods was 672 µg for males and 565µg for females. The average daily intake of folate equivalents was similar for Aboriginal and Torres Strait Islander people and non-Indigenous people (618µg and 614µg respectively), and average intakes exceeded the Estimated Average Requirement (EAR) for all age and gender groups. The amount of folate equivalents consumed by males (695µg) and females (572µg) in non-remote areas was higher than in remote areas (males 588µg, females 538µg). The major dietary source was folic acid supplemented cereal products (bread).
Vitamin B12 consumption
The amount of vitamin B12 consumed by Aboriginal and Torres Strait Islander people from foods averaged 5.0µg per day for males and 3.8µg for females, with the average of 4.4µg per day being similar to non-Indigenous Australians and exceeding the relevant EAR. The main sources of vitamin B12 were meat, poultry and game products in Aboriginal and Torres Strait Islander groups and milk and milk products in non-Indigenous Australians.
Calcium consumption
The daily amount of calcium consumed from foods and beverages by Aboriginal and Torres Strait Islander people averaged 734mg for males and 611mg for females. Intakes were lower than relevant EAR for children between the ages of 9 and 18 years, adult women and men over the age of 51 years. Aboriginal and Torres Strait Islander people in non-remote areas (711mg) had a higher calcium intake than those in remote areas (530mg). The average calcium intake for the Aboriginal and Torres Strait Islander population (673mg) was lower than the average intake for the non-Indigenous population (807mg). Milk was the major source of calcium in both populations.
Iron consumption
The average iron intake for Aboriginal and Torres Strait Islander people from food and beverages was 10mg per day, an average iron intake of 1.3mg per 1,000 kJ of energy. Intakes were the same for Aboriginal and Torres Strait Islander males and females and similar for Aboriginal and Torres Strait Islander and non-Indigenous populations. Aboriginal and Torres Strait Islander people living in remote areas had slightly higher iron intakes than those in non- remote areas (1.5mg and 1.3mg respectively).
Biomarkers of nutrition
The National Aboriginal and Torres Strait Islander health measures survey (NATSIHMS) 2012-2013 collected information on biomarkers of nutrition, including vitamin D, anaemia, iodine, folate status, blood pressure, blood lipids and anthropometric measurements [97]:
- More than a quarter of Aboriginal and Torres Strait Islander adults (27%) had a vitamin D deficiency. After age-adjustment, Aboriginal and Torres Strait Islander people were only slightly more likely to have a vitamin D deficiency than their non- Indigenous counterparts (ratio 1.1). The levels of vitamin D deficiency were similar for both Aboriginal and Torres Strait Islander males and females, and across all age-groups (ranging from 25% to 29%). Vitamin D deficiency was more common among Aboriginal and Torres Strait Islander people living in remote areas (39%) than those in non-remote areas (23%).
- The proportion of Aboriginal and Torres Strait Islander adults who were at risk of anaemia was 7.6%. Aboriginal and Torres Strait Islander adults were at higher risk of anaemia than their non-Indigenous counterparts in all age-groups (ratio 1.9 after age-adjustment). Women were more likely to be at risk of anaemia than men (10% compared with 4.8%). The risk of anaemia was higher for those living in remote areas compared with those living in non-remote areas (10% compared with 6.9%). Levels of anaemia were not assessed in Aboriginal and Torres Strait islander children in 2012-13.
- The Aboriginal and Torres Strait Islander adult population was found to be iodine-sufficient, with iodine levels higher than for non-Indigenous adults (median levels of 135ug/L compared with 124ug/L). Those living in remote areas had higher median levels than those living in non-remote areas [97].
- One fifth (20%) of Aboriginal and Torres Strait Islander adults had high blood pressure; more men (23%) had high blood pressure than women (18%).
- A quarter (25%) of Aboriginal and Torres Strait Islander adults had abnormal or high total cholesterol levels or high triglyceride levels. After adjusting for age, Aboriginal and Torres Strait Islander adults were nearly twice as likely (ratio 1.9) to have abnormally high triglycerides compared with non-Indigenous adults (27% compared with 14%). Aboriginal and Torres Strait Islander adults were less likely (ratio 0.8) than non-Indigenous adults to have high total cholesterol levels (26% compared with 33%).
Results of previous studies of nutrition status in Aboriginal and Torres Strait Islander communities, have described poor status of ascorbic acid, folate and beta-carotene consistent with the very low contemporary dietary intakes of fruit and vegetables, particularly in vulnerable groups such as infants, children, pregnant and breastfeeding women [12]. High rates of iron deficiency anaemia have also been described among young children [12]; anaemia is associated with negative impacts on physical and cognitive development during the early years and can reduce potential for educational attainment later in life [65]. Where investigated, multiple nutrient deficiencies have tended to cluster in individuals, suggesting generally poor nutritional status, rather than any specific micro-nutrient problem [11].
Bodyweight
Obesity and abdominal obesity, as measured by BMI and waist circumference (WC), have been shown to be risk factors for type 2 diabetes and hypertension in Aboriginal and Torres Strait Islander people. Information on BMI and WC for measuring weight and chronic disease risk, including in Aboriginal and Torres Strait Islander populations, is included in Box 3.
Based on BMI information collected as a part of the 2012-2013 AATSIHS, 66% of Aboriginal and Torres Strait Islander people aged 15 years or older were classified as overweight (29%) or obese (37%) [31]. A further 30% were normal weight and 4% were underweight. Combined overweight/obesity levels were significantly higher for people living in non-remote areas (67%) than for those living in remote areas (62%). Similar proportions of Aboriginal and Torres Strait Islander males and females were overweight or obese (66% and 67% respectively). A larger proportion of males than females were overweight (31% and 26% respectively), while a greater proportion of females than males were obese (40% and 34% respectively); however the only statistically significant difference in obesity rates between females and males was in the 45–54 year age group (50% compared with 35%).
After age-adjustment, the combined overweight/obesity levels were slightly higher for Aboriginal and Torres Strait Islander people aged 15 years or older than for their non-Indigenous counterparts (ratio 1.2) and Aboriginal and Torres Strait Islander people were 1.6 times as likely as non-Indigenous people to be obese (ratio 1.4 for males and 1.7 for females).
Box 3: Measuring weight and chronic disease risk
The standard measure for classifying a person’s weight status is Body Mass Index (BMI). BMI is defined as a person’s weight in kilograms divided by height in metres squared [98]. Being overweight (BMI 25 to 29) or obese (BMI of 30 or more) increases a person’s risk for cardiovascular disease, type 2 diabetes, certain cancers, and some musculoskeletal conditions. Being underweight (BMI less than 18.5) can also have adverse health consequences, including lower immunity (leading to increased susceptibility to some infectious diseases) and osteoporosis (bone loss) [99].
Abdominal obesity, a risk factor for the development of the metabolic syndrome, can be measured by waist circumference (WC) alone (greater than 94cm for men and greater than 80cm for women), or waist-hip ratio (WHR) (greater than or equal to
0.90 for men and greater than or equal to 0.85 for women) [99].
Measurement issues in Aboriginal and Torres Strait islander populations
There is evidence that, in common with some other populations at high risk of diabetes and related conditions (such as South Asians), that the healthy BMI range is lower for Aborigines than for Australians of European origin [11]. Aboriginal people tend to have a ‘linear’ body build – being narrow across the shoulders and hips and having relatively longer limbs and shorter torso – and relatively more body fat, which tends to be deposited centrally (abdominally), for a given BMI. It has been suggested that a BMI of 22 might be more appropriate than 25 as a measure of acceptable BMI for Aboriginal people. Conversely, the healthy BMI range of Torres Strait Islander groups tends to be higher than for Australians of European origin [11].
As fat tends to be deposited centrally in both Aboriginal men and women, even modest weight gains can be associated with increased cardio-metabolic risk: insulin resistance, impaired glucose tolerance and dyslipidaemia [11, 100]. Therefore, optimal BMI and WC cut-offs are still uncertain for Aboriginal and Torres Strait Islander people when calculating diabetes type 2 and cardiovascular risk [64, 101, 102].
There is evidence that measuring the WHR in Aboriginal and Torres Strait Islander people is more accurate and easier to measure than BMI [64]. More recently, Hughes and colleagues [103] have developed an equation for calculating fat free mass in Aboriginal and Torres Strait Islander adults using the easily acquired variables of resistance7, height, weight, age and gender for use in the clinical assessment and management of obesity.
Aboriginal and Torres Strait Islander adults in non-remote areas who were sufficiently physically active were less likely to be obese than those who were fully inactive (31% compared with 56%); however causality cannot be implied by this association [97].
In 2012-2013, around 3.5% of Aboriginal and Torres Strait Islander people aged 15 years or older were underweight, with about 2.8% of Aboriginal and Torres Strait Islander males and 4.2% of Aboriginal and Torres Strait Islander females having a BMI of less than 18.5 [67]. After age-adjustment, Aboriginal and Torres Strait Islander people were 1.6 times more likely to be underweight than non-Indigenous people (rate ratio for males 1.8 and females 1.4) but less likely to be of normal weight (rate ratio 0.7).
Measurements of WC and WHR were taken in the 2012-2013 AATSIHS (not in the previous health survey) to help determine levels of risk for developing certain chronic diseases [91]. Based on WC, a higher proportion of Aboriginal and Torres Strait Islander females (81%) than Aboriginal and Torres Strait Islander males (62%) aged 18 years or older were found to be at increased risk. Based on WHR, 81% of males and 73% of females aged 18 years or older were at increased risk of developing chronic diseases. The proportions of Aboriginal and Torres Strait Islander males and females who were at increased risk of developing chronic diseases based on both measures of WC and WHR increased with age.
Community level diet and nutrition data
Remote communities
In order to collect reliable estimates of dietary intake at a community level in remote Aboriginal communities where there are a limited number of food outlets, the ‘store turnover method’ was developed in the 1990s and validated against objective biomedical data [24, 104-106]. The method has been recently updated to include use of bar code scanning [107]. Results have shown little change in dietary intake over the past 25 years [30, 37, 107]. While there have been some improvements in intake of fruit and vegetables, intakes are still less than 20% of recommended levels. Diets remain high in sugar, white bread and/or flour, and have increased in sugar sweetened beverages; there is now greater reliance on ‘convenience’, takeaway and ‘fast’ foods [30, 37, 107]. In remote central Australian communities, ‘discretionary’ foods and drinks provided 35% energy intake in the 1980s, but now provide 41% energy and 84% sugar intake [30]. In three communities in northern Australia, around 25% of food expenditure was on non- alcoholic beverages, (around 16% specifically on sugar-sweetened beverages) and only about 2% on fruit and 5% on vegetables [107]. Lack of change in spending patterns in another community between 1997 and 2011 has also been summarised [108]. Where data are available, the dietary profile tends to be better in those remote communities where more traditional foods are consumed [11, 109].
In Torres Strait communities marine foods continue to make substantial contributions to the diet and many men, women and children living in the Torres Strait are involved in different aspects of collecting shellfish, fishing and hunting [24]. Concerns have been raised more recently about the heavy metal content in the organ meat of dugong and turtle [110]. Production of traditional garden staples continues to be important for some ceremonial purposes in Torres Strait communities [25]. When assessed by the ‘store turnover’ method in the 1990s, more than half the energy in the community diet was found to be derived from white flour, white rice, tinned meat and vegetable oil [25]. Apparent dietary intake of fruit and vegetables from the community stores was about 15% and 30% respectively of recommended levels; people who depended on store foods would not be able to meet their needs for vitamins A, C and E and folic acid [25]. More recent dietary intake data for the region are not available.
Urban communities
Beyond the individual data from the NATSINPAS reported above, limited dietary data are available for urban Aboriginal settings [111, 112]. A comparison of the food habits of Aboriginal and non-Indigenous people in a city and a country town showed that in both localities Aboriginal groups consumed takeaway meals and added salt more often than their non-Indigenous counterparts [113]; recent studies have confirmed high intakes of salt in a regional town [111]. A recent systematic review has confirmed that the diets of Aboriginal and Torres Strait Islander people in all areas are inadequate, and that a more concerted approach to understanding dietary patterns of Aboriginal and Torres Strait Islander peoples is required [114].
Food security
Food security exists “when all people, at all times, have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life” [115]. Food security is considered a fundamental human right [116] and the Universal Declaration of Human Rights states “everyone has the right to a standard of living adequate for the health and well- being of himself and of his family, including food” [117]. The right to adequate food is seen not as a right to be fed but “a right of people to be given a fair opportunity to feed themselves, now and in the future” [118]. Food security is impacted by availability, accessibility, affordability and acceptability (appropriateness) of food.
The 2012-2013 NATSINPAS attempted to address the issue of food security by asking respondents if they had run out of food and couldn’t afford to buy more in the last 12 months [119]. This was a problem for 22% of respondents; 7% of respondents had run out of and gone without food, while 15% had run out but not gone without food.
More than one in five (22%) Aboriginal and Torres Strait Islander people were living in a household that, in the previous 12 months, had run out of food and had not been able to afford to buy more [15]. This was much higher than in the non-Indigenous population (3.7%). Aboriginal and Torres Strait Islander people in remote areas were more likely to run out of food than those in non-remote areas (31% and 20% respectively) and slightly more likely to go without food (9.2% and 6.4% respectively).
As national surveys are unlikely to include data for the most vulnerable groups, such as homeless people, these results are likely to underestimate the true extent of the problem [24, 120].
In previous studies, around 30% of Aboriginal and Torres Strait Islander adults reported they sometimes worried about going without food, and the proportion of Aboriginal and Torres Strait Islander households that had run out of food ranged from 18% in NSW to 45% in the NT [121].
To improve food security it is necessary to take a food systems approach [122]. The underlying causes of food insecurity in Aboriginal and Torres Strait Islander communities include socioeconomic factors such as income and employment, housing, over-crowding, transport, food costs, cultural food values, education, food and nutrition literacy, knowledge and skills as discussed above.
Lack of food security causes hunger and anxiety related to food shortage in the short term, and serious health consequences related to malnutrition in the medium to long term, including conditions mediated by both under-nutrition and obesity [120]. While it may seem paradoxical that food insecurity is linked to obesity, this can arise because ‘filling up’ on some energy-dense, relatively nutrient-poor foods (such as flour and sugar) can cost less than ‘filling up’ on nutrient-dense whole foods, such as lean meats, fresh vegetables and fruits [123, 124]. Young children and pregnant and breastfeeding women tend to be particularly vulnerable to the short and longer-term effects of food insecurity, which can impact on children’s growth, physical and socio-emotional development and learning potential [120].
Access to food stores and transport are important nutrition determinants in urban, regional and remote locations. Large supermarkets, through economies of scale, are generally less expensive and offer the greatest variety of food choices compared with smaller independent food stores [125]. However access to large supermarkets is heavily influenced by their location and shoppers ability to easily access them, particularly if they do not own a car. Connectivity between food stores and residential areas compromises food security for people living in both urban and regional areas [125]. Transport to food outlets and quality of public transport are strongly and independently associated with food insecurity in urban Australia [126].
Costs of poor diet and nutrition
The most recent available estimate of the financial cost of poor diet and nutrition (based on costings from 1990) for the total cost to Australia of poor nutrition was more than $5 billion per year, including direct healthcare costs of $3 billion per year [127]. Given that, in 2008 in Australia, the direct costs and total annual cost (including health system costs, loss of productivity costs and carers’ costs) of obesity alone, was estimated at $8.3 billion and around
$58 billion respectively [128], the current cost of poor nutrition in Australia is now likely to greatly exceed the 1990 estimates [12].
More recent estimates of the cost of overweight and obesity are higher still; direct costs of obesity in 2011-2012 were estimated to be $8.6 billion (in 2014-15 dollars) [129] the cost to Australia’s collective wellbeing was estimated to be $120 billion by the Herald/Age Lateral Economics Index [130].
Among specific population groups, it has recently been estimated that the cost of obesity in pre-schoolers alone is $17M per year in Australia [131]. It was estimated that each obese child incurs a healthcare cost $367 above that of a child of healthy weight and that the direct healthcare costs of children with obesity aged 2-4 years were 1.62 times those of healthy weight children.
The cost of poor diet or overweight/obesity in Aboriginal and Torres Strait Islander people has not been estimated. There is an urgent need for the estimated cost of poor nutrition in Australia to be updated, including costs due to poor Aboriginal and Torres Strait Islander diets [35].
Nutrition programs and services
All nutrition programs ultimately aim to address the prevention or management of disease and the promotion of health and wellbeing. A range of Australian Government Department of Health programs contribute to the prevention and management of diet-related disorders among Aboriginal and Torres Strait Islanders at a national level [132]. However, despite government investment in these programs, and broader initiatives such as Closing the Gap, disproportionately poor diets, poor nutrition and high levels of diet-related conditions persist in Aboriginal and Torres Strait Islander communities [6, 8, 10, 11, 13, 133].
While many programs targeting nutritional issues are implemented as healthy lifestyle programs to address obesity, it must be remembered that diet is more than a lifestyle choice – it is determined by the availability of and access to healthy food, and by having the infrastructure, knowledge and skills to prepare food appropriately [11, 114, 134]. Reviews of evaluated programs that include any focus on improving nutrition in Aboriginal and Torres Strait Islander people, consistently show that multi-strategy environmental interventions to address broader determinants, such as policy actions to improve food supply, are among the most effective [11, 12, 18, 24, 112, 135-144].
As with all health programs, nutrition programs should be developed with the target communities, be delivered sensitively, be tailored to community needs, and not be forced, or perceived to be forced, upon communities. A major success factor is community involvement in (and, ideally, control of) all stages of program initiation, development, implementation and evaluation [112, 140]. Program implementation methods that build confidence among collaborating Aboriginal and non-Aboriginal health agencies are fundamental to building capacity to enhance Aboriginal nutrition and health [145].
The three main levels of nutrition programs are: a whole of population approach (primarily focused on prevention); a community approach (food supply and demand); and a targeted individual approach (especially clinical dietetic services). Such a large proportion of the Aboriginal and Torres Strait Islander population is affected by poor diet, that intervention is required at all levels – effective action requires a whole-of-life approach across the whole health continuum [146-149].
Few programs have been evaluated rigorously, especially in urban areas, or in the long term [112, 140, 150].
Whole of population approach
Programs implemented at the broad population level (such as at national or at a state and territory level) generally focus on primary prevention of disease. They may include social marketing programs (that employ multi-media buys on television, radio and/ or print and social media strategies, supported by broader health promotion approaches, such as point of sale promotions) or may involve a population-wide intervention (such as food fortification or labelling). Some whole of population strategies in Australia have included components targeted to Aboriginal and Torres Strait Islander groups.
Social marketing campaigns
An example of programs that fall into this category include the Tomorrow People campaign; part of the Australian Better Health Initiative’s Measure Up campaign [151]. A joint Federal, state and territory government initiative, Tomorrow People was about promoting simple changes to eating habits and being active for Aboriginal and Torres Strait Islander people. No evaluation data are available and the program has been discontinued.
Food fortification
In September 2009, Australia implemented mandatory folic acid fortification of wheat flour for bread making to reduce the incidence of neural tube defects [152]. Baseline data [153] showed 10% of Aboriginal women and 26% of Aboriginal men participants had red blood cell (RBC) folate concentrations below 250ng/mL, the cut- off associated with folate deficiency. None of the non-Aboriginal women and 4% of the non-Aboriginal men had red blood cell folate concentrations below 250ng/mL. All participants were vitamin B12 replete. The higher prevalence of folate deficiency in Aboriginal participants suggested they were more likely to benefit from a universal program of folate fortification. After fortification, no group was deficient in folate, suggesting that the population health intervention had the desired effect of increasing folate status in the Australian Aboriginal population [154].
In September 2009, Australia implemented mandatory iodine fortification of bread to reduce iodine deficiency in some areas of Australia [152]. Mild iodine deficiency in Aboriginal populations in the NT was described prior to iodine fortification; modelling determined that bread fortification was not sufficient for pregnant and non-pregnant individuals of this population [155]. Evaluation of the program showed increased intake of iodine in women of childbearing age and young children in the general population, but data for Aboriginal and Torres Strait Islander populations are not yet available [152].
Community approach
A range of nutrition programs have been implemented at community level. Some have focussed on improving food supply (availability, affordability, accessibility and acceptability of healthy food), many have focussed on increasing demand for healthy food, and a few multi-strategy programs have targeted both areas [112, 140, 146].
Multi-strategy community programs
A long-term, multi-strategy community program that has demonstrated considerable success is the Looma Healthy Lifestyle Project which began in 1993 [18, 156, 157]. Interventions and activities offered included: cooking classes and store tours; promotionoftraditionalcookingmethods; huntingtrips; sportsand walking groups; and informal education sessions about diabetes and chronic diseases. By 2000, evaluation showed improvements in a range of coronary heart disease risk factors related to diet, but no significant changes in the prevalence of obesity or diabetes in the community [156].
A subsequent health assessment in 2009 found that the prevalence of diabetes in the community had not increased since 2003 [18]. Children and young people in the community were found to be relatively healthy, with 84% of those under 18 years of age being of normal weight, compared with 77% nationally.
The Minjilang Health and Nutrition Survival Tucker Project was a community program that employed multiple strategies including: individual health assessment and feedback; the provision, promotion and cross-subsidisation of nutritious foods in the store; and physical activity promotion [158]. The project began in Minjilang (on Croker Island in the NT) in 1989 and ran intensively for 12 months. The evaluation involved store turnover data (validated as a measure of community dietary intake), objective biomedical data, and comparison of store turnover with a control community for nine years. Observed dietary changes included doubling of fruit and vegetable intake and a decrease in intakes of sugars and saturated fats compared with the control community. Improvements in biomarkers included marked reductions in serum triglycerides, cholesterol and blood pressure, and increases in red blood cell folate, and serum vitamin C and carotenoids. There was also a small but significant decrease in BMI and improved glucose tolerance among older women. After the initial funding ceased, the program was continued by the community. Most dietary changes persisted for at least three years, although sugar turnover rebounded slightly [158]. Subsequently, store managers were shown to be key ‘gate-keepers’ to community nutrition [47, 51]. As one outcome, the Arnhem Land Progress Association introduced a successful nutrition policy in all stores [159].
Similar community-based programs were implemented in four remote WA Aboriginal communities [160]. Although dietary changes were not reported, biomedical results in one of the communities showed 49% of the participants had lost weight and over half had lower cholesterol (59%) and lower blood glucose levels (54%) after several months.
The Many Rivers Diabetes Prevention Project commenced in NSW in 2011 [161]. Evaluation demonstrated positive governance and social outcomes, increased knowledge and awareness among participants and families, and improved understanding of the barriers and enablers of successful intervention programs [161]. However, reported dietary impacts were mixed and tended to be more pronounced in non-Indigenous children and among Aboriginal and Torres Strait Islander girls.
The impact of efforts to improve nutrition in several communities on the Anangu Pitjantjatjara Yankunytjatjara (APY) Lands over 30 years was evaluated using multiple methods in 2015 [30]. Impacts included decreased sugar turnover, doubling of fruit and vegetable turnover, increased availability and affordability of healthy foods and consequent improvement in nutrient intakes. However the overall effect has been a decrease in total diet quality since 1986, characterised by an increase in discretionary foods from providing 35% of energy intake to 41% of energy intake. Results reflect changes to the general Australian food supply, and suggested that, in the absence of supportive regulation and market intervention, adequate and sustained resources are required to improve nutrition [30].
Food supply programs
Improving the availability, variety, quality and access of healthy foods can be achieved through improving stores and retail food outlets, transport, local food production, prepared food provision and food aid and subsidies.
Store and other food supply programs
Efforts to influence local food supply through changes in food retail practices have been most commonly been applied in remote communities that rely on a single community store. Store nutrition policies [159] and store managers [47, 51] have been shown to be important influences on the food supply in remote Aboriginal and Torres Strait Islander communities.
Among food supply factors shown to influence community diets has been the availability of specific healthy foods (fruit and vegetables) and unhealthy foods (fatty takeaway and convenience foods) and sugary drinks and price (including cross-subsidisation) and advertising [30, 38, 98, 156, 158, 160, 162-164]. In this regard, community stores should be seen as essential services, like health and education, rather than simply viewed as small businesses [30, 44, 46].
In one community store, sales of sugary drinks fell after removal of the most popular brands of sugary drinks from the store at the request of the community in 2009 [163]. However, sales of alternative sources of sugar such as cordial and sweet biscuits are now higher at that store than the others surveyed in 2012 [30]. This demonstrates the need to consider unintended consequences and to assess full store turnover when evaluating nutrition interventions in remote communities.
The Shop@RiC randomised controlled trial tested the impact and cost effectiveness of a 20% price discount only and a combined price discount and in-store nutrition education strategy on purchasing of fruit and vegetables, diet drinks and water in 20 remote Aboriginal communities over two years using a novel step wedge design [165]. Benefits were modest (such as mean increased intake of a quarter of a piece of fruit per day), mixed (such as mean 6% increase in intake of sugar sweetened drinks) and were potentially undermined by unintended consequences [164]. The authors proposed that bigger subsidies and implementation of additional intervention strategies may have increased positive results.
In urban and regional areas, mapping of community food outlets has been a feature of recent programs trying to improve access to healthy food, such as the Many Rivers Research project [161].
Opportunities to improve the food supplied by Aboriginal and Torres Strait Islander and other community organisations, such as at meetings, community barbecues, group programs and other community events, and in children’s services, hostels, sports clubs and aged-care facilities, have been studied relatively rarely [166]. However, successful examples include projects at a sporting club canteen [167] and a school holiday program [168].
Local food production
Community gardens are commonly identified as a solution to addressing food security in Aboriginal and Torres Strait Islander communities[143, 169, 170].Thereismoreevidenceofeffectiveness of home gardens in Torres Strait Islander communities, than on the mainland [25, 169] reflecting the relatively infertile soils, the effect of insects and other pests, and that agriculture can be inconsistent with mobility associated with Aboriginal cultural life [12].
School gardens can be a popular alternative in Aboriginal and Torres Strait Islander communities, as they are easier to coordinate and have the backup of staff and students to work in the garden on a daily basis, although school holidays do need to be considered [171, 172]. Evaluations of the Stephanie Alexander Kitchen Gardens Foundation program [173, 174] found that, although there were many positive social and learning outcomes of the program, there was less evidence that it improved children’s dietary intake of fruit and vegetables.
Such ventures require intensive and dedicated resources, and there are no examples of sustainable gardens contributing significantly and cost-effectively to communities’ diets, particularly on the mainland [25, 143, 169-175].
Food aid
Food subsidy programs can improve food security by providing families with healthy foods, such as vegetables and fruit, or food vouchers [176-180]. These programs may be less successful, however, when perceived as charity rather than as a service [112, 181, 182] and not supported by community Elders [141, 183, 184].
Among Aboriginal and Torres Strait Islander groups, subsidised food has most commonly been provided at the local level for breakfast or lunch, particularly in children’s settings such as schools or preschools [160, 167, 183-188]. In the 1970s, the provision of hot meals and nutritious snacks to Aboriginal and Torres Strait Islander children in preschool demonstrated some positive impacts [176]. However, recent studies in Aboriginal and Torres Strait Islander communities suggest that feeding programs should only be implemented when food insecurity is a major issue and when the local community supports such programs [141, 183]. An evaluation of Aboriginal nutrition projects in WA found that provision of school meals at low or no cost, combined with classroom nutrition education delivered by a respected community Elder, were most effective [184].
Not-for-profit organisations such as FoodBank (https://www. foodbank.org.au/), Second Bite (http://secondbite.org/) and OzHarvest (http://www.ozharvest.org/) source food that would otherwise go to waste and redistribute to other food relief agencies and community food programs supporting people in need. However, these programs have not been evaluated at the level of health impacts or outcomes for specific population groups.
The Victorian Aboriginal Community Controlled Health Organisation (VACCHO) partnered with Second Bite recently to develop Sharing the Tracks to Good Tucker: Aboriginal Community Food Program Success Stories [189] which highlights several examples of local projects demonstrating positive processes and social impacts.
Among more recent work, the Bulgarr Fruit and Vegetable Program provided a weekly box of subsidised fruit and vegetables to families whose children were attending any one of three local Aboriginal Medical Services (AMSs) for health assessments. Families made a co-payment of $5 for the fruit and vegetable box, which was worth
$40-$60 (depending on the size of the box which was determined by the number of children). After 12 months, involvement in the subsidy program was associated with improvements in plasma levels of vitamin biomarkers of fruit and vegetable intake in children. However, there was no significant change in self-reported fruit or vegetable intake or measured weight status (which could be expected to take longer to change) [178]. There were also some broader health benefits, including a significant decrease in oral antibiotic prescriptions [179].
Recent trials of specific nutrient supplementation have not been successful [190] and do not address the underlying issues of food insecurity or poor dietary patterns [12].
Nutrition education and food literacy programs to increase demand for healthy foods
While nutrition education alone will not improve food security or dietary intake [12], it can be effective when combined with a range of other strategies to help people access healthy food. Nutrition education programs in Aboriginal and Torres Strait Islander communities have aimed to increase food and nutrition knowledge, skills and/or abilities and have ranged from structured workshops (such as [191, 192]) to less formal information sessions [184, 185, 193-196]. However, few education programs have been evaluated.
Cooking programs are very popular [185, 197-199]. Different models include cooking demonstrations [192, 200, 201], cooking classes [199, 202-204] and the development of community kitchens [168, 196, 199, 205]. Several whole-of-population programs, such as the school-based Need for Feed Program [206] and Jamie Oliver’s Ministry of Food [207] include targeted Aboriginal and Torres Strait Islander sessions.
Among food literacy and cooking programs, the community kitchens model may be particularly relevant for Aboriginal and Torres Strait Islander communities as it is based on community development principles and supports empowerment and self- efficacy. Local [112, 208] and international [209] evidence suggests that these programs can improve participants’ food security through developing cooking, shopping and budgeting skills as well as reducing social isolation. However, it has been suggested that some cook books developed for such programs reinforce western values and disregard traditional food ways [210].
Perceptions of the usefulness of the budgeting program FOODcents [192, 211] were very high and comparable between Aboriginal and non-Aboriginal participants. Significantly larger improvements in confidence, nutrition knowledge, and reported dietary behaviours were evident among Aboriginal participants [212]. The researchers concluded that adult nutrition education programs that address specific knowledge and skill deficits that are common among disadvantaged groups can be effective for multiple target groups, and may also assist in reducing nutrition-related inequalities.
A recent program designed to help people reduce their risk of developing diabetes and cardiovascular disease, is currently funded by the Victorian Government and managed by Diabetes Australia-Victoria [213]. The Life! program offers a course specifically for Aboriginal people and their families called the Road to Good Health. Run by Aboriginal Health Workers and other health professionals, this course supports participants to make long term, sustainable lifestyle changes, such as adopting a healthier diet and becoming more physically active [214]. A working group, that includes some Aboriginal and/or Torres Strait Islander members and organisations, has ensured that Aboriginal and Torres Strait Islander values and health promotion practices are embedded in the course. Results of process evaluation suggests the course is culturally relevant and valuable to users, but published evaluations of impact are not yet available.
Individual approach
At a local level, most mainstream and Community Controlled Primary Health Care Services in Australia could play a critical role in the delivery of nutrition and dietetic services. To meet the needs of Aboriginal and Torres Strait Islander people, primary health care services need to deliver both competent and culturally appropriate chronic disease care [215, 216].
The involvement of Aboriginal and Torres Strait Islander Health Workers has been identified by health professionals and patients as an important factor in the delivery of effective clinical care to Aboriginal and Torres Strait Islander people, including nutrition education [215, 217]. However, barriers to the involvement of Aboriginal and Torres Strait Islander Health Workers include: inadequate training; lack of clear role divisions among health care professionals; lack of stable relationships with non-Indigenous staff; and high demands for acute care [218]. The need for a greater number of Aboriginal and Torres Strait Islander Health Workers and better training in nutrition has been identified [133, 219, 220].
Aboriginal and Torres Strait Islander Community Controlled Primary Health Care Services play a major role in delivering essential primary health care services to Aboriginal and Torres Strait Islander people in a culturally secure manner [221]. Health services run by Aboriginal and Torres Strait Islander communities provide holistic care that is relevant to the local community and address the physical, social, spiritual and emotional health of the clients [214]. Such services can deliver effective prevention and management programs that enable lifestyle changes that are maintained and supported by the community [222].
It is generally accepted that inadequate access to primary health care services contributes to the poor health status of Aboriginal and Torres Strait Islander people [222].
Peer educator programs
The effectiveness of education type strategies can be enhanced when a ‘train the trainer’ or peer education model is used to deliver education to individuals or small groups [223]. Of the programs reviewed many used a peer education approach, training Aboriginal workers to deliver nutrition activities for their own communities [105, 158, 192, 195, 196, 200, 201, 224-226]. A person who is familiar with the language, culture and family context is well placed to deliver education that is appropriate and relevant for their local community. The sustainability of a peer education approach strategy is likely to be greater when educators are paid for their time, rather than relying upon volunteers. Several programs have engaged Elders to build on traditional knowledge and stories [227]. Providing opportunities for Aboriginal and Torres Strait Islander people to train and be employed in dedicated nutrition positions is critical to advancing nutrition and food security in the longer term [228, 229].
The Community Foodies program in SA is a nutrition program that aims to build the capacity of communities to make healthier food choices by training and supporting volunteer community members (Foodies) to act as agents for change. The Aboriginal and Torres Strait Islander Community Foodies, also known as Outback Community Foodies, has developed culturally appropriate resources, but has only been evaluated at process level [196].
The Deadly Choices program in Queensland (Qld) aims to empower Aboriginal and Torres Strait Islander people to make healthy choices for themselves and their families. One evaluated component has been the school-based chronic disease education initiative for young Aboriginal and Torres Strait Islander students (years 7 to 12) in Brisbane, Qld [230]. The program provided health and nutrition education, opportunities for participation in physical activity, and made arrangements for health checks. A recent evaluation of the program found that participants demonstrated significant improvements over time in knowledge, attitudes and self-efficacy associated with types of chronic disease, chronic disease risk factors, prevention and health checks. The evaluation also found significant increases in breakfast frequency and physical activity per week, fruit and vegetable consumption per day, and the uptake of health checks among students who participated in the program. The students who took part in the program showed a significant improvement in their knowledge of chronic disease and associated risk factors, and a significant increase in their breakfast frequency compared with a control group [230].
Aboriginal and Torres Strait Islander nutrition workforce
A key feature of many of successful nutrition interventions is the recruitment, training and support of Aboriginal and Torres Strait Islander workers in dedicated positions to promote nutrition [12, 133]. Many early successful programs emphasised the importance of professional partnerships between non-Indigenous nutritionists and Aboriginal Health Workers, and demonstrated the effectiveness of providing culturally appropriate training programs and educational resources for Aboriginal Health Workers [12, 231]. A trained nutrition workforce, with excellent cross-cultural competency and communication skills is needed to deliver effective interventions [146, 232, 233]. In particular, a trained, well-supported and resourced Aboriginal and Torres Strait Islander nutrition workforce is essential [81, 133, 230].
Until 2010, food and nutrition units were integrated into core Aboriginal Health Worker primary health care training. Effective, structured training of Aboriginal and Torres Strait Islander Health Workers in Certificate Level III or Level IV nutrition, in both clinical and preventive community health, was available through Technical and Further Education (TAFE) colleges in some Australian jurisdictions [133]. However, the current status of Aboriginal and Torres Strait Islander nutrition worker training, nationally, is unknown.
It is estimated that less than 20 Aboriginal and Torres Strait Islanders have ever trained as nutritionists and/or dietitians in Australian universities [208, 234, 235].
It is difficult to identify the number of health professionals delivering nutrition and dietetic services to Aboriginal and Torres Strait Islander people in Australia. Dietitians and nutritionists are not required to be registered in Australia, so data are not available from Indigenous Allied Health Australia (www.iaha.com.au) or the Australian Government’s health workforce data website (http:// data.hwa.gov.au). It is estimated that there are 14 identified Aboriginal and Torres Strait Islander dietitians and/or nutritionists working in Australia; however it is unknown whether they are employed in mainstream or specific Aboriginal and Torres Strait Islander health services [234, 235]. Neither is it known how many non-Indigenous dietitians/nutritionists are employed to provide mainstream or Aboriginal and Torres Strait Islander specific health services. In 2013, there were 122 Indigenous Allied Health practitioners and 48 Indigenous health promotion practitioners in Australia, but of these very few work in nutrition [222, 234]. Similarly, it is unknown how many of the 910 Aboriginal and Torres Strait Islander Health Workers (that is, those with Certificate Level III or Level IV) has trained in nutrition or are working in that area.
There is a lack of Aboriginal and Torres Strait Islander specific nutrition positions available at all levels nationally [172, 208]. Nutrition professionals working in Aboriginal and Torres Strait Islander health are employed mainly in the government public sector and Aboriginal and Torres Strait Islander Community Controlled Health Care services [149, 232]. Private health insurance also supports access to private dietetic services, but relatively few Aboriginal and Torres Strait Islander people hold, or can afford, private health insurance compared to other Australians [208]. Qld and the NT have previously adopted a systematic approach to Aboriginal and Torres Strait Islander nutrition workforce development and capacity building [208, 220, 236]. However, the workforce was reduced dramatically after the change of government in Qld in 2011 [208]. Proportionally, more nutrition professionals are now employed and there are more Aboriginal and Torres strait Islander nutrition programs in place in the NT than in other jurisdictions [208, 220].
Policies and strategies
There is a long history of effort to improve diet, nutrition and food security among Aboriginal and Torres Strait Islander people [120]. However, since the expiry of the National Aboriginal and Torres Strait Islander nutrition strategy and action plan (NATSINSAP) there has been no specific food and nutrition policy or strategy targeting these issues. The key initiatives are included below.
The National Aboriginal and Torres Strait Islander nutrition strategy and action plan (2000-2010)
The National Aboriginal and Torres Strait Islander nutrition strategy and action plan (NATSINSAP) [81] was developed following two years of wide consultation. NATSINSAP provided a framework for collaborative action across all levels of government, in partnership with industry, the non-government sector, and Aboriginal and Torres Strait Islander organisations and people. A component of the National public health nutrition strategy eat well Australia 2000-2010, the aim of NATSINSAP was to drive dietary changes to improve the nutritional status of Aboriginal and Torres Strait Islander peoples [81].
Building on existing efforts to improve access to nutritious and affordable food across urban, rural and remote communities, NATSINSAP focused on seven key areas:
- food supply in remote and rural communities
- food security and socioeconomic status
- family focused nutrition promotion, resourcing programs, disseminating and communicating ‘good practice’
- nutrition issues in urban areas
- the environment and household infrastructure
- the Aboriginal and Torres Strait Islander nutrition workforce
- national food and nutrition information systems.
An evaluation of NATSINAP was commissioned in 2009 [133] and released following a freedom of information request in March 2015 [237]. The review found that there was significant progress in some areas despite limited funding [133]. Specific achievements included:
- improved food supply in remote and rural communities, particularly through the development and implementation of the Remote Indigenous Stores and Takeaways (RIST) project that aimed to improve access to good quality, affordable, healthy foods in remote communities
- development of the Aboriginal and Torres Strait Islander nutrition workforce, including specifically through:
- inclusion of nutrition as a core component of the national Aboriginal and Torres Strait Islander Health Worker training package
- increased Aboriginal and Torres Strait Islander nutrition content, and the development of specialist Indigenous nutrition courses at five universities
- disseminating and communicating good practice, including through:
- extension of the nutrition component of Australian Indigenous HealthInfoNet
- organisation of a national Nutrition Networks Conference for Aboriginal and Torres Strait Islander nutrition and health promotion workers in Alice Springs in 2008
- advocacy for improving Aboriginal and Torres Strait Islander nutritional status.
The evaluation found that there was very little action in the areas of household food security or nutrition issues in urban areas [112], and that governance issues and inadequate resource allocation compromised the necessary operational capacity to drive implementation [133]. However, NATSINSAP did form the basis for subsequent programs and interventions [112, 220].
The evaluation recommended that “the Strategy and Action Plan be revised and updated through a consultative process, and that it be adequately funded and embedded in emerging policy frameworks with clear accountability and reporting requirements” [120, 133, 220]. This has not eventuated and coordinated implementation of NATSINSAP has ceased.
Close the Gap (2006)
The Close the Gap Aboriginal and Torres Strait Islander health campaign, led by Australia’s peak Aboriginal and Torres Strait Islander and non-Indigenous health bodies, non-government organisations and human rights organisations, brought the life expectancy gap between Aboriginal and Torres Strait Islander and non-Indigenous Australians to the public attention in 2006. In response to this campaign, the Council of Australian Governments (COAG) agreed to a policy goal of closing the gap in Aboriginal and Torres Strait Islander disadvantage in 2007 [238]. In 2008, the Close the Gap campaign partners developed a detailed set of targets at the National Indigenous Health Equity Summit, which culminated in the signing of the Close the Gap statement of Intent [239]. Among the proposed targets was that by 2018, 90% of Aboriginal and Torres Strait Islander families could access a healthy food basket for under 25% of their income [239]. This target is unlikely to be achieved, and the Close the Gap progress and priorities report 2017 states that there needs to be greater attention to nutrition and food security [240].
Closing the Gap (2008)
In response to the Close the Gap campaign, COAG developed a National Indigenous Reform Agenda. ‘Closing the Gap’ made a commitment to closing the life expectancy gap within a generation, and halving the mortality gap between Aboriginal and Torres Strait Islander and non-Indigenous children under five years of age [241, 242]. One of the agreed indicators was to reduce the prevalence of overweight and obesity [242]. Eight Indigenous-specific National Partnership Agreements were signed, and $4.6 billion was invested to improve health and its social determinants, such as housing, employment, education and early childhood development. A National strategy for remote Indigenous food security was added to the COAG agenda in December 2009 [243].
All of the Closing the Gap National Partnership Agreements have now expired, but the progress of the National Indigenous Reform Agreement continues to be monitored, and the Prime Minister releases a Closing the Gap report on progress against these targets annually [244]. A report detailing progress on the two health- related targets is also released by the Close the Gap Steering Committee and provides recommendations to the government [8].
A focus on improving nutrition has largely been omitted from the Closing the Gap responses [146, 219, 245]. One recent relevant initiative is that the 2016 Closing the Gap report [244] states that the revised Community Development Programme aims to provide opportunities for job seekers in remote communities to contribute in a range of areas, including food preparation and nutrition. However, no further details are available presently.
COAG National Strategy for Food Security in Remote Indigenous Communities (part of the National Indigenous Reform Agreement) (2009-2012)
The COAG National strategy for food security in remote Indigenous communities (the Strategy) [243] aimed to improve the food security of Aboriginal and Torres Strait Islander Australians living in remote communities through sustained coordinated action to improve the food supply and nutritious food consumption in four jurisdictions (WA, SA, NT, and Qld). It was informed by the House of Representatives Standing Committee on Aboriginal and Torres Strait Islander Affairs inquiry into remote Aboriginal and Torres Strait Islander community stores entitled Everybody’s business: remote Aboriginal and Torres Strait community stores [46]. The inquiry made over thirty recommendations to improve remote community stores. Five key actions to improve food security included the development of:
- national standards for stores and takeaways
- a national quality improvement scheme to implement the standards
- incorporation of stores under the Corporations Aboriginal and Torres Strait Islander Act
- a national healthy eating action plan
- a national workforce action plan.
Under the strategy, national standards for remote stores and takeaways were piloted in 10 locations and the National healthy eating action plan was developed but no funding was committed for implementation. The strategy expired in 2012 and was audited by the Australian National Audit Office in 2014 [246]. The audit found that the strategy was adapted for implementation in some areas, such as the SA Government’s Anangu Pitjantjatjara Yankunytjatjara Lands food security strategic plan 2011-2016 [247]. However the audit found that activities were focused mainly in the NT, where they were associated with other programs such as store licencing under the Northern Territory National Emergency Response (known as ‘the Intervention’) [248]. The audit found that resourcing of the strategy was very poor and few outcomes had been achieved [246].
National Aboriginal and Torres Strait Islander health plan 2013-2023 and Implementation plan (2015)
The National Aboriginal and Torres Strait Islander health plan (NATSIHP) 2013-2023, developed following extensive community consultation, is the current national framework to drive efforts to improve Aboriginal and Torres Strait Islander peoples’ health. Improving food access and nutrition was identified as key strategy within the 10 year plan [249]. NATSIHP aims to reduce risk factors and improve health outcomes across the life course, with priority areas including: maternal health and parenting; childhood health and development; adolescent and youth health; and healthy adults and healthy ageing. Nutrition has an important role to play at each of these life stages.
The Implementation plan [250] also identifies nutrition, particularly for pregnant women, infants and children, as a priority. However, it does not articulate specific nutrition strategies.
Instead, the Australian Government has committed to undertaking a nutrition framework gap analysis in order to identify actions to address various food and nutrition issues, including food security and maternal and child nutrition [250]. The analysis will cover a broad range of issues such as oral health, increasing knowledge and awareness, health literacy of parents, affordability, access, storage capability, the development of a ‘nutritional risk’ scheme and food security.
The Implementation plan notes that the national ‘nutritional risk’ scheme for at-risk mothers, infants and children could address issues such as: iron in the context of anaemia; folate levels; BMI; appropriate levels of weight gain in pregnancy; and healthy baby weight. No further details are available at the time of writing.
Stronger futures policy, Northern Territory (2011)
Under the Northern Territory national emergency response act 2007, now called the Stronger futures policy, all remote and community stores in Aboriginal communities in the NT must be licenced to the Australian Government [251, 252]. Under the scheme, among other requirements, stores are encouraged to adopt pricing policies to make nutritious food more accessible and affordable.
The Stronger futures policy [252] also includes the ‘income management’ of all Aboriginal people in the NT receiving welfare payments – quarantining 50% of Aboriginal people’s social security payments through a cashless ‘Basics card’. The rationale for this was to increase spending on food, groceries and other essential items and reduce spending on alcohol, tobacco, illicit drugs and gambling. An evaluation of the impact of income management was
assessed by analysis of store sales in ten remote NT communities over a three year period [253]. Key outcome measures included: trends in total store sales; sales of total food and beverage, fruit and vegetables, soft drink and tobacco. Other than a significant increase in the rate of sales for all outcome measures during a three-month government stimulus payment period, there was no apparent beneficial effect of income management on the sale of tobacco and cigarettes, soft drink or fruit and vegetables. This finding has been considered significant given that an expansion of the cashless debit card trial was announced in the 2016-17 federal budget [112].
Outback Stores (2006)
In 2006, the Commonwealth Government through Indigenous Business Australia set up the Outback Stores enterprise. The main purpose was to manage remote community stores to help ensure their commercial viability [254]. A nutrition policy has been developed for these stores. Selected sales data for fruit and vegetables and drinks are included in Outback Stores annual reports [254] and positive local stories have featured in the media [246]. However, high sales of sugary soft drinks (1.13 million litres per year) were noted during Senate Estimates in 2016 [255] and nutrition impacts in the 36 Outback Stores have not been assessed formally by independent observers [256].
Strategic priorities
Scoping study to inform the development of a new national nutrition policy
In 2012 a scoping study to inform the development of a new National nutrition policy was commissioned by the Australian Government [220]. The study was finalised in 2013 and made available publically following a freedom of information request in 2016. The evidence identified that a new comprehensive nutrition policy is required urgently to address the high and increasing rates of diet‐related disease and risk factors in Australia, (including overweight and obesity) and to promote the health and wellbeing of the population – particularly vulnerable groups including Aboriginal and Torres Strait Islander people. The study reviewed past efforts to improve Aboriginal and Torres Strait Islander nutrition and made recommendations for future action. The scoping study provided an exemplar National nutrition policy underscored by four key principles:
- food, nutrition and health
- equity
- environmental sustainability
- monitoring and surveillance, evaluation and review.
The National strategic framework for chronic conditions
The National strategic framework for chronic conditions (the Framework) is being developed by the Australian Government Department of Health in partnership with states and territories under the auspice of the Australian Health Ministers’ Advisory Council (AHMAC). It will provide a national approach to guide planning, design and delivery of policies, strategies, actions and services to reduce the impact of chronic conditions in Australia [256]. The Framework will supersede the National chronic disease strategy 2005 [257] and was due for release late 2016. It is unclear how it will articulate with other national Aboriginal and Torres Strait Islander health initiatives.
Future directions
The paradox of both over- and under-nutrition in Aboriginal and Torres Strait islander communities in Australia is a classic example of the double burden of malnutrition, described recently in the Global nutrition report [5]. Poor nutrition and diet-related chronic conditions are responsible for the largest proportion of the ill- health experienced by Aboriginal and Torres Strait Islanders [7].
Recent reviews have confirmed that efforts to improve Aboriginal and Torres Strait Islander nutrition remain fragmented, lack sufficient resources and co-ordination, and hence are largely ineffective in Australia [112, 216, 245].
Nutrition, public health and Indigenous health experts are calling for a nationwide, large scale, sustained effort to address Aboriginal and Torres Strait Islander nutrition [120, 146, 219, 245]. The recent Close the Gap progress and priorities report 2017 states specifically that there needs to be greater attention to nutrition and food security [240].
Given the very high proportion of Aboriginal and Torres Strait Islander people affected by poor diet, primary prevention through nationally coordinated, strategic, cross-sectoral policy action and legislative reform is likely to be the most cost-effective [133, 220]. Systematic, widespread, sustained implementation of evidence-based nutrition interventions is required to inform policy development [112, 140, 150, 220].
This strategy would also facilitate a focus on programs that can be complimented by broader action extending beyond the health sector, to address the social determinants of poor Aboriginal and Torres Strait Islander health, such as poverty, culture, racism, employment and education [137, 144, 146, 258, 259] . Nutrition education and skill development interventions may also be of value, particularly if they incorporate recent ethnographic evidence and reflect past and present contexts of food, support the educative role of caregivers, and support access to traditional foods [260].
However nutrition education alone will not improve nutrition [137, 142, 146, 245, 258, 259]. Increasingly, Aboriginal organisations are calling for strength-based approaches which utilise community assets to promote health and wellbeing [112, 258, 261, 262].
It is imperative to embed nutrition and food security outcomes into nationally relevant health and social policies that are current and have strong governance and accountability mechanisms. The current National Aboriginal and Torres Strait Islander health plan (NATSIHP) and Implementation plan should be used to leverage action in this regard. The development of a National framework for chronic disease [256] and potential development of a national nutrition policy or framework also provide an opportunity to explicitly consider issues and include actions to improve diet and nutrition in Aboriginal and Torres Strait Islander groups.
The NATSIHP takes a ‘whole-of-life’ approach to improving health outcomes [230, 263]. To promote pragmatic integration with this approach, priority nutrition actions would address maternal health and parenting; childhood health and development; adolescent and youth health; healthy adults; and healthy ageing. Investment in early childhood development has great potential to reduce health inequalities [112], with the benefits especially pronounced among the most vulnerable children [264]. In particular, maternal and early years education and community-based intervention programs that combine nutrition education with strategies such as growth monitoring and food provision, can improve growth and prevent hospital admissions, and are considered critical to preventing diet- related chronic conditions in later life [138, 141, 144, 265]. Similarly, programs for children and adolescents, including school-based education programs, can play an important part in providing the knowledge necessary for informed decisions about health [120].
Key priorities
Evidence based decision making must consider not only what should be done, but also how food and nutrition policies and programs should be developed to support the existing strengths of Aboriginal and Torres Strait Islander communities [112, 261]. Community control has been shown to be critical for the success of nutrition programs. To ensure sustained and effective interventions to improve nutrition also requires: an adequately trained workforce; adequate and sustained resourcing; intersectoral partnerships; a practical monitoring, research and evaluation framework; and effective dissemination.
This review has highlighted several common factors associated with successful food and nutrition programs based on principles of good practice; these are summarised in Box 4. Conversely, programs that do not have a high level of community ownership and support, or operate in isolation from, or do not address broader structural issues, such as poverty and lack of access to a healthy food supply, are unlikely to be effective [18] .
Box 4. Summary of common success factors associated with successful Aboriginal and Torres Strait Islander food and nutrition programs
Governance, staff and resources
- Establish high levels of community participation and control of project design.
- Include employment and training of specific Aboriginal or Torres Strait Islander nutrition workers.
- Ensure use of peer-education, support and role modeling.
- Build the capacity of Aboriginal or Torres Strait Islander workers and organisations.
- Involve partnerships between nutritionists (for nutrition content expertise) and Aboriginal or Torres Strait Islander workers (for cultural expertise and acceptance).
- Facilitate partnerships between organisations implementing programs and health and other sectors.
- Secure sustainable funding to enable long-term interventions rather than short-term projects.
Intervention strategies
- Apply multiple strategies in multiple settings.
- Address food security issues (availability, affordability, accessibility and acceptability of healthy food) as well as providing nutrition education.
- Include policy, regulatory and structural change to make health choices easier.
- Link screening/health assessments with health promotion programs.
- Use a participatory action research approach.
Evaluation
- Evaluate at process (was the intervention conducted as intended?), impact (was there a change in knowledge, attitudes or determinants?) and outcome (was there a change in diet, risk factors or health outcome?) levels.
- Ensure results are fed back to the community.
- Ensure results are disseminated widely.
Based on the issues and evidence presented in this review, potential interventions are highlighted in Table 3.
Table 3. Potential strategies to improve Aboriginal and Torres Strait Islander nutrition
| Intervention area | Potential Strategies |
|---|---|
| Improve food supply and availability of healthy foods | Stores
Improve store management practices, transport and stocking of healthy food. Consider community stores as essential services, like health and education, rather than small businesses. Make the development, implementation and evaluation of store nutrition policies mandatory. Use available resources, such as the Remote Indigenous Stores and Takeaway (RIST) resources (http://www.healthinfonet.ecu.edu.au/health-risks/nutrition/resources/rist). |
| Community
Reinvigorate traditional food procurement projects and local food gardens. Provide affordable, healthy community meals and takeaways through community kitchens, restaurants and/or cafes. Provide affordable, healthy breakfasts and lunches in settings such as childcare centres, kindergartens, schools, sports clubs, Home and Community Care (HACC) programs. Combine food supply interventions with culturally-appropriate nutrition education for maximum effect. Improve the quality of the food provided by Aboriginal and Torres Strait Islander organisations through the development, implementation and evaluation of catering guidelines and food supply policies. |
|
| Increase accessibility to healthy foods | Establish local programs, such as transport assistance (including shopper shuttles), food delivery and/or food aid programs in urban areas. |
| Improve housing, including food-storage, preparation and cooking facilities. | |
| Increase relative affordability of healthy food
|
Preserve and expand the current national differential taxation system (GST) to further favour competitive retail pricing of basic healthy foods. |
| Introduce a tax on sugar sweetened drinks. | |
| Introduce or expand freight subsidies to transport basic healthy foods to remote areas. | |
| Provide food supplementation/subsidisation for women, infants and children and other food insecure groups using different models, e.g. WIC-style program for pregnant and lactating women and their babies up to five years of age. This will require formal referral systems between health and welfare agencies to be effective. | |
| Subsidise provision of fruit and vegetables in schools and other settings. | |
| Expand in-store ‘cross-subsidisation’- increase ‘mark-up’ of less healthy items, and lower price margins on healthier foods. | |
| Develop pre-programmed credit card to reward healthy purchases. | |
| Enhance primary care programs | Expand prenatal, antenatal and postnatal nutrition programs, and incorporate into holistic maternal and child health care services. |
| Ensure health services provide consistent, evidence-based food and nutrition messages and breastfeeding advice [11, 266]. | |
| Expand brief nutrition interventions and early interventions in primary care, including ‘well persons’ health checks and follow-up action. | |
| Establish formal referral systems between health and welfare agencies (involves food security assessment, referral, advice and follow-up) in: Aboriginal Medical Services/primary health services; nutrition and dietetics programs; social and welfare services; aged care and disability services; home visiting programs. | |
| Conduct group-based behaviour modification programs for those at risk of diet-related chronic disease, based on effective primary care service delivery models. Link with community nutrition education, food and health literacy, budgeting and skill development (below). | |
| Introduce community nutrition education, food and health literacy, budgeting and skill development programs | Implement school-based nutrition-promotion projects. |
| Implement community food literacy and budgeting programs – ensure culturally-appropriate approaches to development, implementation, evaluation and dissemination. | |
| Enhance workforce | Create more opportunities for Aboriginal and Torres Strait Islander people to undertake vocational education and training (VET) sector and tertiary level training in nutrition – essential for a sustainable profession with increasing nutrition expertise, e.g. Accredited Practising Dietitians.
Create opportunities for a dedicated Aboriginal and Torres Strait Islander nutrition workforce. |
| Enhance training opportunities and create job opportunities and dedicated positions for Aboriginal and Torres Strait Islander peer educators to be trained and supported to work in nutrition with their local communities, adopting ‘train the trainer’ models. | |
| Enhance cultural competency training and core training of health professionals in nutrition, so as to equip non-Indigenous graduates with the knowledge and skills for working with Aboriginal and Torres Strait Islander people and communities. | |
| Include evaluation, monitoring and surveillance and dissemination
|
Develop a national, coordinated food and nutrition monitoring and surveillance system that includes an Aboriginal and Torres Strait Islander component – to assess and monitor dietary intake, nutritional status, availability, affordability, accessibility and acceptability of healthy food, and track progress. |
| Establish a national growth assessment and action system for Aboriginal and Torres Strait Islander infants and children. | |
| Ensure all nutrition programs, policies and monitoring systems are evaluated and the findings are disseminated to inform decision making and achieve improvements in policy and practice. |
Community control
All available evidence confirms that the most important factor determining the success of Aboriginal and Torres Strait Islander food and nutrition programs is community involvement in (and ideally control of) program initiation, development and implementation, with community members working in partnership in all stages of development, implementation and evaluation [18, 112, 140, 146, 267]. The most effective programs have adopted a multi-strategy approach, addressing both food supply (availability, accessibility and affordability of foods) and demand for healthy foods. Conversely, programs that do not have a high level of community ownership and support, or operate in isolation from, or do not address broader structural issues, such as poverty and lack of access to a healthy food supply, are not effective [18].
Workforce development and capacity building
A trained nutrition workforce, with excellent cross-cultural competency and communication skills, is critical to deliver effective interventions [133, 146, 232, 268]. Existing core training of non-Indigenous health professionals in nutrition must include an appropriate Aboriginal and Torres Strait Islander curriculum framework, so as to equip graduates with the knowledge and skills for working with Aboriginal and Torres Strait Islander people and communities [81, 133, 201, 232, 269]. To develop a well- supported, resourced and educated Aboriginal and Torres Strait Islander nutrition workforce, food and nutrition units should be integrated into core Aboriginal Health Worker primary health care training across the country [81, 133]. Ongoing support structures, professional development, mentoring and sustainable funding are also required to support workers to translate training into practice in their communities [229]. There is also a need for more opportunities for Aboriginal and Torres Strait Islander people to undertake tertiary level training in nutrition, essential for a sustainable profession with increasing nutrition expertise, e.g. as accredited practising dietitians and nutritionists.
Food and nutrition programs should also contribute to development of local strengths and capacities, for example, through Aboriginal or Torres Strait Islander health professionals and non-Indigenous health professionals working in partnership, and training respected community members and Elders to deliver nutrition messages [112, 262].
Other suggested strategies to build workforce capacity include:
- integrating core food and nutrition units into other specialist courses (e.g. environmental health, agriculture, store management, social work) to ensure comprehensive and collaborative work is carried out across the traditional health silos
- creating more specific nutrition positions for the Aboriginal and Torres Strait Islander workforce in all settings
- redefining the roles of health positions working with Aboriginal and Torres Strait Islander communities – positions are often quarantined to solely work in individual health behaviour change programs, failing to address broader food environmental issues that impact on nutrition and food security
- re-orientating the workforce towards ‘prevention’ activities [268]
- increasing the number of local and regional positions to extend the geographic coverage and access (increase the ‘dose’) of evidence-informed policies and programs.
Adequate and sustained resourcing
A key limitation affecting the capacity to promote and improve nutrition and food security is the ad hoc way in which many programs are funded. Many of the intervention programs described in this review were short term research or pilot projects [112, 140, 150]. This is a major barrier to sustaining nutrition and food security initiatives and their associated health outcomes. As a result, many evaluations reported that the project timeframes were too short to demonstrate changes in clinical outcomes [112, 140, 150]. This is because significant time was often needed to develop trust and build relationships in the community and adopt an ecological approach [270]. Systematic and ongoing program funding is required to address these issues effectively in the long term.
Intersectoral partnerships
While concerns around poor nutrition and poor diet-related health outcomes tend to be initiated through the health sector, it is rarely the case that health professionals in isolation have the power to intervene successfully. The engagement of partners drawn from across the food supply system is critical to address the broad reaching determinants of poor nutrition. The formation of partnerships – from ‘networking’ to formal collaboration – from different sectors, such as local government, welfare, housing and education, in addition to health and community controlled Indigenous organisations, helps build capacity to deliver quality programs and to reduce duplication and fragmentation of effort [261, 271].
Monitoring, research and evaluation
Australia currently has a mostly ad hoc food and nutrition monitoring and surveillance program, and no formal coordinated system [220, 272]. National surveys have assessed the dietary intake of either adults and/or children in 1983, 1985, 1995 and 2011-13 [273]. The 2011 to 2013 Australian health survey was the first to include specific assessment of the dietary intake and selected diet-related biomedical and food security indicators of Aboriginal and Torres Strait Islander people living in urban, rural and remote Australia. This should provide the baseline for a regular ongoing monitoring and surveillance system [120, 220]. Recommendations for an ongoing, regular, comprehensive and coordinated national food and nutrition monitoring system have been made previously [220, 272, 274].
As with broader Aboriginal and Torres Strait Islander health research [275], Indigenous nutrition research has been criticised for focusing on quantifying dietary risks and deficits, without offering clear solutions [112, 261].
Assessing the impact of published programs is usually not possible due to their short duration, small sample size and lack of control groups, and very few interventions have assessed long term health benefits. Identified barriers to rigorous evaluations of Aboriginal and Torres Strait Islander nutrition programs include: perceived inappropriateness of nutrition surveys [195]; lack of community interest in participating as a control group [193]; difficulty following up participants [191, 276]; and lack of opportunity to develop evaluation expertise among Aboriginal and Torres Strait Islander Health Workers [201].
There is a need for innovative research and evaluation to meet some knowledge gaps, particularly in food supply and access in urban settings and among some population groups, such as adolescents and older people [112, 277]. It has been suggested that a participatory action research approach may be the most appropriate [187, 195, 201].
Some successful programs have, however, been conducted and improvements in outcomes such as dietary intake, biochemical markers, weight, and waist circumference have been demonstrated [112, 140, 150]. There is a clear need to apply what is already known from these effective programs and to better translate this evidence into practice [274]. Research on what is required for a program that is successful in one community or setting to be successfully implemented in other communities or settings, and whether individual programs that show promising results in the short term are effective in the longer term, would be useful [18].
Dissemination
Dissemination of quality evaluations of food and nutrition and related interventions, with practical recommendations, are critical to help build on what has been learnt [112, 140, 150, 220]. Evaluation reports and recommendations need to be publically available for policy makers and practitioners to learn from, apply and build on.
Other considerations
Approaches to eradicating malnutrition in all its forms and its consequences need to be multi-faceted and include improved physical infrastructure, better food supplies, health and nutrition education and access to clinical care [11, 12].
To improve nutrition of infants and children, it is essential to involve carers, health workers and local community members, ensure that interventions are integrated into primary health care systems and address the underlying causes of growth problems [10, 141, 144]. To help meet gaps around programs for older people, it has been suggested that incorporating nutrition screening into Home and Community Care (HACC) services and ensuring the nutritional quality of community meal programs present opportunities [277, 278].
In urban areas, transport assistance, improved kitchen facilities, community/school gardens, organisational nutrition policies and food subsidy programs have been proposed as promising approaches [279]. In remote areas, multi-strategy programs with a strong focus on improving food supply, have been most effective [112, 140]. Recent evaluations [30, 164] highlight that promotion of all healthy foods (not just fruit and vegetables), including substantial price discounts, and complementary focus on the radical decrease of discretionary (junk) foods and sugary drinks are needed urgently.
Concluding comments
Throughout their lives, many Aboriginal and Torres Strait Islander people inequitably suffer poor health, with poor nutrition being a major contributing factor.
The underlying factor common to the growth and nutritional problems experienced by many Aboriginal and Torres Strait Islander people is extreme social disadvantage – low levels of education, high levels of unemployment, low incomes and a sub-standard physical environment including poor availability, affordability and accessibility of healthy food. A lack of food security and poor nutritional health, results in high levels of both growth impairment and overweight and obesity in childhood, and high rates of chronic disease in adulthood.
Atbirth, AboriginalandTorres Strait Islanderbabiesaresubstantially lighter than non-Indigenous babies, and the proportion of low birthweight Aboriginal and Torres Strait Islander babies is much higher than among other Australians. From birth, the growth of most Aboriginal and Torres Strait Islander infants tends to be satisfactory until around six months of age, at which time they need healthy foods to complement breastfeeding, and become more directly exposed to the substandard environment and socio-economic conditions in which many Aboriginal and Torre Strait Islanders live. At this time, many enter a vicious synergistic cycle of infection-malnutrition. Many Aboriginal and Torres Strait Islander people carry this legacy of impaired growth and poor nutritional status into early adulthood, where it is associated with development of chronic disease in later life and has a significant impact on the health of mothers, and of the next generation.
Over recent decades, there has been a rapid rise among Aboriginal and Torres Strait Islander Australians of diet-related chronic disorders such as obesity, cardiovascular disease, type 2 diabetes and chronic renal disease and their complications. From adolescence, and increasingly even earlier, many Aboriginal and Torres Strait Islander people start to gain weight excessively, eventually becoming overweight or obese. This has contributed to alarming levels of diet-related chronic disease.
The diets of Aboriginal and Torres Strait Islanders are typically lower in vegetables, fruit, wholegrain cereals and other healthy foods, but higher in discretionary, or ‘junk’ foods and drinks than other Australians. This is underscored by the relatively poor availability, affordability and accessibility of healthy foods for Aboriginal and Torres Strait Islander communities throughout Australia.
Numerous programs and interventions have been implemented at national, state and community levels to improve nutrition status among AboriginalandTorres Strait Islanderpeoples. Severalofthese have resulted in objective dietary and biomedical improvement,
and have provided useful insights into what works and what more is needed to improve Aboriginal and Torres Strait Islander nutrition and health. Those that achieve the greatest success are invariably those that are developed with the target communities, are culturally appropriate and are tailored to community needs. However, recent reviews have confirmed that current efforts to improve Aboriginal and Torres Strait Islander nutrition are often fragmented, lack sufficient resources and co-ordination, and thus do not achieve the expected outcomes. Another key feature of many successful interventions is the recruitment, training and support of Aboriginal Health Workers and capacity-building in the communities.
In view of the central role that nutrition and diet-related diseases will play in addressing at least two of the targets set for ‘closing the gap’ between Aboriginal and Torres Strait Islander and non- Indigenous people – to halve the 11-year gap in life expectancy within a generation, and to halve the gap in infant and childhood mortality within a decade – it is clear that commitments to redressing the underlying social disadvantages experienced by many Aboriginal and Torres Strait Islander people will need to be accompanied by expansion of key nutrition initiatives.
It is imperative that Australia continues to develop national, coordinated, strategic, cross-sectoral policies and legislative reforms to address the nutrition, food security and diet-related health of Aboriginal and Torres Strait Islander peoples. This should build on proven approaches and be developed with Aboriginal and Torres Strait Islander people in a way that strengthens and supports culture and capacity. Commitment and partnership across a range of government and industry bodies will be necessary to tackle the factors contributing to poor nutrition and diet-related health of Aboriginal and Torres Strait Islander peoples effectively.
All available evidence confirms that effective nutrition interventions are feasible and have huge potential to influence long term improvements in nutrition and diet-related health of Aboriginal and Torres Strait Islanders.
A first step will be to progress nutrition deliverables within the National Aboriginal and Torres Strait Islander health plan’s (NATSIHP) Implementation plan, specifically the Nutrition framework gap analysis and Nutritional risk scheme. However, there is an urgent need for practical, specific nutrition and food security strategies, actions and deliverables to be incorporated within the social and cultural determinants of health domain of the NATSIHP’s Implementation plan.
Experts are also expressing an urgent need to develop, fund and implement a National nutrition policy (or Framework) that explicitly incorporates and addresses Aboriginal and Torres Strait Islander peoples’ nutrition and food security issues.
Appendix 1. The Australian Dietary Guidelines
| Guideline 1 | To achieve and maintain a healthy weight, be physically active and choose amounts of nutritious food and drinks to meet your energy needs.
|
| Guideline 2 | Enjoy a wide variety of nutritious foods from these five groups every day:
And drink plenty of water. |
| Guideline 3 | Limit intake of foods containing saturated fat, added salt, added sugars and alcohol.
|
| Guideline 4 | Encourage, support and promote breastfeeding. |
| Guideline 5 | Care for your food; prepare and store it safely. |
Source: National Health and Medical Research Council, 2013 [11]
Appendix 2. The Aboriginal and Torres Strait Islander Guide to Healthy Eating
Source: National Health and Medical Research Council, 2015 [280]
Appendix 3: Data sources and limitations
The two major data limitations in Aboriginal and Torres Strait Islander nutrition are data gaps and bias.
Dietary data
The execution of the National Aboriginal and Torres Strait Islander nutrition and physical activity survey (NATSINPAS) 2011-2013, a component of the Australian health survey 2011-13, was the first time nationally representative food and nutrition data and related biomedical data for Aboriginal and Torres Strait Islander people had been collected [6]. As noted by the AIHW [10], available data are too sparse to produce consistent time series, to regularly assess changes in dietary risk factors, or explain their contribution to the health gaps between the Aboriginal and Torres Strait Islander and non-Indigenous populations, and the health inequities within the Aboriginal and Torres Strait Islander population. Some data items are collected only from Aboriginal and Torres Strait Islander people living in non-remote locations.
Numbers of Aboriginal and Torres Strait Islander participants in the NATSINPAS 2011-2013 [14, 92] were too small to produce reliable estimates of the prevalence of risk factors in Aboriginal groups compared with Torres Strait Islander groups. However some metrics, for example, anthropometry and intake of some foods, such as seafood, are known to be very different in each of these populations [11].
The Australian Bureau of Statistics (ABS) has noted that significant under-reporting of dietary intake is likely in both the 2012-13 NATSINPAS and 2011-12 National nutrition and physical activity survey (NNPAS) [281]. There appears to be a higher rate of under- reporting in the NATSINPAS (mean energy missing 27%), for both males (mean energy missing 24%) and females (mean energy missing 31%), than in the NNPAS (mean energy missing 19%). Under-reporting appears to be more prevalent among females than males, increases with age and increases as BMI increases [281].
Also, the ABS note [281] that given the association of under- reporting with overweight/obesity and consciousness of socially acceptable/desirable dietary patterns, under-reporting is unlikely to affect all foods and nutrients equally; that is, people are likely to over-report healthy foods and under-report discretionary foods. A recent study comparing dietary estimates from the NATSINPAS to food and beverage purchase data has confirmed such likely self- reporting bias [282].
Very limited data are collected regularly on Aboriginal and Torres Strait Islander food and nutrition in Australia. The regular Aboriginal and Torres Strait Islander health survey reported by the AIHW collects only data on intake of number of serves per day of fruit and vegetables by self-reported methods in non-remote areas [6]. Such self-reported dietary intakes have been shown to be highly unreliable in Aboriginal communities [86] and these data are likely to be over-estimated for the reasons outlined by the ABS [281].
Little recent data are available concerning the full range of nutrition issues, such as infant growth or risk factors for poor pregnancy. Data for specific age/gender groups are also sparse, such as for adolescents and older Aboriginal and Torres Strait Islander groups. For example, despite the prominence of Fetal alcohol spectrum disorder (FASD), current data on alcohol use in pregnancy are from the National drug strategy household survey and thus are based only on a small number of pregnant women; due to the sample size, further disaggregation (for example, by Indigenous status, remoteness or socioeconomic position) is not possible [10].
Food security
Over 20 years ago the Australian national nutrition survey (1995) included a single question around individual food security: ‘In the last 12 months, were there any times that you ran out of food and couldn’t afford to buy any more?’ [283]. A similar question was again included in the 2004-05 National Aboriginal and Torres Strait Islander health survey (NATSIHS) which collected information from 10,439 Aboriginal and Torres Strait Islander people from remote and non-remote areas across Australia [284]. While a useful indicator, it is likely to underestimate the degree or nature of food security problems, as the question only addresses one aspect of food security (running out of food as a result of running out of money). It has also not been possible from this limited information to isolate nutrition and food security data for the majority of Aboriginal and Torres Strait Islander people that live in urbanised environments. There is a need to better understand food insecurity from an Aboriginal and Torres Strait Islander perspective and to develop specific tools for assessment.
Monitoring activities can focus, as in the above example, on measuring the prevalence of food security for particular groups (that is quality of food, shortage of food, experiences of hunger, anxiety about food intake). Another approach is to assess the determinants of food security, in relation to the factors which impact ‘food supply’ and ‘food access’. Examples here may include:
- documenting the price, availability, quality and promotion of food in community retails outlets
- mapping the location of supermarkets and other food outlets in relation to residential areas
- monitoring the uptake of food aid programs.
Anthropometry
In the 2012–13 AATSIHS, measures of height and weight were collected to determine BMI. These measured BMI data for 2012–13 are not comparable with previous ABS national Aboriginal and Torres Strait Islander health surveys or national health surveys, in which BMI were mainly based on (highly unreliable) self-reported height and weight [10, 67] . However, several reports compare these data [10].
Representativeness of sampling is also a challenge in interpreting survey results. In the 2012–13 AATSIHS, BMI was only calculated for people for whom both height and weight were measured. In 2012–13, 80.6% of Aboriginal and Torres Strait Islander people aged two years and over had their height and weight recorded. Height and weight measurements were obtained from 76.7% of Aboriginal and Torres Strait Islander children aged 2–14 years, and 82.5% of Aboriginal and Torres Strait Islander people aged 15 years and over [10].
There is a lack of national growth data for Aboriginal and Torres Strait Islander infants in Australia; such data are collected, analysed and reported routinely only in the NT [274].
Implication of data issues
Gaps and bias in food, nutrition and diet-related data for Aboriginal and Torres Strait Islander groups in Australia can have serious policy implications.
These data have been used to inform burden of disease studies [70] and policy actions [242, 243, 250] and can lead to incorrect conclusions and unsatisfactory decisions. For example, in 2004-05, when self-reported data were collected to inform the development of the Closing the Gap targets [242], 42% of Aboriginal and Torres Strait Islander people aged fifteen years or over reported consuming the recommended daily intake for fruit and 10% reported consuming the recommended daily intake for vegetables. There were no significant differences between the proportion of Aboriginal and Torres Strait Islander (11%) and non- Indigenous people (13%) who reported meeting other relevant dietary recommendations; and the nutrition gap was deemed subsequently to be non-existent [146, 219]. However the questions asked had not been validated for application in Aboriginal and Torres Strait Islander groups, and it is unclear to what degree social desirability may have led to response bias. Self-reported data do not match the low levels of intake described consistently from application of more reliable quantitative methods. Further, self- reported fruit and vegetable intakes do not represent the entirety of nutrition and dietary issues affecting Aboriginal and Torres Strait Islander people. Hence the decision to effectively exclude nutrition from Closing the Gap was made on inaccurate data.
The lack of a collection of nationally co-ordinated growth data, or growth assessment and actions programs, for Aboriginal and Torres Strait Islander infants in Australia is a critical gap in the development of effective intervention policies. For example, owing to significant gaps in available data, Australia is not included in United Nations Children’s Fund (UNICEF) reports relevant to First Nations children, including The children left behind: a league table of inequality in child well-being in the world’s rich countries [285]. This report is important for many First Nations children who experience conditions near the bottom of the table, because it focuses attention on the need for resources and programs to close the equity gap [274].
Lack of data also makes it impossible to report against standard global nutrition indicators, particularly for infants and children [274]. In particular, few of the nutrition indicators in the Global nutrition report [5] can be reported for Australia; hence it is impossible to make meaningful international comparisons.
The need to develop reliable national nutrition and food security indicators and an effective monitoring and surveillance system has been highlighted repeatedly [220, 272]. This was identified in the NATSINSAP under the Key Action area: National food and nutrition information systems [81] re-iterated in resolutions from the 2008 National Nutrition Networks conference [233] and included in recommendations of the evidence-based scoping study for a new nutrition policy in Australia [220].
The limited monitoring of diet, nutrition and food supply and food security status, particularly among the Aboriginal and Torres Strait Islander population, but also across mainstream Australia, has restricted awareness of the significance of nutrition issues and concerted policy action to address these.
References
- O’Dea K (1984) Marked improvement in carbohydrate and lipid metabolism in diabetic Australian Aborigines after temporary reversion to traditional lifestyle. Diabetes;33:596-603
- United Nations General Assembly (2016) United Nations decade of action on nutrition (2016-2025). Geneva: United Nations General Assembly
- Northern Territory Department of Health Data Management and System Reporting Branch (2015) Healthy Under 5 Kids Program: Growth and Nutrition Report: NT Annual Report 2015. Darwin: Northern Territory Department of Health
- World Health Organization (2006) WHO child growth standards – length/height-for-age, weight-for-age, weight-for-length, weightfor- height and body mass index-for-age: methods and development. Geneva: World Health Organization
- Global Nutrition Report (2016) Global Nutrition Report. Retrieved 2016 from http://www.globalnutritionreport.org/
- Australian Institute of Health and Welfare (2015) The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples 2015. (AIHW Catalogue no IHW 147) Canberra: Australian Institute of Health and Welfare
- Australian Institute of Health and Welfare (2016) Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. (Australian Burden of Disease Study series no. 6, Cat no. BOD 7) Canberra: Australian Institute of Health and Welfare
- Australian Health Ministers’ Advisory Council (2015) Aboriginal and Torres Strait Islander health performance framework 2014 report. Canberra: Department of the Prime Minister and Cabinet
- de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C (2007) Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization;(85):660-667
- Australian Institute of Health and Welfare (2016) Australia’s health 2016. Canberra: Australian Institute of Health and Welfare
- National Health and Medical Research Council (2013) Australian Dietary Guidelines: providing the scientific evidence for healthier Australian diets. Canberra: National Health and Medical Research Council
- National Health and Medical Research Council (2000) Nutrition in Aboriginal and Torres Strait Islander peoples: an information paper. Canberra: National Health and Medical Research Council
- Australian Institute of Health and Welfare (2015) Aboriginal and Torres Strait Islander health performance framework 2014 report: detailed analyses. (AIHW Cat. no. IHW 167) Canberra: Australian Institute of Health and Welfare
- Australian Bureau of Statistics (ABS) (2016) Australian Aboriginal and Torres Strait Islander Health Survey: consumption of food groups from the Australian Dietary Guidelines, 2012-13. (4727.0.55.008) Canberra: Australian Bureau of Statistics (ABS)
- Australian Bureau of Statistics (2015) Australian Aboriginal and Torres Strait Islander health survey: nutrition results – food and nutrients, 2012-13. (ABS cat. no. 4727.0.55.005) Canberra: Australian Bureau of Statistics
- Australian Bureau of Statistics (2016) Australian Health Survey: consumption of food groups from the Australian Dietary Guidelines, 2011-12. (ABS Cat. no. 4364.0.55.012) Canberra: Australian Bureau of Statistics
- National Health and Medical Research Council (2012) Infant feeding guidelines: information for health workers. Canberra: National Health and Medical Research Council
- Closing the Gap Clearinghouse (2012) Healthy lifestyle programs for physical activity and nutrition. (Closing the Gap Clearinghouse resource sheet no. 9) Canberra: Closing the Gap Clearinghouse
- Sebastian T, Donelly M (2013) Policy influences affecting the food practices of Indigenous Australians since colonisation. Australian Aboriginal Studies;(2):59-75
- Rasmussen M, Guo X, Wang Y, Lohmueller KE, Rasmussen S, Albrechtsen A, Skotte L, Lindgreen S, Metspalu M, Jombart T, Kivisild T, Zhai W, Eriksson A, Manica A, Orlando L, De La Vega FM, Tridico S, Metspalu E, Nielsen K, Avila-Arcos MC, Moreno-Mayar JV, Muller C, Dortch J, Gilbert MTP, Lund O, Wesolowska A, Karmin M, Weinert LA, Wang B, Li J, Tai S, Xiao F, Hanihara T, Van Driem G, Jha AR, Ricaut F-X, De Knijff P, Migliano AB, Romero IG, Kristiansen K, Lambert DM, Brunak S, Forster P, Brinkmann B, Nehlich O, Bunce M, Richards M, Gupta R, Bustamante CD, Krogh A, Foley RA, Lahr MM, Balloux F, Sicheritz-Ponten T, Villems R, Nielsen R, Wang J, Willerslev E (2011) An Aboriginal Australian genome reveals separate human dispersals into Asia. Science;334(6052):94-98
- Saggers S, Gray D (1991) Aboriginal health and society: the traditional and contemporary Aboriginal struggle for better health. North Sydney: Allen and Unwin
- O’Dea K, Jewell PA, Whiten A, Altmann SA, Strickland SS, Oftedal OT (1991) Traditional diet and food preferences of Australian Aboriginal hunter-gatherers. Philosophical Transactions of the Royal Society B;334(1270):233-241
- Lee AJ (1996) The transition of Australian Aboriginal diet and meal patterns. World Review of Nutrition and Dietetics;79:1-52
- Lee A, O’Dea K (2015) Aboriginal and Torres Strait Islander nutrition and health. In: Croxford S, Itsiopoulous C, Forsyth A, Belski R, Thodis A, Shepherd S, eds. Nutrition through the life stages : a comprehensive overview of food and nutrition in all stages of life. Crows Nest, N.S.W.: Allen and Unwin:261-276
- Leonard D, Beilin R, Moran M (1995) Which way kaikai blo umi? Food and nutrition in the Torres Strait. Australian Journal of Public Health;19(6):589-595
- Gracey M (2000) Historical, cultural, political, and social influences on dietary patterns and nutrition in Australian Aboriginal children. American Journal of Clinical Nutrition;72(5 [Supp]):1361S-1367S
- Blainey G (1975) Triumph of the nomads: a history of ancient Australia. South Melbourne, Vic: Macmillan
- Franklin M, White I (1991) The history and politics of Aboriginal health. In: Reid J, Trompf P, eds. The health of Aboriginal Australia. Marrickville: Harcourt Brace Jovanovich Group [Australia] Pty Ltd:1- 36
- O’Dea K, White N, Sinclair A (1988) An investigation of nutritionrelated risk factors in an isolated Aboriginal community in Northern Australia: advantages of a traditionally-orientated life-style. Medical Journal of Australia;148:177-180
- Lee A, Rainow S, Tregenza J, Tregenza L, Balmer L, Bryce S, Paddy M, Sheard J, Schomburgk D (2015) Nutrition in remote Aboriginal communities: lessons from Mai Wiru and the Anangu Pitjantjatjara Yankunytjatjara Lands. Australian and New Zealand Journal of Public Health;40(S1):S81–S88
- Australian Bureau of Statistics (2014) Australian Aboriginal and Torres Strait Islander health survey: updated results, 2012–13. (ABS Catalogue no. 4727.0.55.006) Canberra: Australian Bureau of Statistics
- Australian Bureau of Statistics (2016) National Aboriginal and Torres Strait Islander Social Survey, 2014-15. Canberra: Australian Bureau of Statistics
- Kettings C, Sinclair AJ, Voevodin M (2009) A healthy diet consistent with Australian health recommendations is too expensive for welfare-dependent families. Australian and New Zealand Journal of Public Health;33(6):566-572
- Lee AJ, Kane S, Ramsey R, Good E, Dick M (2016) Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia. BMC Public Health 16.
- Lee A, Mhurchu CN, Sacks G, Swinburn B, Snowdon W, Vandevijvere S, Hawkes C, L’Abbe M, Rayner M, Sanders D, Barquera S, Friel S, Kelly B, Kumanyika S, Lobstein T, Ma J, Macmullan J, Mohan S, Monteiro C, Neal B, Walker C (2013) Monitoring the price and affordability of foods and diets globally. Obesity Reviews;14(S1):82-95
- Lewis M, Lee A (2016) Costing ‘healthy’ food baskets in Australia – a systematic review of food price and affordability monitoring tools, protocols and methods. Public Health Nutrition;19(6):2872-2886
- Brimblecombe JK, O’Dea K (2009) The role of energy cost in food choices for an Aboriginal population in northern Australia. Medical Journal of Australia;190(10):549-551
- Ferguson M, O’Dea K, Holden S, Miles E, Brimblecombe J (2016) Food and beverage price discounts to improve health in remote Aboriginal communities: mixed method evaluation of a natural experiment. Australian and New Zealand Journal of Public Health;Early View(http:// dx.doi.org/10.1111/1753-6405.12616):1-6
- Carlson A, Frazao E (2012) Are healthy foods really more expensive? It depends on how you measure the price. USDA-ERS Economic Information Bulletin;(96):50
- Barosh L, Friel S, Engelhardt K, Chan L (2014) The cost of a healthy and sustainable diet – who can afford it? Australian and New Zealand Journal of Public Health;38(1):7-12
- Healthabitat (2016) Healthabitat: environmental health and design. Retrieved 2016 from http://www.healthabitat.com/
- Healthabitat (2013) Housing for Health – the guide. Improving nutrition: the ability to store, prepare and cook food. Retrieved 2013 from http://www.housingforhealth.com/the-guide/health-housing/ improving-nutrition-the-ability-to-store-prepare-and-cook-food/
- Begg S, Vos T, Barker B, Stevenson C, Stanley L, Lopez A (2007) The burden of disease and injury in Aboriginal and Torres Strait Islander peoples 2003. Brisbane: Centre for Burden of Disease and Cost- Effectiveness, School of Population Health, University of Queensland
- Leonard D, Turner C, Hobson V, Pollard C, Lewis J, Bowcock R (2003) FoodNorth: food for health in north Australia. Perth: North Australia Nutrition Group, Department of Health, Western Australia
- Landrigan T, Pollard C (2011) Food Access and Cost Survey (FACS) Western Australia, 2010. Perth, WA: Department of Health, Western Australia
- House of Representatives Aboriginal and Torres Strait Islander Affairs Committee (2009) Everybody’s business: remote Aboriginal and Torres Strait community stores. Canberra: The Parliament of the Commonwealth of Australia
- Pollard CM, Nyaradi A, Lester M, Sauer K (2014) Understanding food security issues in remote Western Australian Indigenous communities. Health Promotion Journal of Australia;25(2):83-89
- Harrison M, Lee A, Findlay M, Nicholls R, Leonard D, Martin C (2010) The increasing cost of healthy food. Australian and New Zealand Journal of Public Health;34(2):179-186
- Pollard CM, Landrigan TM, Ellies PL, Kerr DA, Lester MLU, Goodchild SE (2014) Geographic factors as determinants of food security: a Western Australian food pricing and quality study. Asia Pacific Journal of Clinical Nutrition;23(4):703-713
- Brimblecombe J, Ferguson M, Liberato SC, O’Dea K, Riley M (2013) Optimisation modelling to assess cost of dietary improvement in remote Aboriginal Australia. PLOS ONE 8.
- Lee A (1996) The effect of retail store managers on Aboriginal diet in remote communities. Australian and New Zealand Journal of Public Health;20:212-214
- Stewart I (1997) Research into the cost, availability and preferences for fresh food compared with convenience food items in remote area Aboriginal communities: final report. Canberra: Roy Morgan Research
- Arnhem Land Progress Aboriginal Corporation (2017) Arnhem Land Progress Aboriginal Corporation. Retrieved 2017 from https://www. alpa.asn.au/
- Outback Stores (2017) Outback Stores: working with communities. Retrieved 2017 from http://outbackstores.com.au/
- Mai Wiru Regional Stores Council (2017) Mai Wiru Regional Stores Council. Retrieved 2017 from http://www.maiwiru.org.au/
- Northern Territory Department of Health (2014) Northern Territory market basket survey 2014. Darwin: Northern Territory Department of Health
- World Health Organization (2015) Guideline: sugars intake for adults and children. Geneva: World Health Organization
- National Health and Medical Research Council (2013) Eat for Health: educator guide. Canberra: National Health and Medical Research Council
- Barker DJP, Eriksson JG, Forsen T, Osmond C (2002) Fetal origins of adult disease: strength of effects and biological basis. International Journal of Epidemiology;31(6):1235-1239
- Lynch J, Smith GD (2005) A life course approach to chronic disease epidemiology. Annual Review of Public Health;26(2005):1-35
- Langley-Evans SC (2014) Nutrition in early life and the programming of adult disease: a review. Journal of Human Nutrition and Dietetics;28(Supplement s1):1-14
- Australian Institute of Health and Welfare (2016) Australia’s mothers and babies 2014: in brief. Canberra: Australian Institute of Health and Welfare
- Australian Institute of Health and Welfare (2013) Aboriginal and Torres Strait Islander health performance framework 2012: detailed analyses. (AIHW Cat. no. IHW 94) Canberra: Australian Institute of Health and Welfare
- Gracey MS (2007) Nutrition-related disorders in Indigenous Australians: how things have changed. Medical Journal of Australia;186(1):15-17
- Kearns T, Liberato S, Ward F (2014) Childhood anaemia knowledge and resource development project report. Darwin: Menzies School of Health Research
- Apunipima Cape York Health Council (2016) Anaemia in young children of Cape York: results of a chart audit. Cape York, Qld: Apunipima Cape York Health Council
- Australian Bureau of Statistics (2013) Australian Aboriginal and Torres Strait Islander health survey: first results, Australia, 2012-13. (ABS Catalogue no. 4727.0.55.001) Canberra: Australian Bureau of Statistics
- Young JK, Giesbrecht HE, Eskin MN, Aliani M, Suh M (2014) Nutrition implications for fetal alcohol spectrum disorder. Advances in Nutrition;5(2014):675-692
- Sayers S, Powers J (1997) Risk factors for Aboriginal low birthweight, intrauterine growth retardation and preterm birth in the Darwin health region. Australian and New Zealand Journal of Public Health;21(5):524-530
- Australian Institute of Health and Welfare (2015) Australian Burden of Disease Study: fatal burden of disease in Aboriginal and Torres Strait Islander people 2010. (Australian Burden of Disease Study series 2. Cat. no. BOD 02) Canberra: Australian Institute of Health and Welfare
- World Health Organization (2013) Exclusive breastfeeding. Retrieved 2013 from http://www.who.int/nutrition/topics/exclusive_ breastfeeding/en/
- Australian Institute of Health and Welfare (2011) 2010 Australian national infant feeding survey: indicator results. (AIHW Catalogue no PHE 156) Canberra: Australian Institute of Health and Welfare
- Helps C, Barclay L (2015) Aboriginal women in rural Australia; a small study of infant feeding behaviour. Women and Birth;In press(http:// dx.doi.org/10.1016/j.wombi.2014.12.004)
- Rogers L (2006) Understanding barriers to breastfeeding in Aboriginal and Torres Strait Islander women. Aboriginal and Islander Health Worker Journal;30(1):8-9, 32
- Footprints in Time (2015) Footprints in Time: the longitudinal study of Indigenous children: report from Wave 5. Canberra: Department of Social Services
- Bruce KD, Hanson MA (2010) The developmental origins, mechanisms, and implications of metabolic syndrome. The Journal of Nutrition;140(3):648-652
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, Sachdev HS (2008) Maternal and child undernutrition: consequences for adult health and human capital. The Lancet;371(9609):340-357
- Rolland-Cachera M, Peneau S (2011) Assessment of growth: variations according to references and growth parameters used. American Journal of Clinical Nutrition;94(6 Suppl):1794S-1798S
- Sayers SM, Mackerras D, Singh G, Bucens I, Flynn K, Reid A (2003) An Australian Aboriginal birth cohort: a unique resource for a life course study of an Indigenous population: a study protocol. BMC International Health and Human Rights;3(1):1472-1698
- Northern Territory Department of Health Data Management and Sysem Reporting Branch (2015) Healthy Under 5 Kids Program: Growth and Nutrition Report: NT Annual Report 2015. Darwin: Northern Territory Department of Health
- National Public Health Partnership (2001) National Aboriginal and Torres Strait Islander Nutrition Strategy and Action Plan 2000-2010 and first phase activities 2000-2003. Canberra: National Public Health Partnership
- Webster V, Denney-Wilson E, Knight J, Comino E, Gudaga Research Team (2013) Describing the growth and rapid weight gain of urban Australian Aboriginal infants. Journal of Paediatrics and Child Health;49(4):303–308
- Hardy LL, O’Hara BJ, Hector D, Engelen L, Eades SJ (2014) Temporal trends in weight and current weight-related behaviour of Australian Aboriginal school-aged children. Medical Journal of Australia;200(11):667-671
- Wake M, Hardy P, Canterford L, Sawyer M, Carlin JB (2007) Overweight, obesity and girth of Australian preschoolers: prevalence and socioeconomic correlates. International Journal of Obesity;31(7):1044-1051
- Valery PC, Ibiebele T, Harris M, Green AC, Cotterill A, Moloney A, Sinha AK, Garvey G (2012) Diet, physical activity, and obesity in school-aged Indigenous youths in northern Australia. Journal of Obesity 2012.
- Lee A, Smith A, Bryce S (1995) Measuring dietary intake in remote Australian Aboriginal communities. Ecology of Food and Nutrition;34:19-31
- Liberato SC, Kearns T, Ward F, Brimblecombe J (2016) Use of electronic visual recording to aid assessment of dietary intake of Australian Aboriginal children living in remote communities. Australian and New Zealand Journal of Public Health;40(S1):S27–S29
- Thurber KA, Banwell C, Neeman T, Dobbins T, Pescud M, Lovett R, Banks E (2016) Understanding barriers to fruit and vegetable intake in the Australian Longitudinal Study of Indigenous Children: a mixed-methods approach. Public Health Nutrition;Firstview(http:// dx.doi.org/10.1017/S1368980016003013)
- Australian Bureau of Statistics (2014) Australian health survey: nutrition first results – foods and nutrients, 2011-12. (ABS Catalogue no 4364.0.55.007) Canberra: Australian Bureau of Statistics
- Australian Bureau of Statistics (2016) Australian Aboriginal and Torres Strait Islander Health Survey: consumption of food groups from the Australian Dietary Guidelines, 2012-13. (4727.0.55.008) Canberra: Australian Bureau of Statistics
- Australian Bureau of Statistics (2014) Australian Aboriginal and Torres Strait Islander health survey: updated results, 2012-13: table 13 [data cube]. Retrieved 6 June 2014 from http://www.abs.gov. au/AUSSTATS/subscriber.nsf/log?openagent&472705500613. xls&4727.0.55.006&Data%20Cubes&D751183318983C51CA257CEE 0010D97D&0&2012%9613&06.06.2014&Latest
- Australian Bureau of Statistics (2015) Australian Dietary Guidelines and Price Indexes. Canberra: Australian Bureau of Statistics
- Australian Bureau of Statistics (ABS) (2016) Australian Aboriginal and Torres Strait Islander Health Survey: consumption of added sugars, 2012-13. (4727.0.55.009) Canberra: Australian Bureau of Statistics (ABS)
- Ferguson M, Brown C, Georga C, Miles E, Wilson A, Brimblecombe J (2017) Traditional food availability and consumption in remote Aboriginal communities in the Northern Territory, Australia. Australian and New Zealand Journal of Public Health;Early view(http:// dx.doi.org/10.1111/1753-6405.12664)
- Australian Bureau of Statistics (2015) Australian Aboriginal and Torres Strait Islander health survey: nutrition results – food and nutrients, 2012-13: Table 12.1 [data cube]. Retrieved 20 March 2015 from http://www.abs.gov.au/ausstats/subscriber.nsf/log?o penagent&4727055005_201213_12.xls&4727.0.55.005&Data%20 Cubes&2DC1BC4A0840357FCA257E0D000ECE96&0&2012- 13&20.03.2015&Latest
- McMahon E, Webster J, O’Dea K, Brimblecombe J (2015) Dietary sodium and iodine in remote Indigenous Australian communities: will salt-reduction strategies increase risk of iodine deficiency? A cross-sectional analysis and simulation study. BMC Public Health 15.
- Australian Bureau of Statistics (2014) Australian Aboriginal and Torres Strait Islander health survey: biomedical results, 2012-13. (ABS Catalogue no 4727.0.55.003) Canberra: Australian Bureau of Statistics
- World Health Organization (2013) Obesity and overweight: fact sheet no 311. World Health Organization. Retrieved March 2013 from http://www.who.int/mediacentre/factsheets/fs311/en/
- World Health Organization (2011) Waist circumference and waist–hip ratio: report of a WHO expert consultation Geneva. Retrieved March 2017 from http://www.who.int/nutrition/publications/obesity/ WHO_report_waistcircumference_and_waisthip_ratio/en/
- Gracey M, Burke V, Martin DD, Johnston RJ, Jones T and Davis EA (2007) Assessment of risks of “lifestyle” diseases including cardiovascular disease and type 2 diabetes by anthropometry in remote Australian Aborigines. Asia Pacific Journal of Clinical Nutrition;16(4):688-697
- Li M and McDermott RA (2010) Using anthropometric indices to predict cardio-metabolic risk factors in Australian Indigenous populations. Diabetes Research and Clinical Practice;87(3):401-406
- Daniel M, Rowley K, McDermott R and O’Dea K (2002) Diabetes and impaired glucose tolerance in Aboriginal Australians: prevalence and risk. Diabetes Research and Clinical Practice;57:23-33
- Hughes JT, Maple-Brown LJ, Piers LS, Meerkin J, O’Dea K and Ward LC (2015) Development of a single-frequency bioimpedance prediction equation for fat-free mass in an adult Indigenous Australian population. European Journal of Clinical Nutrition;69(1):28–33
- Lee A, O’Dea K, Mathews J (1994) Apparent dietary intake in remote Aboriginal communities. Australian Journal of Public Health;18(2):190-197
- Lee A, Bailey A, Yarmirr D, O’Dea K, Mathews J (1994) Survival tucker: improved diet and health indicators in an Aboriginal community. Australian Journal of Public Health;18(3):277-285
- Wycherley T, Ferguson M, O’Dea K, McMahon E, Liberato S, Brimblecombe J (2016) Store turnover as a predictor of food and beverage provider turnover and associated dietary intake estimates in very remote Indigenous communities. Australian and New Zealand Journal of Public Health;Early view(http://dx.doi.org/10.1111/1753- 6405.12571)
- Brimblecombe JK, Ferguson MM, Liberato SC, O’Dea K (2013) Characteristics of the community-level diet of Aboriginal people in remote northern Australia. Medical Journal of Australia;198(7):380-384
- Hoy W, Manning R, Tungatalum L, Hoy P, Mott S, Eddy DD, Ball PA (2014) A profile of sales audits of a remote Aboriginal community’s general store: 1992 and 2011 [letter]. Australian and New Zealand Journal of Public Health;38(1):94
- Urapuntja Health Service (1990) Urapuntja Health Service health survey. Alice Springs: Institute for Aboriginal Development
- Haswell-Elkins M, McGrath V, Moore M, Satarug S, Walmby M, Ng J (2007) Exploring potential dietary contributions including traditional seafood and other determinants of urinary cadmium levels among indigenous women of a Torres Strait Island (Australia). Journal of Exposure Science and Environmental Epidemiology;17(3):298-306
- Lawrence CG (2013) The urgency of monitoring salt consumption and its effects in Aboriginal and Torres Strait Islander Australians. Medical Journal of Australia;198(7):365-366
- Browne J, Adams K, Atkinson P (2016) Food and nutrition programs for Aboriginal and Torres Strait Islander Australians: what works to keep people healthy and strong? (Issues Brief No. 17) Canberra: Deeble Institute for Health Policy Research
- Guest CS, O’Dea K (1992) Diabetes in Aborigines and other Australian populations. Australian Journal of Public Health;16(4):340-349
- Whalan S, Farnbach S, Volk L, Gwynn J, Lock M, Trieu K, Brimblecombe J, Webster J (2017) What do we know about the diets of Aboriginal and Torres Strait Islander peoples in Australia? A systematic literature review. Australian and New Zealand Journal of Public Health;Early view(https://doi.org/10.1111/1753-6405.12721)
- Food and Agriculture Organisation of the United Nations (1996) Rome Declaration on World Food Security and the World Food Summit Plan of Action. Retrieved 1996 from http://www.fao.org/docrep/003/ w3613e/w3613e00.HTM
- Davy D (2016) Australia’s efforts to improve food security for Aboriginal and Torres Strait Islander peoples. Health and Human Rights;18(2):209-218
- United Nations (1948) Universal Declaration of Human Rights. Geneva: United Nations
- Eide WB, Kracht U, eds. (2005) Food and human rights in development: legal and institutional dimensions and selected topics: volume 1. Antwerp: Intersentia
- Australian Bureau of Statistics (2015) Australian Aboriginal and Torres Strait Islander health survey: nutrition results – food and nutrients, 2012-13: Table 14.1 [data cube]. Retrieved 20 March 2015 from http://www.abs.gov.au/ausstats/subscriber.nsf/log?o penagent&4727055005_201213_14.xls&4727.0.55.005&Data%20 Cubes&2ABA2FFD38663577CA257E0D000ECF19&0&2012- 13&20.03.2015&Latest
- Dietitians Association of Australia (2016) Supporting document for the Joint Policy Statement on: Food Security for Aboriginal & Torres Strait Islander Peoples. Canberrra: Dietitians Association of Australia
- Australian Institute of Health and Welfare (2011) Aboriginal and Torres Strait Islander health performance framework 2010: detailed analyses. (AIHW Catalogue no IHW 53) Canberra: Australian Institute of Health and Welfare
- Brimblecombe J, van den Boogaard C, Wood B, Liberato SC, Brown J, Barnes A, Rogers A, Coveney J, Ritchie J, Bailie R (2015) Development of the good food planning tool: a food system approach to food security in Indigenous Australian remote communities. Health & Place;34:54-62
- Drewnowski A, Specter S (2004) Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition;79(1):6-16
- Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB (2007) Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. Journal of General Internal Medicine;22(7):1018-1023
- Palermo CE, Walker KZ, Hill P, Mcdonal J (2008) The cost of healthy food in rural Victoria. Rural and Remote Health 8.
- Nolan M, Rikard-Bell G, Mohsin M, Williams M (2006) Food insecurity in three socially disadvantaged localities in Sydney, Australia. Health Promotion Journal of Australia;17(3):247-253
- Crowley S, Antioch K, Carter R, Waters AM, Conway L, Mathers C (1992) The cost of diet-related disease in Australia: a discussion paper. Canberra: Australian Institute of Health and Welfare
- Access Economics (2008) The growing cost of obesity in 2008 : three years on. Canberra: Access Economics
- PricewaterhouseCoopers Australia (2015) Weighing the cost of obesity: a case for action. Sydney: PricewaterhouseCoopers Australia
- Gruen N, Lancy A (2011) The Herald/Age – Lateral Economics index of Australia’s wellbeing: final report. Melbourne: Lateral Economics
- Brown V, Moodie M, Baur L, Wen L, Hayes A (2017) The high cost of obesity in Australian pre-schoolers. Australian and New Zealand Journal of Public Health;41(3):323-324
- Australian Government Department of Health (2013) Nutrition: informing the development of Indigenous community agreements. Retrieved 12 August 2013 from http://www.health.gov.au/internet/ publications/publishing.nsf/Content/oatsih-evidence-socialhealthtoc~ nutrition
- URBIS (2010) Review of the National Aboriginal and Torres Strait Islander Nutrition Strategy and Action Plan 2000-2010: final report. Sydney: URBIS
- World Health Organization (2004) Global strategy on diet, physical activity and health. Geneva: World Health Organization
- Clifford A, Jackson Pulver L, Richmond R, Shakeshaft A, Ivers R (2009) Disseminating best-evidence health-care to Indigenous health-care settings and programs in Australia: identifying the gaps. Health Promotion International;24(4):404-415
- NSW Centre for Overweight and Obesity (2005) A literature review of the evidence for interventions to address overweight and obesity in adults and older Australians (with special reference to people living in rural and remote Australia and Aboriginal and Torres Strait Islanders). Sydney: Australian Department of Health and Ageing
- Johnston L, Doyle J, Morgan B, Atkinson-Briggs S, Firebrace B, Marika M, Reilly R, Cargo M, Riley T, Rowley K (2013) A review of programs that targeted environmental determinants of Aboriginal and Torres Strait Islander health. International Journal of Environmental Research and Public Health;10(8):3518-3542
- Herceg A (2005) Improving health in Aboriginal and Torres Strait Islander mothers, babies and young children: a literature review. Canberra: Department of Health and Ageing
- Jongen C, McCalman J, Bainbridge R, Tsey K (2014) Aboriginal and Torres Strait Islander maternal and child health and wellbeing: a systematic search of programs and services in Australian primary health care settings. BMC Pregnancy and Childbirth 14.
- Schembri L, Curran J, Collins L, Pelinovskaia M, Bell H, Richardson C, Palermo C (2016) The effect of nutrition education on nutritionrelated health outcomes of Aboriginal and Torres Strait Islander people: a systematic review. Australian and New Zealand Journal of Public Health;40(S1):S42–S47
- McDonald EL, Bailie RS, Rumbold AR, Morris PS, Paterson BA (2008) Preventing growth faltering among Australian Indigenous children: implications for policy and practice. Medical Journal of Australia;188(Supplement 8):S84-S86
- Butlin A, Cashel K, Lee A, Phyland P, Taylor V (1997) Food and nutrition programs for Aboriginal and Torres Strait Islander peoples. Canberra: Office for Aboriginal and Torres Strait Islander Health Services
- Rychetnik L, Webb K, Story L, Katz T (2003) Food security options paper: a planning framework and menu of options for policy and practice interventions. Sydney: NSW Centre for Public Health Nutrition
- Bywood PT, Raven M, Erny-Albrecht K (2015) Improving health in Aboriginal and Torres Strait Islander mothers, babies and young children: a literature review. Adelaide: Primary Health Care Research and Information Service
- Genat B, Browne J, Thorpe S, MacDonald C (2016) Sectoral system capacity development in health promotion: evaluation of an Aboriginal nutrition program. Health Promotion Journal of Australia;27(3):236-242
- Lee AJ, Leonard D, Moloney AA, Minniecon DL (2009) Improving Aboriginal and Torres Strait Islander nutrition and health: prevention and promotion – editorial. Medical Journal of Australia;190(10):547-548
- Morris NF, Stewart S, Riley MD, Maguire GP (2016) The Indigenous Australian Malnutrition Project: the burden and impact of malnutrition in Aboriginal Australian and Torres Strait Islander hospital inpatients, and validation of a malnutrition screening tool for use in hospitals – study rationale and protocol. SpringerPlus 5.
- Nguyen HD, Chitturi S, Maple-Brown LJ (2016) Management of diabetes in Indigenous communities: lessons from the Australian Aboriginal population. Internal Medicine Journal;46(11):1252-1259
- Foley W, Houston A (2014) Closing the gap by increasing access to clinical dietetic services for urban Aboriginal and Torres Strait Islander people. Nutrition & Dietetics;71(4):216-222
- Clifford A, Jackson Pulver L, Richmond R, Shakeshaft A, Ivers R (2011) Smoking, nutrition, alcohol and physical activity interventions targeting Indigenous Australians: rigorous evaluations and new directions needed. Australian and New Zealand Journal of Public Health;35(1):38–46
- Australian Better Health Initiative (2008) Tomorrow people. Australian Better Health Initiative
- Australian Institute of Health and Welfare (2016) Folic acid & iodine fortification. Retrieved 2016 from https://www.aihw.gov.au/reports/ food-nutrition/folic-acid-iodine-fortification/contents/summary
- Maxwell SJ, Brameld KJ, Bower C, D’Antoine H, Hickling S, Marley J, O’Leary P (2013) Baseline investigations of folate status in Aboriginal and non-Aboriginal West Australians prior to the introduction of mandatory fortification. Australian and New Zealand Journal of Obstetrics and Gynaecology;53(1):26–31
- Bower C, Maxwell S, Hickling S, D’Antoine H, O’Leary P (2016) Folate status in Aboriginal people before and after mandatory fortification of flour for bread-making in Australia. Australian and New Zealand Journal of Obstetrics and Gynaecology;56(3):233–237
- Mackerras DEM, Singh GR, Eastman CJ (2011) Iodine status of Aboriginal teenagers in the Darwin region before mandatory iodine fortification of bread. Medical Journal of Australia;194(3):126-130
- Rowley KG, Daniel M, Skinner K, Skinner M, White GA, O’Dea K (2000) Effectiveness of a community-directed ‘healthy lifestyle’ program in a remote Australian Aboriginal community. Australian and New Zealand Journal of Public Health;24(2):136-44
- Rowley KG (2001) Improvements in circulating cholesterol, antioxidants, and homocysteine after dietary intervention in an Australian Aboriginal community. American Journal of Clinical Nutrition;74(4):442-448
- Lee A, Bonson A, Yarmirr D, O’Dea K, Mathews J (1995) Sustainability of a successful health and nutrition program in a remote Aboriginal community. Medical Journal of Australia;162:632-635
- Lee AJ, Hobson V, Katarski L (1996) Review of the nutrition policy of the Arnhem Land Progress Association. Australian and New Zealand Journal of Public Health;20(5):538-544
- Gracey M, Bridge E, Martin D, Jones TW, Spargo RM, Shephard M, Davis EA (2006) An Aboriginal-driven program to prevent, control and manage nutrition-related “lifestyle” diseases including diabetes. Asia Pacific Journal of Clinical Nutrition;15(2):178-188
- Gwynn JD, Blunden SV, Turner N, Flood V, Attia J, Smith W, D’Este C, Wiggers J (2014) Many Rivers Diabetes Prevention Project 2007-2012: final report. Sydney: Ministry of Health
- Rodgers K, Willis D, Thomas R (1998) Environmental factors influencing Aboriginal nutrition in Western New South Wales. Health Promotion Journal of Australia;8(1):18-23
- Butler R, Tapsell L, Lyons-Wall P (2011) Trends in purchasing patterns of sugar-sweetened water-based beverages in a remote Aboriginal community store following the implementation of a communitydeveloped store nutrition policy. Nutrition & Dietetics;68(2):115-119
- Brimblecombe J, Ferguson M, Chatfield MD, Liberato SC, Gunther A, Ball K, Moodie M, Miles E, Magnus A, Mhurchu CN, Leach AJ, Bailie R (2017) Effect of a price discount and consumer education strategy on food and beverage purchases in remote Indigenous Australia: a stepped-wedge randomised controlled trial. The Lancet Public Health;2(2):e82-e95
- Brimblecombe J, Ferguson M, Liberato SC, Ball K, Moodie ML, Magnus A, Miles E, Leach AJ, Chatfield MD, Mhurchu CN, O’Dea K, Bailie RS (2013) Stores Healthy Options Project in Remote Indigenous Communities (SHOP@RIC): a protocol of a randomised trial promoting healthy food and beverage purchases through price discounts and in-store nutrition education. BMC Public Health 13.
- MacDonald C, Genat B, Thorpe S, Browne J (2015) Establishing healthpromoting workplaces in Aboriginal community organisations: healthy eating policies. Australian Journal of Primary Health;Online early(http://dx.doi.org/10.1071/PY14144)
- Reilly RE, Cincotta M, Doyle J, Firebrace BR, Cargo M, van den Tol G, Morgan-Bulled D, Rowley KG (2011) A pilot study of Aboriginal health promotion from an ecological perspective. BMC Public Health 11.
- Edwards C, Colbey A (2007) Yirrkala active cooking. Aboriginal and Islander Health Worker Journal;31(4):5-7
- Mills P, Pensio P, Sailor B (1997) The Garden Kai Kai Project. In: Council NHaMR, ed. Promoting the health of Aboriginal and Torres Strait Island Communities: case studies and principles of good practice. Canberra: National Health and Medical Research Council:3-8
- Remote Indigenous Gardens Network (2016) Remote Indigenous Gardens Network. Retrieved 2017 from http://www. remoteindigenousgardens.net/
- Viola A (2006) Evaluation of the Outreach School Garden Project: building the capacity of two Indigenous remote school communities to integrate nutrition into the core school curriculum. Health Promotion Journal of Australia;17(3):233-239
- Green R (2009) From little things, big things grow: investigating remote Aboriginal community gardens. University of Sydney, Sydney
- Gibbs L, Staiger PK, Townsend M, Macfarlane S, Gold L, Block K, Johnson B, Kulas J, Waters E (2013) Methodology for the evaluation of the Stephanie Alexander Kitchen Garden program. Health Promotion Journal of Australia;24(1):32-43
- Yeatman H, Quinsey K, Dawber J, Nielsen W, Condon-Paoloni D, Eckermann S, Morris D, Grootemaat P, Fildes D (2013) Stephanie Alexander kitchen garden national program evaluation: final report. Wollongong, NSW: Centre for Health Service Development, University of Wollongong
- Hume A, Wetten A, Feeney C, Taylor S, O’Dea K, Brimblecombe J (2014) Remote school gardens: exploring a cost-effective and novel way to engage Australian Indigenous students in nutrition and health. Australian and New Zealand Journal of Public Health;38(3):235-240
- Coyne T, Dowling M, Paoloni DC (1980) Evaluation of preschool meals programmes on the nutritional health of Aboriginal children. Medical Journal of Australia;2:369-375
- Black AP, Brimblecombe J, Eyles H, Morris P, Vally H, O′Dea K (2012) Food subsidy programs and the health and nutritional status of disadvantaged families in high income countries: a systematic review. BMC Public Health 12.
- Black AP, Vally H, Morris P, Daniel M, Esterman A, Karschimkus CS, O’Dea K (2013) Nutritional impacts of a fruit and vegetable subsidy programme for disadvantaged Australian Aboriginal children. British Journal of Nutrition;110(12):2309-2317
- Black AP, Vally H, Morris PS, Daniel M, Esterman AJ, Smith FE, O’Dea K (2013) Health outcomes of a subsidised fruit and vegetable program for Aboriginal children in northern New South Wales. Medical Journal of Australia;199(1):46-50
- Kristjansson E, Francis DK, Liberato S, Benkhalti Jandu M, Welch V, Batal M, Greenhalgh T, Rader T, Noonan E, Shea B, Janzen L, Wells GA, Petticrew M (2015) Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years. Queensland: Cochrane Database of Systematic Reviews
- Crawford B, Yamazaki R, Franke E, Amanatidis S, Ravulo J, Steinbeck K, Ritchie J, Torvaldsen S (2014) Sustaining dignity? Food insecurity in homeless young people in urban Australia. Health Promotion Journal of Australia;25(2):71-78
- Mullum Mullum Indigenous Gathering Place (2016) Mullum Mullum Indigenous Gathering Place: foodbank. Retrieved 2017 from http:// www.mmigp.org.au/foodbank
- Warchivker I (2003) An analysis of a community response to child nutrition problems at Kintore (Walungurru) 1998-2001. Alice Springs: Centre for Remote Health
- Miller M, Coffin J, Shaw P, D’Antoine H, Larson A, James R (2004) Evaluation of Indigenous nutrition projects funded by the National Childhood Nutrition Program in Western Australia: final report. Perth: Telethon Institute for Child Health Research, Combined Universities Centre for Rural Health
- Indigenous Health Service (2005) Good food great kids: an Indigenous community nutrition project 2002-2004. Healesville, VIC: Indigenous Health Service, Yarra Valley Community Health Service, Eastern Health
- Roberts D, Simmond T (2007) Grace Close Nutrition and Wellbeing Programme. Sydney: Collaborative Centre for Aboriginal Health Promotion
- Curtis S, Pegg D, Curtis O (2004) Aunty Jean’s Good Health Team: listening to the voices of the Elders to create an Aboriginal chronic and complex care program. Unanderra, NSW: Illawarra Health
- Briggs J (2001) Impact of an integrated approach to diabetes care at Rumbalara Aboriginal Health Service. Melbourne: Department of Rural Health, University of Melbourne
- Browne J, Thorpe S, MacDonald C, Atkinson P, Bonnell E, Murray M, Barbour L, Yam C (2014) Aboriginal community food program success stories: sharing the tracks to good tucker. Melbourne: Victorian Aboriginal Community Controlled Health Organisation
- Aquino D, Marley JV, Senior K, Leonard D, Helmer J, Joshua A, Huddleston A, Ferguson H, Hobson V, Hadgraft N (2013) Early Childhood Nutrition and Anaemia Prevention Project : summary report. Darwin: The Fred Hollows Foundation, Indigenous Australia Program
- Queensland Health (2005) 2005 Evaluation of the Healthy Weight Program: summary report. Brisbane: Queensland Health
- Foley RM, Pollard CM (1998) Food Cent$ – implementing and evaluating a nutrition education project focusing on value for money. Australian and New Zealand Journal of Public Health;22(4):494-501
- Chan LCK (2007) Short term efficacy of a lifestyle intervention programme on cardiovascular health outcome in overweight Indigenous Australians with and without type 2 diabetes mellitus: the healthy lifestyle programme (HELP). Diabetes Research and Clinical Practice;75(1):65-71
- Tyrrell M, Grundy J, Lynch P, Wakerman J (2003) Laramba Diabetes Project: an evaluation of a participatory project in a remote Northern Territory community. Health Promotion Journal of Australia;14(1):48-53
- Reilly R, Doyle J, Rowley K (2007) Koori community-directed health promotion in the Goulburn Valley. Australian Community Psychologist;19(1):39-46
- Community Matters Consultancy (2007) Community Foodies Program 2006-07: a realist evaluation. Noarlunga, SA: Southern Adelaide Health Service
- Nilson C, Kearing-Salmon KA, Morrison P, Fetherston C (2015) An ethnographic action research study to investigate the experiences of Bindjareb women participating in the cooking and nutrition component of an Aboriginal health promotion programme in regional Western Australia. Public Health Nutrition;FirstView(http:// journals.cambridge.org/action/displayAbstract?fromPage=online& aid=9669086&fulltextType=RA&fileId=S1368980015000816)
- Smith J (2002) Wadja Warriors football team’s healthy weight program. Aboriginal and Islander Health Worker Journal;26(4):13-15
- Gui G, Lau Q (2007) ‘Quick meals for Kooris’: an evaluation. Aboriginal and Islander Health Worker Journal;31(4):20-21
- Dunn S, Dewis E (2001) Healthy weight program evaluation, Queensland 1996-1999. Aboriginal and Islander Health Worker Journal;25(4):26-28
- Howie RJ (2004) Formative evaluation of the Kuwinyuwardu Aboriginal Resource Unit Gascoyne Healthy Lifestyle Program. Subiaco, Western Australia: School of Population Health, University of Western Australia
- Amy S (2008) Food For All program progress report. Swan Hill, Vic: Swan Hill Rural City Council
- Moore L, Webb R, Abbott P, Zonka B (2006) Cooking classes for diabetes: a partnership between Daruk Aboriginal Medical Service and the Western Sydney Institute of TAFE. Aboriginal and Islander Health Worker Journal;30(6):11-13
- Active Healthy Communities (2014) Fitness and Sports Training (FAST) and Deadly Tucker programs. Sunshine Coast, Qld: Active Healthy Communities
- Gunnion T (2008) Frankston Community Kitchens pilot project report. Frankston, Vic: Frankston Community Health Service
- Diabetes Queensland (2015) Need For Feed. Retrieved 2015 from http://www.needforfeed.org.au/
- The Good Foundation (2017) Jamie’s Ministry of Food. Retrieved 2017 from https://www.thegoodfoundation.com.au/program/jamiesministry- of-food
- Vidgen HA, Adam M, Gallegos D (2017) Who does nutrition prevention work in Queensland? An investigation of structural and political workforce reforms. Nutrition & Dietetics;74(1):88-94
- Crawford SM, Kallina L (1997) Building food security through health promotion: community kitchens. Journal of the Canadian Dietetic Association;58(4):197-201
- Fredericks B, Anderson M (2013) Aboriginal and Torres Strait Islander cookbooks : promoting Indigenous foodways or reinforcing Western traditions? Presented Brisbane
- FOODcents (2017) FOODcents. Retrieved 2017 from http://www. foodcentsprogram.com.au/
- Pettigrew S, Jongenelis MI, Moore S, Pratt IS (2015) A comparison of the effectiveness of an adult nutrition education program for Aboriginal and non-Aboriginal Australians. Social Science & Medicine;In press(http://dx.doi.org/10.1016/j.socscimed.2015.09.025)
- Life! (2015) About the Life! program. Retrieved 2015 from http://www. lifeprogram.org.au/about-the-life-program/about-the-program
- Diabetes Australia (2013) Aboriginal and Torres Strait Islanders and diabetes action plan. Canberra: Diabetes Australia
- McDermott RA, Schmidt B, Preece C, Owens V, Taylor S, Li M, Esterman A (2015) Community health workers improve diabetes care in remote Australian Indigenous communities: results of a pragmatic cluster randomized controlled trial. BMC Health Services Research 15.
- Browne J, D’Amico E, Thorpe S, Mitchell C (2014) Feltman: evaluating the acceptability of a diabetes education tool for Aboriginal health workers. Australian Journal of Primary Health;20(4):319-322
- Stoneman A, Atkinson D, Davey M, Marley JV (2014) Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal Community Controlled Health Services. BMC Health Services Research 14.
- Bailie R, Si D, Dowden M, O’Donoghue L, Connors C, Robinson G, Cunningham J, Weeramanthri T (2007) Improving organisational systems for diabetes care in Australian Indigenous communities. BMC Health Services Research 7.
- Browne J, Hayes R, Gleeson D (2014) Aboriginal health policy: is nutrition the ‘gap’ in ‘Closing the Gap’? Australian and New Zealand Journal of Public Health;38(4):362-369
- Lee AJ, Baker P, Stanton R, Friel S, Weightman A (2013) Scoping study to inform the development of the new national nutrition policy for Australia. Canberra: Australian Department of Health and Ageing
- Australian Institute of Health and Welfare (2013) Healthy for Life: Aboriginal Community Controlled Health Services: report card. (AIHW Catalogue no IHW 97) Canberra: Australian Institute of Health and Welfare
- Steering Committee for the Review of Government Service Provision (2014) Report on government services 2014: Indigenous compendium. Canberra: Productivity Commission
- Graham S, McCall E, Morris L (2015) Breastfeeding education within an aboriginal community using community development principles through Australian breastfeeding association community mentoring workshops. HNE Handover: For Nurses and Midwives;8(2 (Special Issue)):217
- Egger G, Fisher G, Piers S, Bedford K, Morseau G, Sabasio S, Taipim B, Bani G, Assan M, Mills P (1999) Abdominal obesity reduction in Indigenous men. International Journal of Obesity and Related Metabolic Disorders;23(6):564-569
- Mackerras D (2001) Birthweight changes in the pilot phase of the Strong Women Strong Babies Strong Culture Program in the Northern Territory. Australian and New Zealand Journal of Public Health;25(1):34-40
- Woods B, Campbell C, Miller M, Thompson C (1998) ‘Eat healthy tucker’ Aboriginal nutrition training workshops. Health Promotion Journal of Australia;8(1):62-63
- Warburton J, Chambers B (2007) Older Indigenous Australians: their integral role in culture and community. Australasian Journal on Ageing;26(1):3-7
- Adams K, Browne J, Palermo C, Radford G (2016) Experiences of urban Australian Indigenous peer mentors in a non-communicable disease prevention program. AlterNative;12(4):425-436
- Browne J, Thorpe S, Tunny N, Adams K, Palermo C (2013) A qualitative evaluation of a mentoring program for Aboriginal health workers and allied health professionals. Australian and New Zealand Journal of Public Health;37(5):457-462
- Malseed C, Nelson A, Ware R (2014) Evaluation of a school-based health education program for urban Indigenous young people in Australia. Scientific Research;6(7):587 – 597
- Wilson A, Delbridge R, Palermo C (2016) Why we need a community of practice for dietitians working in Indigenous health [letter]. Nutrition & Dietetics;73(1):114
- Colles SL, Belton S, Brimblecombe J (2016) Insights into nutritionists’ practices and experiences in remote Australian Aboriginal communities. Australian and New Zealand Journal of Public Health;40(S1):S7–S13
- National Nutrition Networks Conference (2008) National nutrition networks conference: priority recommendations – March 2008. Alice Springs: National Rural Health Alliance
- Indigenous Allied Health Australia (2017) Personal communication. Indigenous Allied Health Australia
- Dietitians Association Australia (2017) Personal communication. Dietitians Association Australia
- Laurence S (2009) Development of an Australian Aboriginal and Torres Strait Islander nutrition workforce: information paper. Canberra: NATSINSAP
- Hudson S (2017) Evaluating Indigenous programs: a toolkit for change. Sydney: Centre for Independent Studies
- Council of Australian Governments (2007) Council of Australian Governments’ meeting [1] 13 April 2007: COAG communiqué. Canberra: Council of Australian Governments
- Dick D, Holland C, Harrison B (2008) Closing the gap: national Indigenous health equality targets: outcomes from the National Indigenous Health Equality Summit. Canberra: Human Rights and Equal Opportunity Commission
- Wright P, Lewis P (2017) Close the Gap: progress and priorities report 2017. Canberra: Close the Gap Campaign Steering Committee
- Council of Australian Governments (2008) Council of Australian Governments’ meeting, 26 March 2008: Indigenous reform. Canberra:
- Council of Australian Governments (2011) National health reform agreement. Canberra: Council of Australian Governments
- Council of Australian Governments (2009) National strategy for food security in remote Indigenous communities. Canberra: Council of Australian Governments
- Department of the Prime Minister and Cabinet (2016) Closing the Gap Prime Minister’s report 2016. Canberra: Department of the Prime Minister and Cabinet
- Gracey M (2014) Why closing the Aboriginal health gap is so elusive. Internal Medicine Journal;44(11):1141-1143
- Pratt S, DeMamiel M, Reye K, Huey A, Pope A (2014) Food security in remote Indigenous communities. (ANAO report no2 2014-15) Canberra: Australian National Audit Office
- South Australian Department of the Premier and Cabinet (2013) Anangu Pitjantjatjara Yankunytjatjara (APY) Lands: Food Security Strategic Plan 2011-2016 Year 2 Evaluation. Adelaide: South Australian Department of the Premier and Cabinet
- Department of Human Services (2013) Income management. Retrieved 2017 from https://www.humanservices.gov.au/ individuals/services/centrelink/income-management
- Department of Health and Ageing (2013) Remote Indigenous Stores and Takeaways (RIST) Project. Retrieved 2013 from http://www. health.gov.au/internet/main/publishing.nsf/Content/phd-nutritionrist
- Australian Government Department of Health (2015) Implementation plan for the National Aboriginal and Torres Strait Islander Health Plan 2013–2023. Canberra: Australian Government Department of Health
- Commonwealth of Australia (2008) Northern Territory National Emergency Response Act 2007. Canberra: Commonwealth of Australia
- Department of Families Housing Community Services and Indigenous Affairs (2012) Stronger Futures in the Northern Territory: a ten year commitment to Aboriginal people in the Northern Territory. Canberra: Department of Families, Housing, Community Services and Indigenous Affairs
- Brimblecombe J, McDonnell J, Dhurrkay JG, Thomas DP, Bailie RS (2010) Impact of income management on store sales in the Northern Territory: after the intervention — research. Medical Journal of Australia;192(10):549-554
- Outback Stores (2016) Outback Stores: working with communities: annual report 2015-2016. Darwin: Outback Stores
- Australian Parliament Hansard (2016) Finance and Public Administration Legislation Committee 21/10/2016 Estimates: Cross- Portfolio Indigenous Matters: Outback Stores Pty Ltd. Canberra: Australian Parliament Hansard
- Australian Health Ministers’ Advisory Council (2017) National Strategic Framework for Chronic Conditions. Canberra: Australian Government
- National Health Priority Action Council (2006) National chronic disease strategy. Canberra: Australian Government Department of Health and Ageing
- Osborne K, Baum F, Brown L (2013) What works? A review of actions addressing the social and economic determinants of Indigenous health. (Issues paper no 7) Canberra: Closing the Gap Clearinghouse
- Lee A, Turner N (2016) We can close the Indigenous nutrition gap – here’s how. Retrieved 16 February 2016 from https://theconversation.com/ we-can-close-the-indigenous-nutrition-gap-heres-how-54529
- Brimblecombe J, Maypilama E, Colles S, Scarlett M, Dhurrkay JG, Ritchie J, O’Dea K (2014) Factors influencing food choice in an Australian Aboriginal community. Qualitative Health Research;24(3):387-400
- Foley W, Schubert L (2013) Applying strengths-based approaches to nutrition research and interventions in Australian Indigenous communities. Journal of Critical Dietetics;1(3):15-25
- National Congress of Australia’s First Peoples (2012) What does success look like? Measuring the success of the National Aboriginal and Torres Strait Islander health plan. Sydney: National Congress of Australia’s First Peoples
- Australian Department of Health (2015) National Aboriginal and Torres Strait Islander Health Plan 2013-2023 [webpage]. Retrieved 2015 from http://www.health.gov.au/natsihp
- Heckman JJ, Mosso S (2014) The economics of human development and social mobility. Annual Review of Economics;6(1):689-733
- O’Dea K, Rowley KG, Brown A (2007) Diabetes in Indigenous Australians: possible ways forward. Medical Journal of Australia;186(10):494-495
- National Health and Medical Research Council (2012) Infant feeding guidelines for health workers. Canberra: National Health and Medical Research Council
- Rogers A, Ferguson M, Ritchie J, Van Den Boogaard C, Brimblecombe J (2016) Strengthening food systems with remote Indigenous Australians: stakeholders’ perspectives. Health Promotion International;Advance access(http://dx.doi.org/10.1093/heapro/ daw047)
- National Nutrition Networks Conference (2000) Recommendations. Retrieved 2000 from http://www.healthinfonet.ecu.edu.au/uploads/ conferences/81_nnncrecommendations.pdf
- National Public Health Partnership (2001) Eat well Australia: an agenda for action in public health nutrition, 2000-2010. Canberra: National Public Health Partnership
- Cargo M, Marks E, Brimblecombe J, Scarlett M, Maypilama E, Dhurrkay JG, Daniel M (2011) Integrating an ecological approach into an Aboriginal community-based chronic disease prevention program: a longitudinal process evaluation. BMC Public Health 11.
- Queensland Health (2006) Urban Indigenous nutrition issues in the Greater Brisbane Area. Brisbane: Queensland Health
- Masters G, Coles-Rutishauser I, Webb K, Marks G, Pearse J (2006) National food and nutrition monitoring and surveillance system: a framework and a business case: final report. Melbourne: Nexus Management Consulting
- Australian Bureau of Statistics (2017) Information paper: Australian Health Survey – evaluation, July 2017. (ABS Cat no. 4364.0.55.013) Canberra: Australian Bureau of Statistics
- Eades SJ, Stanley FJ (2013) Improving the health of First Nations children in Australia. Medical Journal of Australia;199(1):12-13
- Sanson-Fisher RW, Campbell EM, Perkins JJ, Blunden SV, Davis BB (2006) Indigenous health research: a critical review of outputs over time. Medical Journal of Australia;184(10):502-505
- Longstreet D, Health D, Savage I, Vink R, Panaretto KS (2008) Estimated nutrient intake of urban Indigenous participants enrolled in a lifestyle intervention program. Nutrition & Dietetics;65(2):128-133
- Fredericks B (2013) Commentary on nutrition and older Indigenous Australians: service delivery implications in remote communities. A narrative review. Australasian Journal on Ageing;32(4):198-199
- Schouten K, Lindeman MA, Reid JB (2013) Nutrition and older Indigenous Australians: service delivery implications in remote communities. A narrative review. Australasian Journal on Ageing;32(4):204-210
- Browne J, Laurence S, Thorpe S (2009) Acting on food insecurity in urban Aboriginal and Torres Strait Islander communities. Melbourne: Heart Foundation
- National Health and Medical Research Council (2015) Aboriginal and Torres Strait Islander guide to healthy eating. Canberra: National Health and Medical Research Council
- Australian Bureau of Statistics (2013) Australian Aboriginal and Torres Strait Islander health survey: user’s guide, 2012-13: under-reporting in the national Aboriginal and Torres Strait Islander nutrition survey. Retrieved 27 November 2013 from http://www.abs.gov.au/ausstats/ abs@.nsf/Lookup/D9B74ECEA9D88C66CA257E0D000EDA59
- McMahon E, Wycherley T, O’Dea K, Brimblecombe J (2017) A comparison of dietary estimates from the National Aboriginal and Torres Strait Islander Health Survey to food and beverage purchase data. Australian and New Zealand Journal of Public Health;Early view(https://doi.org/10.1111/1753-6405.12718)
- Australian Bureau of Statistics (1998) National Nutrition Survey. Retrieved 2004 from http://www.abs.gov.au/AUSSTATS/abs@.nsf/0/ 01F2086AD5CDBF65CA256BD000272375?OpenDocument
- Australian Health Ministers’ Advisory Council (2008) Aboriginal and Torres Strait Islander health performance framework report 2008. Canberra: Department of Health and Ageing
- Adamson P (2010) The children left behind: a league table of inequality in child well-being in the world’s rich countries. (Innocenti Report Card no. 9) Florence, Italy: UNICEF
Footnotes
- The crystallized honey produced by larvae of psyllid bugs
- Information on BMI and measuring weight and chronic disease risk is included in Box 3.
- Information on BMI and measuring weight and chronic disease risk is included in Box 3.
- Limitations associated with the NATSINPAS data collection methodology are outlined in Appendix 3
- Discretionary foods and drinks are those not necessary for health, but high in saturated fat, added sugar, salt and/or alcohol; commonly called ‘junk’ foods and drinks
- Free sugars include sugars added to food and drinks together with honey and fruit juice
- When an electrical current is passed through the body, fatty tissue offers more resistance than lean tissue. The resistance to the flow of electricity is used to calculate the proportion of body fat in the individual.