Selection of appropriate spirometry reference values in Aboriginal Australians
Brief reportWhite E1,2, James A3,4, de Klerk N1,2,5, Musk A W5,6, Hall G L.1,2,7 (2019)
- Telethon Kids Institute, Perth, Australia
- Centre for Child Health Research, University of Western Australia, Perth.
- Department of Pulmonary Physiology/West Australian Sleep Disorders Research Institute, Sir Charles Gardiner Hospital, Perth, Western Australia.
- School of Medicine and Pharmacology, University of Western Australia, Perth.
- School of Population and Global Health, University of Western Australia, Perth
- Department of Respiratory Medicine, Sir Charles Gairdner Hospital
- School of Physiotherapy and Exercise Science, Faculty of Health Sciences, Curtin University, Perth, Australia
Suggested citation: White E, James A, de Klerk N, Musk A W, Hall G L. (2019). Selection of appropriate spirometry reference values in Aboriginal Australians. Australian Indigenous HealthBulletin 19(3). Retrieved from: https://healthbulletin.org.au/articles/selection-of-appropriate-spirometry-reference-values-in-aboriginal-australians/
Corresponding author: Prof Graham Hall, Children’s Lung health, Telethon Kids Institute, PO Box 855, West Perth, WA 6872, email: Graham.hall@telethonkids.org.au
Download PDF (382KB)
Abstract
Objective: The Global Lung Function Initiative (GLI) spirometry equations for “Other” ethnic groups have been recommend for use in Aboriginal Australians until appropriate spirometry equations can be developed. We sought to validate the GLI ‘Other’ equations in healthy Aboriginal Australians.
Methods: Spirometry in Aboriginal Australians with no history of lung disease or tobacco smoking were obtained. Predicted spirometry (forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC) and FEV1/FVC were calculated from the GLI ‘Caucasian’ and ‘Other’ equations. An a priori agreement was set at a mean Z score <0.5.
Results: Spirometry was available in 87 healthy Aboriginal children and adults (aged 5 to 76 years (48% male)). Mean (SD) predicted FEV1 and FVC derived from the GLI ‘Caucasian’ equations (-1.95 (1.07) and -2.08 (1.06), respectively) were significantly lower than predicted. Similarly, the GLI ‘Other’ equation was a poor predictor of lung function in healthy Aboriginal Australians (FEV1: -1.49 (1.14), FVC: -1.62(1.19)). In contrast, FEV1/FVC Z-scores were not significantly different from zero whether compared with predicted ‘Caucasian’ (0.15 (0.82)) or ‘Other’ (-0.01(0.87)).
Conclusions: The Global Lung Function ‘Caucasian’ and ‘Other’ spirometry equations do not match healthy Aboriginal FEV1 and FVC data. Our data supports the use of GLI ‘Other’ FEV1/FVC to detect obstructive lung disease in Aboriginal Australians
Implications: The use of inappropriate spirometry reference equations can have clinical consequences. Appropriate lung function reference equations for Aboriginal and Torres Strait Islanders are urgently needed.
Introduction
The prevalence of lung disease and the associated mortality and morbidity are significantly increased in Aboriginal and Torres Strait Islander peoples when compared with non-Aboriginal Australians [1-4]. Given the significantly increased burden associated with lung disease in Aboriginal and Torres Strait Islander peoples, it is vital that healthcare services are able to provide accurate tools for the diagnosis and management of patients with breathing difficulties.
The early diagnosis and management of lung disease can reduce disease burden, improve quality of life, reduce mortality, and lower healthcare costs [5]. Spirometry, the most commonly used lung function test, plays an important role in the the diagnosis and management of asthma and other lung diseases [6]. An individual’s lung function results can be characterised as normal or abnormal and as being responsive to medications, such as bronchodilators. However, the ability to define a lung function result as ‘normal’ or ‘abnormal’ hinges on the comparison of an individual’s results to those expected from a healthy reference population of the same ethnic background.
The 2012 Global Lung Function Initiative (GLI) collated spirometry from ~70,000 individuals aged 3 to 95 years to create the first multi-ethnic all ages spirometry reference equations [7]. In addition to deriving reference ranges for Caucasian, African American and North- and South-East Asians an additional reference equation was created using the entire non-Caucasian data-set (labelled “Other”) as an interim measure for those ethnicities where specific reference equations were yet to be created. Current recommendations from the Australian and New Zealand Society of Respiratory Science advise adoption of GLI spirometry reference equations in Australia, and the use of the GLI ‘Other’ equations in Australian Aboriginal and Torres Strait Islander populations, for whom there are no current GLI ethnic-specific equations [8].
The limited spirometry data available in Aboriginal and Torres Strait Islander peoples without a history of lung disease suggests that spirometry (e.g. forced expiratory volume in 1 seconds (FEV1)) is 20% to 30% lower than in the non-Aboriginal population [9-11], indicating that the use of lung function reference equations derived from non-Aboriginal groups may be inappropriate in the Aborignal and Torres Strait Islander population. These results reinforce the recommendations of the Australian and New Zealand Society of Respiratory Science against using Caucasian reference equations in Aboriginal populations [8].
An important finding of the GLI was that, after accounting for height and gender, ethnic differences are stable across all ages. For example, at the population level, FEV1 in African-Americans is ~15% lower than Caucasians, after accounting for height and gender, and this difference is consistent across the full age range represented by the GLI equations (3 to 95 years). This greatly facilitates the development of reference ranges in ethnic populations currently not included in the GLI spirometry equations and the implementation of these new equations into clinical practice.
In this study, we aimed to assess the appropriateness of the Global Lung Function Initiative ‘Other’ reference equations for spirometry in healthy Aboriginal Australians.
Methods
We performed an assessment of differences between spirometry outcomes in healthy, non-smoking Aboriginal children and adults, and predicted values derived from GLI Caucasian and Other reference equations, by reanalysing the spirometry and respiratory health data of 437 individuals from two remote Aboriginal communities [9, 12]. To ensure only data from healthy, non-smoking individuals were included, we excluded those with any of the following: a questionnaire-history of smoking ever, a doctor diagnosis of any lung disease and self-reported recurrent respiratory symptoms in the past year.
Following these exclusions, data were available for 87 healthy Aboriginal Australians aged 5 to 76 years (48% male). Predicted lung function, in the form of Z scores, for FEV1, FVC and FEV1/FVC, were derived for the GLI ‘Caucasian’ and ‘Other’ equations. A perfect match of a healthy population to the reference group would give a mean Z score of 0 with a standard deviation of 1 and with no relationship between derived Z scores and age, height and gender. The appropriateness of the GLI equations for Aboriginal Australians was assessed using a one-sided t-test compared to zero. The GLI group considers a mean Z-score difference between populations of >0.5 Z-score as being physiologically relevant [13].
Results
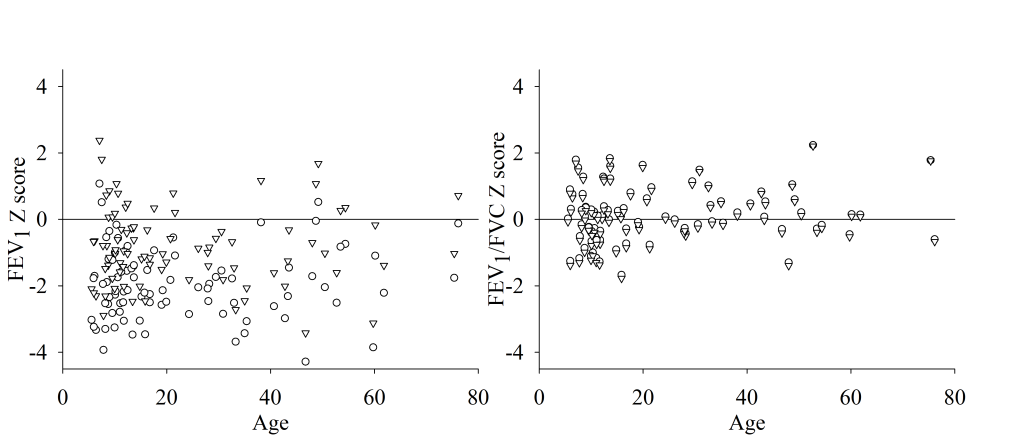
The mean (SD) FEV1 Z-score was significantly lower than that predicted from GLI Caucasian reference data (-1.95 (1.07)) equating to 76 (13.7) % predicted (figure 1, left panel). Predicted FEV1 derived from the GLI ‘Other’ equations was also significantly lower than zero with a mean (SD) Z-score of -1.49 (1.14) and % predicted of 81.3(14.7) %). Mean FVC was also significantly lower than predicted from GLI Caucasian reference data (-2.08 (1.06)) equating to 74.8 (13.1) % predicted, with predicted FVC derived from the GLI ‘Other’ equations also significantly lower than normal (-1.62(1.19) FVC Z score and 81.2(14.3) % predicted). In contrast, FEV1/FVC Z-scores were not significantly different from zero whether compared with predicted Caucasian (0.15 (0.82)) or ‘Other’ (-0.01(0.87)) GLI FEV1/FVC reference data (figure 1, right panel). There were no significant associations between FEV1, FVC and FEV1/FVC Z scores and participants age or height for either GLI prediction equation (p>0.05; data not shown).
The choice of reference equation significantly affected the proportion of participants with abnormal lung function (defined as below the lower limit of normal and equating to < -1.64 Z-scores). In these data, 66.7% (n=58) and 40.6% (n=44) of individuals had abnormally low FEV1, and 72.4% (n=63) and 52.9% (n=46) had abnormally low FVC, when compared with Caucasian and Other predicted equations respectively. In contrast, only 1 participant had abnormally low FEV1/FVC and was < -1.64 Z-score for both the GLI Caucasian and Other predicted equations.
Figure 1: FEV1 (left) and FEV1/FVC (right) Z-scores in healthy Aboriginal Australians calculated for each individual using Caucasian (circles) or Other (triangles) GLI predicted equations.
Discussion
In this study, we assess the appropriateness of the use of the Global Lung Function Initiative spirometry prediction equations for Aboriginal Australians. We report that there is a real ethnic population difference between healthy Aboriginal and Caucasian FEV1 and FVC and the use of GLI ‘Other’ predicted equations may still lead to overestimation of abnormal FEV1 and FVC in healthy Aboriginal Australians. In contrast, the predicted FEV1/FVC from healthy Aboriginal children and adults was a good match to both the Caucasian or Other GLI FEV1/FVC prediction equations.
Our finding that FEV1/FVC may be reasonably predicted in Aboriginal Australians by GLI Caucasian and Other FEV1/FVC reference equations agrees with the findings of the GLI group that, after accounting for age, height and gender, predicted FEV1/FVC is generally independent of ethnicity [7]. The Global Lung Function Initiative group found that ethnic differences in FEV1/FVC ranged between ~1% in African Americans and up to ~3% in South-east Asians compared to Caucasian data [7]. This finding reinforces the value of using the GLI approach to derive new ethnic correction factors for lung function outcomes in Aboriginal Australians and affirms the Australian and New Zealand Society of Respiratory Science recommendations that the GLI ‘Other’ FEV1/FVC is the most appropriate reference value option to diagnose obstructive lung disease in ethnic groups lacking GLI ethnicity-specific reference equations [8].
Previous studies exploring normal lung function in Aboriginal Australians have common limitations such as small samples of rural communities and include smokers and those with respiratory disease [9-12, 14]. This analysis was from a limited sample size of 87 participants, and therefore its findings need to be considered with some caution. The participants were all from rural communities, whereas the majority of Aboriginal Australians live in urban and regional centres, so our results may not be applicable to the wider Aboriginal Australian population. However, despite these limitations, our analysis does suggest that there is likely to be a real population difference between healthy Aboriginal and Caucasian spirometry.
The results of this study highlight the problems with using ethnically inappropriate prediction equations. Considering the heavy burden of respiratory disease within the Aboriginal Australian population, there is an urgent need to produce high quality ethnic-specific spirometry reference data for this group [14]. This may be effectively completed by collecting spirometry data in healthy Aboriginal Australians, that meets the necessary exclusion criteria and includes adequate participant numbers and modelling an ethnic correction factor using GLI modelling techniques. In the interim, our analysis lends support to the current recommendation of the Australian and New Zealand Society of Respiratory Science to use FEV1/FVC in clinical practice to diagnose obstructive lung disease in Aboriginal Australians [8].
References
- Australian Institute of Health and Welfare 2010. Asthma, chronic obstructive pulmonary disease and other respiratory diseases in Australia. Canberra: AIHW; 2010.
- Australian Institute of Health and Welfare 2011. The health and welfare of Australia’s Aboriginal and Torres Strait Islander people, an overview. Canberra2011.
- O’Grady KF, Hall KK, Bell A, Chang AB, Potter C. Review of respiratory diseases among Aboriginal and Torres Strait Islander children. Australian Indigenous HealthBulletin. 2018;18(2).
- Poulos AM, Cooper SJ, Ampon R, Reddel HK, Marks GB. Australian Institute of Health and Welfare. Mortality from asthma and COPD in Australia. Canberra: AIHW; 2014.
- Abramson MJ, Crockett AJ, Frith PA, McDonald CF. COPDX: an update of guidelines for the management of chronic obstructive pulmonary disease with a review of recent evidence. Med J Aust. 2006;184(7):342-5.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-68.
- Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324-43.
- Brazzale D, Hall G, Swanney MP. Reference values for spirometry and their use in test interpretation: A Position Statement from the Australian and New Zealand Society of Respiratory Science. Respirology. 2016;21(7):1201-9.
- Bremner PR, de Klerk NH, Ryan GF, James AL, Musk M, Murray C, et al. Respiratory symptoms and lung function in aborigines from tropical Western Australia. Am J Respir Crit Care Med. 1998;158(6):1724-9.
- Thompson JE, Sleigh AC, Passey ME, Barnes A, Streatfield RW. Ventilatory standards for clinically well aboriginal adults. Med J Aust. 1992;156(8):566-9.
- Veale AJ, Peat JK, Salome CM, Woolcock AJ, Thompson JE. ‘Normal’ lung function in rural Australian aborigines. Aust N Z J Med. 1997;27(5):543-9.
- Musk AW, James AL, Palmer LJ, Ryan GF, Lake F, Golledge CL, et al. Respiratory infections and lung function in an Australian Aboriginal community. Respirology. 2008;13(2):257-62.
- Quanjer PH, Stocks J, Cole TJ, Hall GL, Stanojevic S, Global Lungs I. Influence of secular trends and sample size on reference equations for lung function tests. Eur Respir J. 2011;37(3):658-64.
- Blake TL, Chang AB, Petsky HL, Rodwell LT, Brown MG, Hill DC, et al. Spirometry reference values in Indigenous Australians: a systematic review. Med J Aust. 2016;205(1):35-40.