A community-based lifestyle intervention targeting Type II Diabetes risk factors in an Australian Aboriginal population: a feasibility study
Original article (peer reviewed)Rankin P, Morton D, Kent L, Mitchell B (2016) A community-based lifestyle intervention targeting Type II Diabetes risk factors in an Australian Aboriginal population: a feasibility study. Australian Indigenous HealthBulletin 16(3). Retrieved [access date] from http://healthbulletin.org.au/articles/a-community-based-lifestyle-intervention-targeting-type-ii-diabetes-risk-factors-in-an-australian-aboriginal-population-a-feasibility-study
Lifestyle Research Centre at Avondale College of Higher Education
Abstract
Objectives: To examine the responsiveness of an Aboriginal cohort to a community-based lifestyle intervention targeting risk factors for type II diabetes.
Methods: A Pre-test/post-test cohort study conducted in two rural Australian locations: Port Augusta, South Australia and Drouin, Victoria. The cohort consisted of 25 individuals of Aboriginal descent (mean age = 44.4 ± 12.3 yrs, age range = 25-70 yrs, 7 males/18 females). The intervention used was the Complete Health Improvement Program, involving 11 group sessions conducted over a one-month period, which promoted a low-fat plant-based diet and physical activity. The main outcomes measured were changes in body weight, fasting plasma glucose (FPG), lipid profile and blood pressure (BP).
Results: Over the 4 week intervention mean body weight decreased by 3.1 kg (95% CI 2.26 to 4.06), a 3.5% reduction from baseline (p<0.001). FPG decreased on average by 16.1% (6.15 mmol/L to 5.16 mmol/L, p=0.001). There was no change in BP or lipid profile. Analyses of the 11 participants who had FPG levels > 5.5 mmol/L at baseline showed a 23.6% reduction in mean FPG (7.82 mmol/L to 5.97 mmol/L, p=0.005) and a 4.12% reduction in body weight (98.85 kg to 94.78 kg, p<0.001).
Conclusion: This feasibility study showed that a lifestyle intervention promoting a low-fat eating pattern combined with physical activity reduced risk factors associated with type II diabetes in a rural Aboriginal cohort when conducted in their usual living environment.
Implications: There is potential for committee-based lifestyle interventions to improve the health risk profile of Aboriginal participants.
View PDF version (PDF – 482KB)
Introduction
In developed countries, first nation or aboriginal people have significantly worse health indicators than non-indigenous populations [1]. In 2003, the life expectancy gap between Aboriginal and non-Indigenous Australians was estimated to be 19-21 years, exceeding that observed in New Zealand (8 years), Canada (5-7 years) and the United States (4 to 5 years) [2]. While the life expectancy gap in Australia has narrowed over the past decade, Aboriginal Australians still live on average 10 to 11 years less than non-Indigenous individuals and death rates are higher for Aboriginal Australians across all age groups [3].
Type 2 diabetes (T2D) is of particular concern among Aboriginal Australians. Compared to non-Indigenous Australians, Aboriginal people are 3.3 times more likely to develop T2D and have almost 7 times the death rate from T2D [3]. The epidemic of diabetes is exacerbated by the poor quality diet consumed in remote Aboriginal communities [4] and the high prevalence of behaviours that contribute to weight gain [5]. Indeed, there is a desperate need for effective counter-measures to combat T2D among Aboriginal Australians.
While community controlled primary health care services can play a key role in delivering diabetes care to the Australian Aboriginal population [6] lifestyle interventions have been shown to be effective in reducing the prevalence and symptoms of T2D in a variety of cultural settings [7-10] including in Aboriginal cohorts[11]. In 1984, O’Dea [12] showed regression of T2D in an Aboriginal cohort within 7 weeks of returning them to their traditional environment and lifestyle. A key component of this lifestyle intervention was a low-fat eating pattern (13% of calories from fat) and physical activity.
In the research undertaken by O’Dea [12] in 1984, challenges returning Aboriginals to their traditional land and lifestyles were reported. These challenges have been further exacerbated over the past 30 years by advancing westernisation. Hence the purpose of this feasibility study was to examine the responsiveness of an at-risk Aboriginal cohort to a lifestyle intervention that advocated a low-fat eating pattern in combination with physical activity that did not displace them from their current living environment.
Methods
Study Design
This study used a pre-test/post-test design to examine the effectiveness of a well-established community-based lifestyle intervention that promotes a low-fat eating pattern and physical activity—the Complete Health Improvement Program (CHIP)—for reducing T2D risk factors among Aboriginal participants living in two rural locations within Australia.
Setting and participants
The setting for this study was two rural Australian locations: the Port Augusta in South Australia and Drouin in Victoria. In both these settings, a CHIP program was conducted.
In each location the local elders were contacted and their support was obtained for the study. Participants were recruited from the respective communities using print media, promotions in community meetings and recommendations from community elders.
Each participant paid $199 to enrol in the program. Time payment options were negotiated with individual participants when requested. Participants were encouraged to engage in the program in consultation with their personal health care provider and were specifically instructed not to make any changes to medication without consultation with their personal physician.
To be eligible for inclusion, the subjects were required to be of Aboriginal descent, over the age of 18, commit to attending 60% of the group sessions in the CHIP intervention and provide baseline and post-intervention data. Those participants who attended a CHIP program but did not meet the eligibility criteria were not enrolled in this study, but were still able to participate in the CHIP intervention. All eligible participants consented to participation.
Ethics clearance for the study was obtained from Avondale College of Higher Education Human Research Ethics Committee (Approval No. 20:10:07) and informed written consent was obtained from all participants for their data to be used.
Intervention
The CHIP intervention, described in detail elsewhere [13], is a well-published lifestyle intervention that has been shown to reduce risk factors associated with T2D in communities throughout Australasia [9, 14] and internationally [10, 15], as well as in low-socioeconomic settings [16].
The CHIP intervention involved 11 group sessions over 4 weeks. Each session was approximately 1.5 hours in duration and involved viewing a pre-recorded lecture presented by a health expert, cooking demonstrations and interactive group activities. The intervention had a nutrition focus, but the content of the program also addressed physical activity (advocating a daily target 10,000 steps measured by pedometers supplied to each participant) and elements from the positive psychology literature such as stress management and emotional wellbeing.
The eating pattern prescribed in the program was low-fat by the standards of national dietary guidelines and this was achieved by encouraging participants to move towards a whole food, plant-based diet ad libitum, with emphasis on the consumption of whole-grains, legumes, fresh fruits and vegetables. This diet was recommended in order to achieve a daily target of fewer than 20% of calories from fat and less than 10 teaspoons of added sugar, 5,000 mg of salt (2,000 mg of sodium) and 50 mg of cholesterol. Participants were also encouraged to consume 2 – 2.5 litres of water daily.
The interventions were facilitated by volunteers who undertook a two-day training course and had previously conducted CHIP interventions for non-Aboriginal participants. In the Port Augusta program one of the three facilitators was a local Aboriginal minister of religion. In the Drouin program, the facilitators worked closely with two local Aboriginal elders who assisted with the recruitment of participants and coordination of the group sessions.
Outcomes
At baseline and at the end of the intervention, body weight and blood pressure (BP) were recorded. Fasting blood samples were also collected at these two points and analysed for fasting plasma glucose (FPG) and lipid profile consisting of total cholesterol (TC), high-density lipoprotein (HDL) cholesterol, low-density lipoprotein cholesterol (LDL) and triglycerides (TG). At program entry, participants’ height, date of birth, gender, marital status were also recorded.
For the Port Augusta program baseline data, were collected on 10 August, 2014 and post intervention data were collected on 14 September, 2014 with the blood samples collected and analysed by SA Pathology. For the Drouin program, baseline data were collected on 31 January, 2015 and post intervention data were collected on 28 February, 2015 with the blood samples collected and analysed by Dorevitch Pathology. In both locations, the group sessions were conducted in the local Seventh-day Adventist church hall.
Statistical analysis
The data were analysed using IBM SPSS Statistics version 22. Paired T-tests were used to analyse pre to post-intervention changes in weight, body mass index (BMI), FPG, TC, HDL, LDL, TG and BP. Cohen’s d was calculated to indicate effect size with <0.2 considered small, >0.2 to <0.8 moderate and >0.8 large [17]. Alpha levels were set at p < 0.05. To further examine the effect of the intervention on participants at risk of T2D participants were stratified by baseline FPG to normal (≤5.5mmol/l) and elevated (>5.5mmol/l). To reduce the Type 1 error that can occur when simultaneous tests are performed in a data set, Bonferroni correction was applied to FPG. For this analysis the alpha level was set at 0.025.
Results
Twenty-five participants met the eligibility criteria for this study, 15 of the 22 individuals who enrolled for the intervention in Port Augusta and 10 of the 18 who enrolled in the Drouin program. The mean age of the participants was 44.4 ± 12.3 yrs with an age range of 25-70 yrs, seven of the participants were male and 18 were female. Participants attended on average 77.5% of the sessions. Nine of the participants were single, 14 were married and one chose not to provide their marital status.
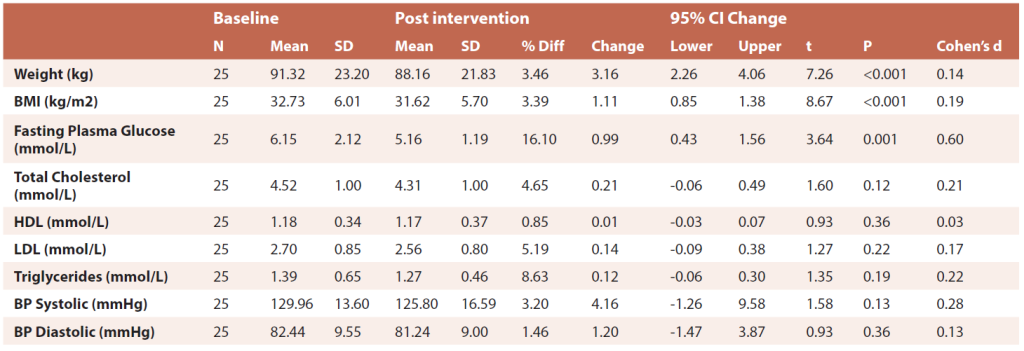
In 4 weeks, significant reductions were recorded in mean body weight, BMI and FPG, but not for BP or the range of lipids (Table 1). Body weight decreased on average 3.1 kg translating to a 3.5% reduction from baseline, with a small effect size. A 16.1% mean decrease in FPG, with a moderate effect size was observed.
The participants were stratified for baseline FPG and Table 2 shows the outcomes for the 11 participants who presented with FPG levels > 5.5 mmol/L at baseline. There was a large effect for mean FPG, with a decrease of 23.6% and a moderate effect for body weight, with a reduction of 4.12%.
Table 1 Baseline to post intervention changes paired T-Tests all participants
N= number, SD = standard deviation, CI = confidence interval
Table 2 Paired T-Tests pre-post intervention changes for participants with fasting plasma glucose > 5.5mmol/L at baseline
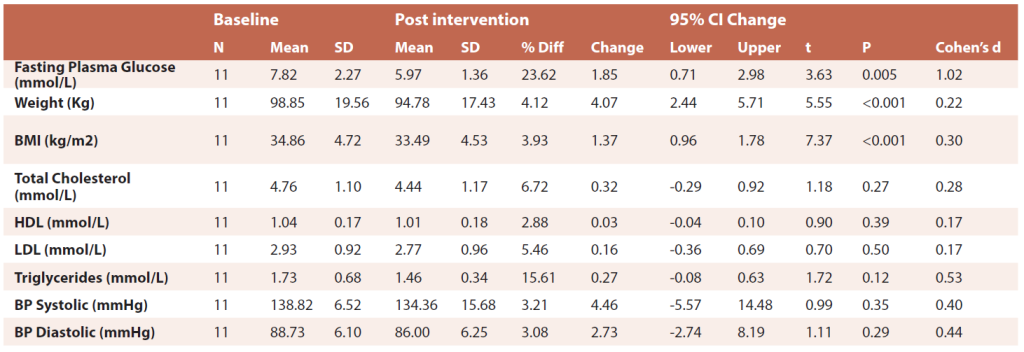
N= number, SD = standard deviation, CI = confidence interval
Discussion
This feasibility study indicates that rapid and meaningful reductions in body weight and FPG can be achieved in Aboriginal cohorts utilising a community-based lifestyle intervention that promotes a low-fat eating pattern and physical activity.
In the study by O’Dea, participants were transported 1.5 days travel by four-wheel drive to a remote location where they had no access to store foods or beverages for the duration of the intervention [12]. A feature of this study was that the participants achieve these results while remaining in their normal living environment. As the program sessions were 1.5 hours on three evenings per week, participants could go about their usual daily routine and not be dislocated from their family or community.
The mean changes in body weight and FPG observed in this study were substantive considering the short duration of the intervention. Increased body weight and raised FPG are important risk factors for T2D [18]. The landmark Diabetes Prevention Program study only had two objectives: decrease body weight by 7% within the first 6 months and increase physical activity (30 min per day) [19]. The participants in the present study made good progress toward this weight loss goal in just 4 weeks.
There were no changes in the lipid profile of participants in this study. This may have been, in part, due to the lower than expected mean baseline TC level of the participants (4.52 mmol/L) despite the elevated baseline BMI (35.5 kg/m2). Other studies have observed similar lower than expected levels total cholesterol in Aboriginal populations [12, 20, 21]. The CHIP intervention has been shown to reduce lipid profiles in other populations which showed higher mean cholesterol levels at baseline [9, 10, 15].
Another interesting element of this study is that it utilised volunteers to deliver the intervention. This keeps delivery costs down and is also of benefit because it enabled delivery in a manner that is appropriate in the local context by facilitators familiar with the community’s needs and who collaborated with community elders. Rowley and O’Dea [22] suggest that these factors are essential for an effective intervention in an Aboriginal population.
The methods used to achieve a low-fat eating pattern used in this study differed to that used by O’Dea. In the O’Dea study, the low-fat eating pattern was achieved by participants consuming very high levels of lean game meat which is low fat animal protein [10]. As it is difficult to achieve this using commercially available meat products, in the communities in this study the CHIP intervention advocated the use of a plant-based diet. While dietary analyses were not conducted in this study the typical fat content of participants completing CHIP is less than 20% [15].
A limitation of this study is the relatively small cohort. However, as previously stated, the intervention used in the study has been shown to be effective in a number of different populations [13]. A second limitation was the participation fee of $199 may have limited access to the program and been a source of bias. Out-of-pocket payments have been shown to create a financial barrier to participating in lifestyle interventions [23]. Conversely, monetary payments have been shown to increase participant motivation to succeed [24], with ‘skin in the game’ increasing participation and outcomes [25]. Furthermore, charging for the intervention can be seen to make the intervention desirable [26]. The level of participation fee that is appropriate for an Aboriginal community is yet to be determined.
As this study was limited to 4 weeks in duration, the long-term outcomes are unknown. None the less, a small New Zealand study found that 106 CHIP participants who returned for follow-up assessment, on average 4 years after completion of the intervention, were able to maintain improvements in most of their biometrics [14].
In conclusion, this feasibility study, showed that a lifestyle intervention promoting a low-fat eating pattern combined with physical activity reduced risk factors associated with type II diabetes in a rural Aboriginal cohort when conducted in their usual living environment. A multi-centre study with longer follow up is needed to further investigate the long-term effects, sustainability and cost-effectiveness of community-based lifestyle interventions targeting type II diabetes among Aboriginal populations.
References
- Stephens C, Nettleton C, Porter J, Willis R, Clark S. Indigenous peoples’ health–why are they behind everyone, everywhere? Lancet. 2005;366(9479):10-3.
- Ring I, Brown N. The health status of indigenous peoples and others. BMJ. 2003;327(7412):404-5.
- Australian Indigenous HealthInfoNet. Overview of Australian Indigenous health status, 2014. 2015 [cited 2015 11/06/2015]. Available from: http://www.healthinfonet.ecu.edu.au/health-facts/overviews.
- Brimblecombe JK, Ferguson MM, Liberato SC, O’Dea K. Characteristics of the community-level diet of Aboriginal people in remote northern Australia. Med J Aust. 2013;198(7):380-4.
- Hardy LL, O’Hara BJ, Hector D, Engelen L, Eades SJ. Temporal trends in weight and current weight-related behaviour of Australian Aboriginal school-aged children. Med J Aust. 2014;200(11):667-71.
- Stoneman A, Atkinson D, Davey M, Marley JV. Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal Community Controlled Health Services. BMC health services research. 2014;14(1):1.
- Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677-86.
- Davis-Smith YM, Boltri JM, Seale JP, Shellenberger S, Blalock T, Tobin B. Implementing a diabetes prevention program in a rural African-American church. J Natl Med Assoc. 2007;99(4):440-6.
- Morton DP, Rankin P, Morey P, Kent L, Hurlow T, Chang E, et al. The effectiveness of the Complete Health Improvement Program (CHIP) in Australasia for reducing selected chronic disease risk factors: a feasibility study. N Z Med J. 2013;126(1370):43-54.
- Morton D, Rankin P, Kent L, Sokolies R, Dysinger W, Gobble J, et al. The Complete Health Improvement Program (CHIP) and reduction of chronic disease risk factors in Canada. Can J Diet Pract Res. 2014;75(2):72-7.
- Rowley KG, Su Q, Cincotta M, Skinner M, Skinner K, Pindan B, et al. Improvements in circulating cholesterol, antioxidants, and homocysteine after dietary intervention in an Australian Aboriginal community. Am J Clin Nutr. 2001;74(4):442-8.
- O’Dea K. Marked improvement in carbohydrate and lipid metabolism in diabetic Australian aborigines after temporary reversion to traditional lifestyle. Diabetes. 1984;33(6):596-603.
- Morton D, Rankin P, Kent L, Dysinger W. The Complete Health Improvement Program (CHIP): History, Evaluation, and Outcomes. A J Lifestyle Med. 2014.
- Kent L, Morton D, Hurlow T, Rankin P, Hanna A, Diehl H. Long-term effectiveness of the community-based Complete Health Improvement Program (CHIP) lifestyle intervention: a cohort study. BMJ Open. 2013;3(11).
- Rankin P, Morton DP, Diehl H, Gobble J, Morey P, Chang E. Effectiveness of a volunteer-delivered lifestyle modification program for reducing cardiovascular disease risk factors. Am J Cardiol. 2012;109(1):82-6.
- Drozek D, Diehl H, Nakazawa M, Kostohryz T, Morton D, Shubrook JH. Short-term effectiveness of a lifestyle intervention program for reducing selected chronic disease risk factors in individuals living in rural appalachia: a pilot cohort study. Adv Prev Med. 2014;2014:798184.
- Cohen J. Statistical power analysis for the behavioral sciences: Lawrence Erlbaum; 1988.
- Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76-9.
- The Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25(12):2165-71.
- Wang Z, Hoy WE. Body mass index and mortality in aboriginal Australians in the Northern Territory. Aust N Z J Public Health. 2002;26(4):305-10.
- Wang Z, Hoy WE. Waist circumference, body mass index, hip circumference and waist-to-hip ratio as predictors of cardiovascular disease in Aboriginal people. Eur J Clin Nutr. 2004;58(6):888-93.
- Rowley KG, O’Dea K. Diabetes in Australian aboriginal and Torres Strait Islander peoples. P N G Med J. 2001;44(3-4):164-70.
- Rezayatmand R, Pavlova M, Groot W. The impact of out-of-pocket payments on prevention and health-related lifestyle: a systematic literature review. Eur J Public Health. 2013;23(1):74-9.
- Kruglanski AW, Riter A, Amitai A, Margolin B-S, Shabtai L, Zaksh D. Can money enhance intrinsic motivation? A test of the content-consequence hypothesis. J Personality Soc Pysch. 1975;31(4):744-50.
- Johnston CA, Rost S, Miller-Kovach K. Weight Watchers for the Facebook Era—How Does It Compare to the Do-It-Yourself Approach? Am J Med. 2013;126(3):102-5.
- Zimmerman FJ. Using behavioral economics to promote physical activity. Prev Med. 2009;49(4):289-91.