Determinants of asthma in Indigenous Australians: insights from epidemiology
ReviewBrock C1, McGuane J,1 (2018)
Determinants of asthma in Indigenous Australians: insights from epidemiology. Australian Indigenous HealthBulletin 18(2). Retrieved [access date] https://healthbulletin.org.au/articles/determinants-of-asthma-in-indigenous-australians
Australian National University Medical School
Corresponding author: Jonathan McGuane, Australian National University Medical School, email: u5983679@anu.edu.au
Abstract
Objective: Asthma prevalence is markedly higher in Aboriginal and Torres Strait Islander Australians compared to the non-Indigenous population, contributing to a significantly higher overall burden of disease-related morbidity and mortality. The purpose of this review was to utilise epidemiological studies conducted over the last decade to gain insight into the determinants of asthma and generate hypotheses regarding causal mechanisms.
Methods: Indigenous and national health surveys by the Australian Bureau of Statistics and the Australian Institute of Health and Welfare were reviewed and a literature search was conducted.
Results: There are marked differences in the prevalence of asthma between Indigenous and non-Indigenous people with respect to ageing and geographic locality. This may be attributable to exposure to specific risk factors around these parameters. The different potential causal mechanisms of asthma in both populations are discussed.
Conclusions: Although many of asthma’s intermediate and proximal disease determinants are shared between Indigenous and non-Indigenous Australians, different patterns of exposure to specific risk factors, plus inequities in disease care and management, likely underpin the higher prevalence in the Indigenous population.
Implications: Closing the gap in the burden of asthmatic disease between Indigenous and non-Indigenous Australians is likely to require structural reform to address the underlying social disadvantage that disproportionately affects Indigenous Australians.
(View PDF version – 440KB)
Introduction
Asthma is a respiratory disorder, defined by the Global Initiative for Asthma as ‘a heterogeneous disease usually characterised by chronic airway inflammation… (with a) history of respiratory symptoms such as wheeze, shortness of breath, chest tightness and cough that vary over time and in intensity, together with variable expiratory airflow limitation’ (1). In the 2004-05 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS), asthma was second only to eye/sight problems among illnesses afflicting Indigenous Australians (2, 3). The aetiopathology of asthma is, in general, poorly understood. It appears that a complex interplay of constitutional factors and environmental exposures during foetal life, infancy, and childhood determine whether an individual develops the disease. A huge number of extrinsic factors have been linked to asthma development, with varying levels of evidence (4). One difficulty in reporting asthma is the considerable variability in presentation and overlap of symptoms with other respiratory conditions, making diagnosis difficult, particularly in children (5). Complicating this, the varying availability of healthcare professionals in different regions means that diagnosis of asthma for reporting purposes can take different forms, from self-reported symptoms to doctor-diagnosed disease (6).
Epidemiology and burden of asthma in Australia
Despite a world-class healthcare system (7, 8) and a life expectancy at birth among the highest in the world (9), Australia has the highest prevalence of asthma globally (10). The cost of asthma must also be considered, and was quantified for guardians of 12-year olds to be $212.46 and 13.4 hours per year, quadrupling if hospital attendance was required, and 0.9% of the Australian health care budget, or $655 million (11, 12). Asthma is more common in Indigenous versus non-Indigenous Australians, with a prevalence among different adult age groups of 17.1 – 22.2% and 9.6 – 10.8%, respectively, according the most recent survey data (13). This finding is in agreement with earlier reports on Asthma in Australia from 2011 and 2008 (3, 6). Among children, the 2004-05 NATSIHS showed a negligible difference in asthma prevalence between Indigenous and non-Indigenous children 0-17 years)[1] (3, 6). In contrast, the 2012-2013 Australian Aboriginal and Torres Strait Islander Health Survey found prevalences of 14.6% and 9.3% in Indigenous and non-Indigenous children, respectively (13).
In the 2008 Asthma in Australia report, the prevalence of current asthma in non-Indigenous Australians is roughly maintained with advancing age in females, but decreases in males (3). This is consistent with the well-recognised ‘gender switch’ in asthma prevalence that occurs from males to females during adolescence, thought to be due to hormonal changes and/or gender-specific differences in environmental exposures (14). In contrast, asthma prevalence is markedly higher among female Indigenous adults compared to Indigenous children (3). Accordingly, hospital separation rates and mortality due to asthma is higher in Indigenous people, especially those aged 35 and over (6). The 2011 Asthma in Australia report demonstrated that in the Australian population as a whole, prevalence decreases in males from the age of 25, while among females, those >75 years had the highest prevalence, similar to the trends in the Indigenous population (6). These data are broadly in agreement with subsequent surveys (15). However, the prevalence in all adult Indigenous female age groups studied is much higher compared to their non-Indigenous counterparts (3).
Geographically, the burden of current asthma is clearly higher among Indigenous people living in non-remote communities compared to remote communities, although this difference disappears with advancing age due to increasing prevalence in the remote Indigenous population (3). The most recent data indicate that the highest prevalence among Indigenous people is found in major cities and inner regional areas, with little difference between these (16). In contrast, the prevalence of asthma in the general population is slightly lower in major cities compared to inner regional and outer regional/remote areas (6, 13). Given that Aboriginal and Torres Strait Islander Australians constitute a small minority of the Australian population (~3%) (17), these data arguably reflect trends in non-Indigenous Australians predominantly (assuming proportional representation in the survey).
Risk factors and potential causal mechanisms
Known risk factors for asthma include atopy, allergen exposure, occupational exposures, early (e.g., neonatal) abnormalities in pulmonary function, airway hyperreactivity, family history, early life exposure to bacteria and viruses (e.g., Respiratory Syncytial Virus) (18), (in girls) early menarche, maternal age, maternal diet, prematurity, neonatal jaundice, and caesarean delivery (4). The extent of the genetic contribution to asthma is unclear, although multiple genome wide association studies have identified candidate genes in moderate and severe asthmatics (19, 20). No studies investigating asthma candidate genes in Australian Indigenous populations have been conducted to date, but importantly, no significantly different asthma gene frequencies have been observed between people of European, American, African American, Caribbean or Latino ancestry, suggesting that asthma-associated genes are not isolated to specific ethnicities (20). From the epidemiological evidence above, a number of risk factors can be postulated for asthma development in Indigenous people specifically, while others may be excluded as major determinants, as discussed below. The Figure below depicts a multifactorial model of asthma incorporating known biological, social, and pathological factors affecting disease development.
Figure. Determinants of asthma development
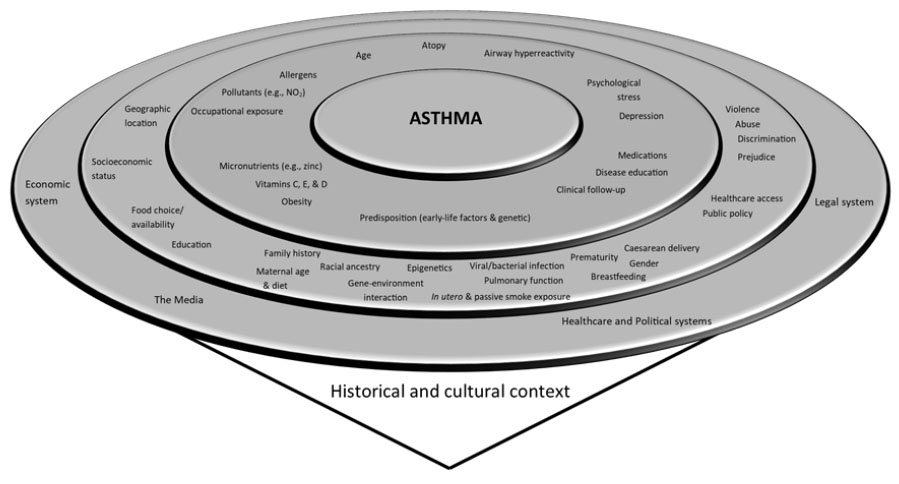
The historical and cultural contexts of Indigenous and non-Indigenous Australians underlie the ways in which these populations interact with the distal determinants of asthmatic disease (outer ring). These systemic influences give rise to factors that impact on disease development for individuals at an intermediate level (middle ring), which in turn govern the proximal determinants (inner ring) of asthma. Adapted from (4, 44, 45).
Smoking
Smoking is commonly associated with chronic respiratory conditions, and although the proportion of Indigenous adults ≥15 years who smoke is 2.6 times higher than that of the non-Indigenous population (16), there is no difference in current smoking rates between those who have asthma and those who do not in either population (3, 21). However, a history of smoking is more commonly reported in people with asthma (21). Moreover, in utero and childhood passive smoke exposure have been associated with asthma development (22-25), and are greater in Indigenous vs non-Indigenous populations (26-28), suggesting that this may play some role. A potential mechanism is via adverse effects on lung development and growth (24), resulting in predisposition to airway hyperreactivity and reduced pulmonary function.
Age and sex
Cumulative exposure to risk factors over the life-course of Indigenous people, such as pollutants, stress, dietary deficiencies, and chronic under-treatment of subclinical asthma, coupled with predisposition as a result of in utero or early life exposures (e.g., maternal smoking), may lead to the increased prevalence with age in this population (4). Misdiagnosis of other chronic respiratory diseases, such as chronic obstructive pulmonary disease and bronchiectasis, may also play a role (3). Given that this effect is seen in females only, an interaction between age and sex seems likely. However, the fact that no post-menopausal (i.e., in the 55 years and older group) drop in current asthma prevalence is seen suggests that factors other than female sex hormones are responsible for the high burden of disease in this age group (3, 6); these remain to be elucidated.
In non-Indigenous males, the prevalence of asthma is highest in childhood and/or young adulthood (3, 6, 15). It has been suggested that prevalence is higher in males compared to females at this age because of greater prevalence of atopy, structural airway differences, and altered symptom reporting (4). This pattern also suggests spontaneous remission in a proportion of patients, consistent with data from the Tasmanian Longitudinal Health Study (29). This study found that 65% of childhood (i.e., at 7 years) asthmatics had remitted in middle age, of whom a slight majority (55.1%) were male. The authors suggested that early, aggressive treatment of allergic rhinitis and eczema (both atopic conditions associated with asthma) promoted remission in adulthood. The implication is that disparities in healthcare access may in part underlie the age-related differences in asthma prevalence between Indigenous and non-Indigenous people.
Locality
Non-remote locality increased the risk of asthma prevalence 2.5 fold in the 2012-13 NATSIHS. Given that – despite perhaps popular sentiment to the contrary – the majority (~80%) of Indigenous people reside in non-remote classification areas (17) , the importance of this risk factor may be high. A possible distal determinant of this difference is the decreased economic opportunities afforded Indigenous people that result in lower socioeconomic status (30), which is known to be linked to asthma prevalence (6, 15). Economic poverty will influence housing choices made by Indigenous people (i.e., requiring cheaper rent/mortgage payments) (31), which can often mean living on or in close proximity to a major road, or in more industrialised areas. This is turn results in increased exposure to vehicular and industrial pollutants especially nitrogen dioxide and diesel particulate matter, both known respiratory irritants (32, 33) and risk factors for asthma development (4, 34).
Geographic location in non-remote areas spatially or environmentally distant from ‘country’ could also contribute to psychological stress and depression (35), both of which are associated with asthma development. In a vicious cycle, chronic diseases such as asthma also fuel higher rates of psychological distress among Indigenous people (35). Finally, Australians experiencing higher levels of relative socioeconomic disadvantage are also less likely to exercise (15), contributing to obesity and (secondarily) asthma development (36).
Unlike the Indigenous population, there is an increase in asthma prevalence among those living in inner regional areas compared to major cities among the Australian population as a whole (6, 15). One potential contributor to this is the fact that there are around half the number of General Practitioners and Specialists in inner and outer regional areas compared to major cities (37). This could result in reduced healthcare accessibility and chronic under-treatment of sub-clinical asthma. Arguing against this is the fact that the availability of doctors is even lower in outer regional and remote areas, with no concomitant increase in current asthma prevalence. Mitigating factors such as lower pollution levels may be relevant in this comparison.
Conclusion
The prevalence of asthma is higher in Indigenous Australians, with an altered geographic and age-related distribution compared to non-Indigenous Australians. In individuals of both populations, many of the same intermediate and proximal determinants underlie asthma development. The difference in prevalence is likely due in part to increased/prolonged exposures to specific risk factors, as well as a lack of culturally-appropriate asthma education and service delivery (38, 39); both of which are important components of holistic asthma care (40-42). More broadly, poorer quality engagement with the Australian economic, healthcare, political and legal systems, and the media (43), against a background of historical dislocation and cultural dispossession, negatively impact asthma prevalence in Indigenous Australians (see Figure). Distrust in government agencies and ‘Western’ health care systems contributes significantly to this (27, 28). It seems probable that the disparity in Australian asthma burden, along with that due to other chronic diseases, will not be rectified until the long-standing inequalities affecting Indigenous people in Australian society are resolved.
References
- Global strategy for asthma management and prevention. Global Initiative for Asthma; 2016.
- Trewin D. National Aboriginal and Torres Strait Islander Health Survey 2004-05. Canberra: ABS: ABS (Australian Bureau of Statistics); 2006. Contract No.: ABS Cat. no. 4715.0.
- Marks G, Poulos L, Ampon R, Waters A-M. Asthma in Australia 2008. Canberra: AIHW: Australian Centre for Asthma Monitoring; 2008. Contract No.: Cat. no. ACM 14.
- Litonjua AA, Weiss ST. Risk factors for asthma: UpToDate; 2016 [updated 29/04/2016. Available from: http://www.uptodate.com/contents/risk-factors-for-asthma#H15.
- Lang DM, Erzurum SC, Kavu M. Asthma: Cleveland Clinic Center for Continuing Education; 2010
- Marks G, Reddel H, Cooper S, Poulos L, Ampon R, Waters A-M. Asthma in Australia 2011. Canberra: AIHW: Australian Centre for Asthma Monitoring; 2011. Contract No.: Cat. no. ACM 22.
- The World Health Report 2000 : health systems : improving performance. Geneva: World Health Organization; 2000.
- Schneider EC, Sarnak DO, Squires D, Shah A, Doty MM. Mirror, Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care. The Commonwealth Fund; 2017.
- World Health Statistics 2016: monitoring health for the SDGs, sustainable development goals. France: World Health Organization; 2016.
- To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12(1):1-8.
- Poulos LM, Toelle BG, Marks GB. The burden of asthma in children: an Australian perspective. Paediatr Respir Rev. 2005;6(1):20-7.
- Asthma hospitalisations in Australia 2010-11. Canberra: AIHW: Australian Institute of Health and Welfare; 2013. Contract No.: Cat. no. ACM 27.
- Asthma: Australian Institute of Health and Welfare; 2017 [updated 22 Dec 2017].
- Almqvist C, Worm M, Leynaert B, for the working group of GALENWPG. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63(1):47-57.
- National Health Survey: First Results, 2014-15. ABS (Australian Bureau of Statistics); 2016. Contract No.: Cat. no. 4364.0.55.001.
- Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2012-13: Australian Bureau of Statistics; 2013
- Estimates of Aboriginal and Torres Strait Islander Australians, June 2011. ABS, Australian Bureau of Statistics; 2013. Contract No.: Cat. no. 3238.0.55.001.
- Busse WW, Lemanske RF, Jr., Gern JE. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376(9743):826-34.
- Wan YI, Shrine NR, Soler Artigas M, Wain LV, Blakey JD, Moffatt MF, et al. Genome-wide association study to identify genetic determinants of severe asthma. Thorax. 2012;67(9):762-8.
- Torgerson DG, Ampleford EJ, Chiu GY, Gauderman WJ, Gignoux CR, Graves PE, et al. Meta-analysis of genome-wide association studies of asthma in ethnically diverse North American populations. Nat Genet. 2011;43(9):887-92.
- Asthma, associated comorbidities and risk factors: Australian Institute of Health and Welfare; 2016 [updated 23 Aug 2016].
- Alati R, Al Mamun A, O’Callaghan M, Najman JM, Williams GM. In Utero and Postnatal Maternal Smoking and Asthma in Adolescence. Epidemiology. 2006;17(2):138-44.
- Peat JK, Toelle BG, Marks GB, Mellis CM. Continuing the debate about measuring asthma in population studies. Thorax. 2001;56(5):406-11.
- Skorge TD, Eagan TML, Eide GE, Gulsvik A, Bakke PS. The Adult Incidence of Asthma and Respiratory Symptoms by Passive Smoking In Utero or in Childhood. American Journal of Respiratory and Critical Care Medicine. 2005;172(1):61-6.
- Landau LI. Parental smoking: asthma and wheezing illnesses in infants and children. Paediatric Respiratory Reviews. 2001;2(3):202-6.
- Chan A, Keane RJ, Robinson JS. The contribution of maternal smoking to preterm birth, small for gestational age and low birthweight among Aboriginal and non-Aboriginal births in South Australia. Med J Aust. 2001;174(8):389-93.
- Glasgow NJ, Goodchild EA, Yates R, Ponsonby AL. Respiratory health in Aboriginal and Torres Strait Islander children in the Australian Capital Territory. J Paediatr Child Health. 2003;39(7):534-9.
- Chang AB, Shannon C, O’Neil MC, Tiemann AM, Valery PC, Craig D, et al. Asthma management in indigenous children of a remote community using an indigenous health model. Journal of Paediatrics and Child Health. 2000;36(3):249-51.
- Burgess JA, Matheson MC, Gurrin LC, Byrnes GB, Adams KS, Wharton CL, et al. Factors influencing asthma remission: a longitudinal study from childhood to middle age. Thorax. 2011.
- Biddle N. CAEPR Indigenous Population Project 2011 Census Papers: Socioeconomic outcomes. Australian National University Centre for Aboriginal Economic Policy Research; 2013.
- Hunter B. Indigenous Australians and the socioeconomic status of urban neighbourhoods. The Australian National University Centre for Aboriginal Economic Policy Research; 1996. Contract No.: No. 106/1996.
- Baldacci S, Viegi G. Respiratory effects of environmental pollution: epidemiological data. Monaldi Arch Chest Dis. 2002;57(3-4):156-60.
- Wong GW, Lai CK. Outdoor air pollution and asthma. Curr Opin Pulm Med. 2004;10(1):62-6.
- Modig L, Toren K, Janson C, Jarvholm B, Forsberg B. Vehicle exhaust outside the home and onset of asthma among adults. Eur Respir J. 2009;33:1261-7.
- The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples, Oct 2010. ABS (Australian Bureau of Statistics); 2010. Contract No.: Cat. no. 4704.0.
- Sybilski AJ, Raciborski F, Lipiec A, Tomaszewska A, Lusawa A, Furmańczyk K, et al. Obesity – a risk factor for asthma, but not for atopic dermatitis, allergic rhinitis and sensitization. Public Health Nutrition. 2015;18(3):530-6.
- Australian Social Trends, April 2013. ABS, Australian Bureau of Statistics; 2013. Contract No.: Cat. no. 4102.0.
- Dawson A, Russel A, Caponi A. Asthma Project at Pika Wiya Health Services: Identifying Barriers and Developing Resources Aboriginal and Islander Health Worker Journal. 2003;27(5):20-2.
- Eley R, Gorman D. Music Therapy to Manage Asthma. Aboriginal and Islander Health Worker Journal. 2008;32(1):9-10.
- Coughlan J, Wilson A, Gibson PG. Evidence-based review of the Australian six step asthma management plan. In: Department NSWH, editor. Sydney1999.
- Chang AB, Taylor B, Masters IB, Laifoo Y, Brown ADH. Indigenous healthcare worker involvement for Indigenous adults and children with asthma. Cochrane Database of Systematic Reviews. 2007(4).
- Enarson DA, Ait-Khaled N. Cultural barriers to asthma management. Pediatric Pulmonology. 1999;28(4):297-300.
- Baum F. Want to improve the nation’s health? Start by reducing inequalities and improving living conditions. The Conversation [Internet]. 2016 01/09/2016.
- Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, et al. Approaching Health Disparities From a Population Perspective: The National Institutes of Health Centers for Population Health and Health Disparities. American Journal of Public Health. 2008;98(9):1608-15.
- Forno E, Gogna M, Cepeda A, Yañez A, Solé D, Cooper P, et al. Asthma in Latin America. Thorax. 2015;70(9):898-905.
[1] A possible exception to this is infants <1 year, in whom prevalence of current asthma was reported as higher in the Indigenous population in the NATSIHS. However, because the diagnosis of asthma at this age is uncertain, and the increased prevalence of other respiratory conditions such as bronchiolitis in Indigenous populations (11, 12), this finding is tentative.



