Review of tobacco use among Aboriginal and Torres Strait Islander peoples
ReviewColonna E1, Maddox R1, Cohen R1, Marmor A1, Doery K1, Thurber K A1, Thomas D2, Guthrie J1, Wells S1, Lovett R1
- Aboriginal and Torres Strait Islander Health Program, National Centre for Epidemiology and Population Health, Australian National University.
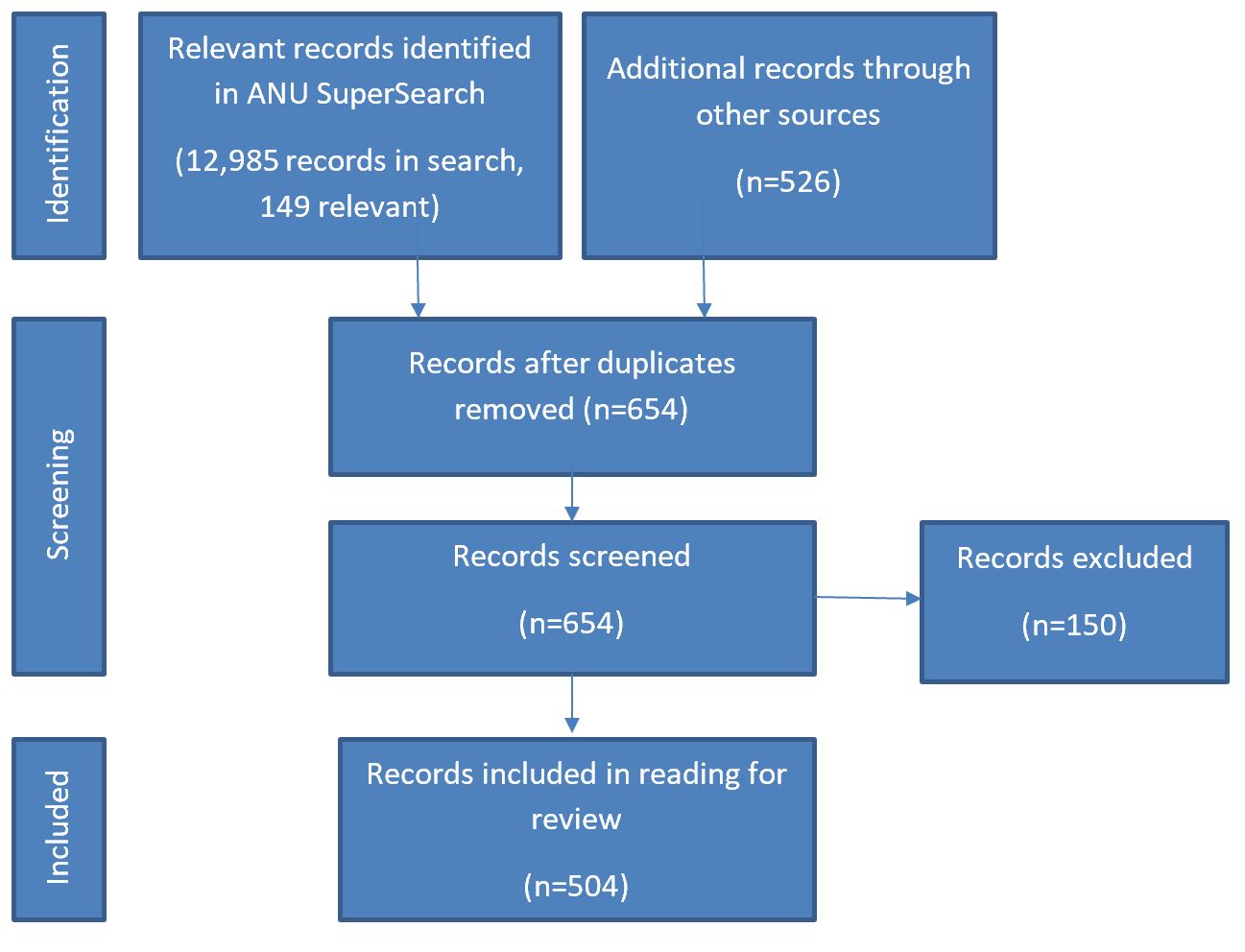
- Menzies School of Health Research.
Corresponding author: Emily Colonna Emily.Colonna@anu.edu.au, 54 Mills Road Acton ACT 2601 ph: +61 2 6125 8417
Suggested citation:
Colonna. E., Maddox, R., Cohen, R., Marmor, A., Doery, K., Thurber, K. A., Thomas, D., Guthrie, J., Wells, S., Lovett R. (2020). Review of tobacco use among Aboriginal and Torres Strait Islander peoples. Australian Indigenous HealthBulletin, 20(2). Retrieved from https://aodknowledgecentre.ecu.edu.au/learn/specific-drugs/tobacco/
Download PDF 2.9MB
Contents
Introduction
About this review
Acknowledgements
Key facts
Tobacco use
Aboriginal and Torres Strait Islander population
The context of tobacco use among Aboriginal and Torres Strait Islander peoples
Extent of tobacco use among Aboriginal and Torres Strait Islander peoples in Australia
How smoking affects your body and health
Tobacco-related disease burden
Tobacco-related mortality
Impact on community and culture
Factors related to tobacco use among Aboriginal and Torres Strait Islander peoples
National policies and strategies impacting tobacco use
Tobacco control policies and their impact on Aboriginal and Torres Strait Islander peoples
Policies related to tobacco use among Aboriginal and Torres Strait Islander peoples
Programs to address tobacco use among Aboriginal and Torres Strait Islander peoples
Opportunities in addressing tobacco use
Concluding comments and future directions
Appendix 1: Glossary and acronyms
Appendix 2: Smoking and health conditions
Appendix 3: Literature search strategy
References.
Introduction
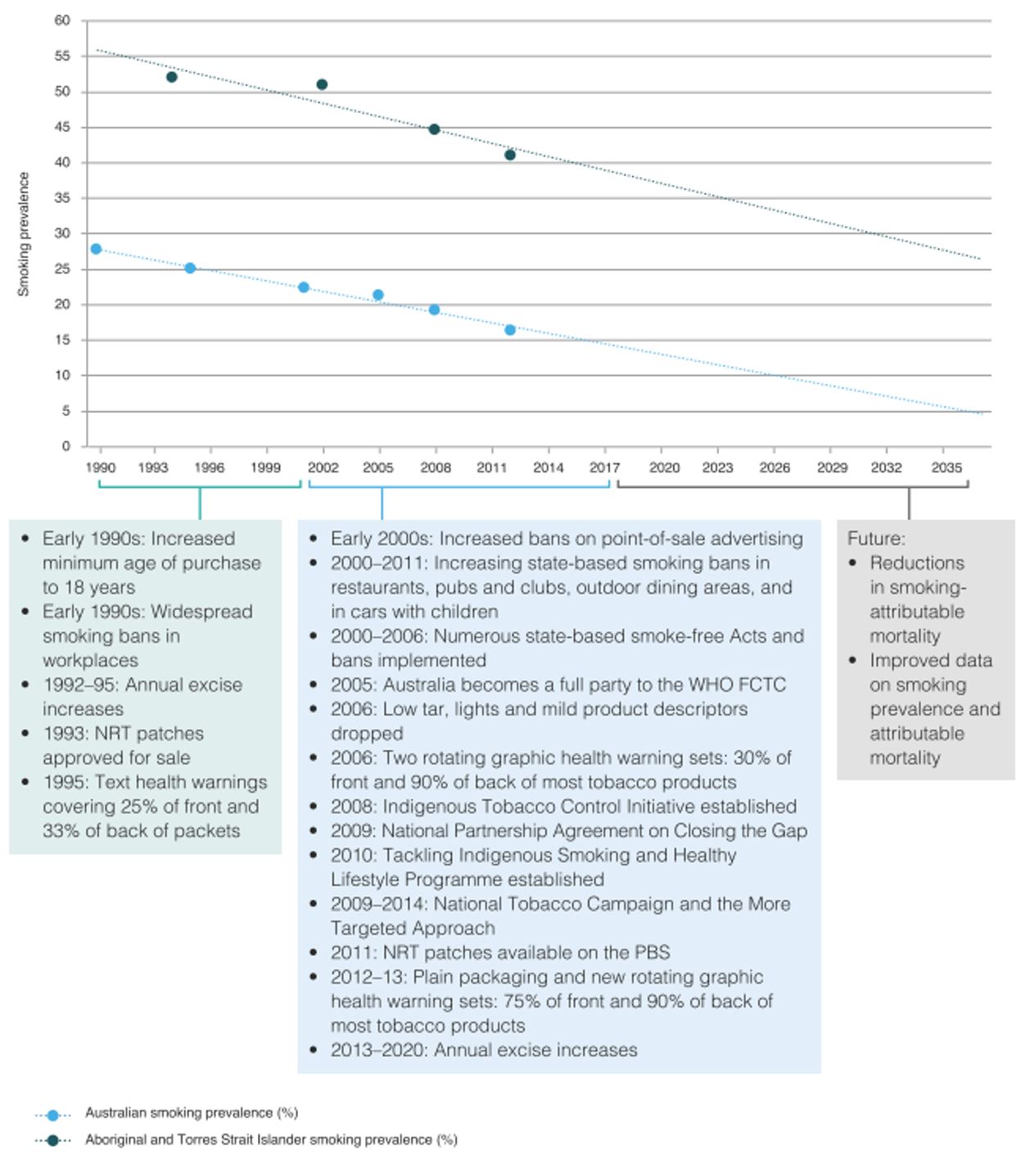
Tobacco use is the leading contributor to the burden of disease for Aboriginal and Torres Strait Islander peoples and is both an issue of great concern and an area for considerable health gains [1]. Reducing tobacco use is achievable. Substantial progress has already been made, with a 9.8 percentage point reduction in the prevalence of daily smoking for those aged 18 years and over from 2004–05 to 2018–19 from 50.0% to 40.2% [2]. This is a promising development, after a period of limited change in the preceding decade [3]. Further reductions in tobacco use will continue to enhance the health and wellbeing of Aboriginal and Torres Strait Islander peoples.
This review takes a strengths-based approach to examine tobacco use in detail, specifically in the Aboriginal and Torres Strait Islander context. Often, Aboriginal and Torres Strait Islander health is viewed through comparative statistics with the non-Indigenous population which can reproduce deficit discourse [4, 5]. These comparisons can also obscure the diversity of nations, cultures, perspectives, languages and experiences that Aboriginal and Torres Strait Islander peoples represent. This review moves beyond comparison to understand Aboriginal and Torres Strait Islander peoples’ tobacco use in context. Unless explicitly stated, literature and evidence presented are specific to the Aboriginal and/or Torres Strait Islander population.
Context is vital to accurately and meaningfully understand tobacco use among Aboriginal and Torres Strait Islander peoples. Beyond establishing the existence of health gaps and substantial opportunities for improvement, it is important to understand the mechanisms by which inequities arose and endure [6]. Within the diversity, Aboriginal and Torres Strait Islander peoples share a common history of colonisation, with negative impacts that continue today [6-8]. As such, the review situates tobacco use within the contexts of enduring and evolving Aboriginal and Torres Strait Islander peoples’ cultures and societies, historical and contemporary trauma, tobacco industry interference and the social and cultural determinants of health.
This contextualisation is also important to avoid reproducing deficit discourse or colonialist ways of knowing and doing that focus on ill health and disadvantage [9]. Contextualisation can assist in addressing the inaccurate and misleading notion that there is a biological basis for the higher rates of tobacco use among Aboriginal and Torres Strait Islander peoples compared with other Australians. This includes fallacies that Indigenous peoples are genetically or biologically predisposed to addiction. These notions are a form of deficit discourse based on ideas of racial inferiority [5] and there is no evidence to support these claims.
Finally, the review acknowledges the complexity of tobacco use. It expands beyond the binary of smoker/non-smoker to examine a range of behaviours relating to tobacco use, including: initiation, smoking, attitudes, starting quit attempts, successful cessation and second-hand smoke exposure.
These approaches to understanding the literature will assist in determining what is known about tobacco use, what has worked to reduce tobacco use, and what can be done in the future to further enhance the health and wellbeing of Aboriginal and Torres Strait Islander peoples.
About this review
The purpose of this review is to provide a comprehensive synthesis of key information on tobacco use among Aboriginal and Torres Strait Islander peoples in Australia to:
- inform those involved or who have an interest in Aboriginal and Torres Strait Islander health, in particular tobacco use, and
- provide the evidence for policy, strategy and program development and delivery.
The review provides general information on the historical, social and cultural context of tobacco use, and the factors that contribute to tobacco use. It provides information on the extent of tobacco use, including: incidence and prevalence data; hospitalisations and health service utilisation and mortality. It discusses the issues related to tobacco use, and provides information on relevant policies and strategies that address tobacco use among Aboriginal and Torres Strait Islander peoples. It concludes by discussing possible future directions in Australia.
Evidence shown is mainly focused on smoking commercial cigarettes as these are the primary cause of tobacco-related harm and the focus of available data sources. However, as this focus does not capture the extent of tobacco use, the review includes evidence on chewing tobacco and electronic cigarettes (e-cigarettes) where available.
This review takes a human rights and social justice approach. Specifically, the review is underpinned by the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) and the Framework Convention on Tobacco Control (FCTC) [10, 11]. This acknowledges that ‘Indigenous peoples have the right to self-determination’ [10, p.4] and recognises the disproportionate harm caused by commercial tobacco to Indigenous peoples [11]. Consistent with National Health and Medical Research Council Ethical conduct in research with Aboriginal and Torres Strait Islander peoples and communities: guidelines for researchers and stakeholders 2018 and Keeping research on track II 2018, Aboriginal and Torres Strait Islander peoples were involved in all aspects of the review [12, 13].
This review draws mostly on journal publications, government reports, national data collections and national surveys, the majority of which can be accessed through the HealthInfoNet’s publications database (http://aih-wp.local/key-resources/publications). Information specifically about tobacco use is available at: http://aod-wp.local/learn/specific-drugs/tobacco
Edith Cowan University prefers the term ‘Aboriginal and Torres Strait Islander’ rather than ‘Indigenous’ for its publications. However, when referencing information from other sources, authors may use the terms from the original source. As a result, readers may see these terms used interchangeably with the term ‘Indigenous’ in some instances. If they have any concerns, they are advised to contact the HealthInfoNet for further information.
Acknowledgements
Special thanks are extended to:
- the anonymous reviewer whose comments assisted finalisation of this review
- staff at the Australian Indigenous HealthInfoNet for their assistance and support
- the Australian Government Department of Health for their ongoing support of the work of the Australian Indigenous HealthInfoNet
- Glen Benton, Partnerships Officer – Aboriginal Quitline, Quit Victoria, for his feedback on the impacts of colonisation and future directions of this review.
Key facts
- Colonisation is an important factor contributing to tobacco use. Tobacco was introduced (and its use entrenched) by colonisers. In addition, colonisation led to ongoing trauma, stress, racism and exclusion from economic structures, and these factors are all associated with tobacco use.
- Tobacco use is the leading contributor to the burden of disease for Aboriginal and Torres Strait Islander peoples, and therefore, there is substantial potential for health gains through reducing tobacco use.
- Smoking harms almost every organ and body system. Most of the tobacco-related harm comes from atherosclerotic diseases (mainly coronary heart disease), cancers, chronic lung disease, and type 2 diabetes.
- Quitting smoking (or never smoking at all) is important. Quitting smoking at any age can reverse the health risks linked to smoking, and the earlier you quit, the better.
- Evidence shows that people want to quit. Sixty-nine percent of people who smoke daily had ever made a quit attempt, and 48% had made a quit attempt in the past year. Quitting smoking is supported by: knowledge of the health impacts of smoking – both for the smoker and those around them; denormalisation of smoking; support of family and friends; and wanting to be a role model for family and community.
- Reducing tobacco use is achievable and substantial progress has already been made, with a 9.8 percentage point reduction in the prevalence of adult daily smoking since 2004. This will lead to substantial health gains.
- Current daily smoking prevalence for adults (aged ≥18 years) is 40.2%. Smoking is less common among younger adults compared with older adults. Smoking is also less common in those living in urban and regional areas compared with those living in remote areas.
- Community, health services and governments are running a range of programs to support people to quit smoking, to never start smoking, and to reduce exposure to second-hand smoke. Effective programs are culturally appropriate and use holistic approaches to address the complex issue of tobacco use.
- Programs to address tobacco use could be strengthened through expanded coverage, long‑term funding, and rigorous evaluation evidence.
- Continued vigilance is required to restrict the tobacco industry’s promotion of tobacco use and its attempts to undermine policies and activities to reduce tobacco use.
Tobacco use
Nicotine
A key factor for why people smoke is the enjoyment it provides [14]. Smoking can help people to feel alert, happy, relaxed and good. Inhalation of nicotine triggers the release of psychoactive neurotransmitters, such as dopamine which influences smoking behaviour via pharmacological feedback. These neurotransmitters produce a rewarding effect for the user and are the basis of the mood altering effects of nicotine [15].
Nicotine dependence is an important factor in why people continue to smoke and have difficulties quitting [15]. Subsequent nicotine exposure reinforces the pleasurable effects which causes tolerance via neuroadaptation and leads to dependence. Once dependent, people then smoke to avoid the undesirable symptoms of withdrawal, for example anxiety and stress.
Definitions
This review uses the term ‘tobacco use’ to include multiple kinds of tobacco use and exposure that impact the health of Aboriginal and Torres Strait Islander peoples. These include:
- Commercial tobacco
- Second-hand smoke exposure
- Tobacco use also includes the exposure of others to second-hand smoke. The smoke inhaled and exhaled by the smoker (mainstream smoke) and the smoke created by the burning of the cigarette (sidestream smoke) contain a similar range of chemicals, however they differ in the proportions and absolute amount of chemicals. Sidestream smoke is three times more toxic than mainstream smoke, containing double the amount of nicotine and carbon monoxide and 15 times more formaldehyde than mainstream smoke [17, 18].
- Native tobacco (pituri, bush tobacco)
- While the importation of commercial chewing tobacco has been banned in Australia since 1991 [19], there are several plants containing nicotine that Aboriginal and Torres Strait Islander peoples in some parts of Australia have historically used, and in some cases continue to use.
- These plants include bush tobaccos and pituri and are not smoked, but chewed and held in the mouth or stored elsewhere on the body, where the nicotine is absorbed through the skin [20-22].
- E-cigarettes
- E-cigarettes are battery operated devices that heat a liquid which produces an inhalable vapour. The liquid varies in composition, typically containing solvents and flavouring agents, and may or may not contain nicotine. It is illegal to sell e‑cigarettes that contain nicotine in Australia [23].
Although the ABS do not include native tobaccos or e-cigarettes in their definition of smoking, both are relevant to reporting tobacco use among Aboriginal and Torres Strait Islander peoples.
Aboriginal and Torres Strait Islander population
In 2019, the Aboriginal and Torres Strait Islander population was estimated at 847,190 people and comprised 3.3% of the total Australian population [24]. Of this, 91% were Aboriginal, 5% were Torres Strait Islander and 4% were both Aboriginal and Torres Strait Islander [25].
The population is highly dispersed across the country. The largest number of Aboriginal and Torres Strait Islander people live in New South Wales (NSW) (281,107), and Queensland (Qld) (235,962) and the smallest number live the Australian Capital Territory (ACT) (8,178) [25]. Despite smaller numbers in the Northern Territory (NT), Aboriginal and Torres Strait Islander peoples make up the highest proportion, 32% (77,605 people), of the population of all the states and territories. Conversely, Victoria (Vic) has the lowest proportion of Aboriginal and Torres Strait Islander people, 0.9% (62,074 people). Two thirds (64%) of Torres Strait Islander people live in Qld with the second largest number of Torres Strait Islander people living in NSW at 15%.
The population is a young population. The median age is 23 years with 33% of the population aged under 15 years and 4.9% aged 65 years or over [24, 26].
Most Aboriginal and Torres Strait people live in major cities and regional areas. In 2016, more than a third (37%) of Aboriginal and Torres Strait Islander peoples lived in major cities, 44% lived in regional areas, and 19% lived in remote areas [25].
The context of tobacco use among Aboriginal and Torres Strait Islander peoples
Pre-colonial use of tobacco
There are limited documented accounts of Aboriginal and Torres Strait Islander peoples’ use of tobacco prior to colonisation. Existing accounts indicate that Aboriginal and Torres Strait Islander peoples did not smoke tobacco, but in some areas of Qld, Western Australia (WA) and NT, people chewed the leaves of nicotine-containing plants, including pituri (Duboisia hopwoodii) and over twenty species of bush tobacco (Nicotiana spp.) [21, 27, 28] (see Chewing native tobacco for more information).
From around 1700, Macassan fishermen from the Indonesian island now known as Sulawesi traded tobacco and pipes with Aboriginal people from the Kimberley region of North West WA to the Gulf of Carpentaria in northern Qld to facilitate relationships and for permission to fish in their waters [27, 28]. Tobacco smoking was also introduced into Cape York and the Torres Strait region prior to the 1800s, though it is not known by whom [28, 29]. Given that tobacco was only available in certain seasons, it is unlikely that smoking tobacco would have been habitual during this period [27, 28]. Further, it is likely that people in south-eastern Australia did not use tobacco prior to colonisation [30].
Colonial introduction to tobacco
From 1788, European colonisers introduced British tobacco across Australia [28]. Tobacco was often used in first encounters between colonisers and Aboriginal and Torres Strait Islander people, as a gesture of goodwill [27, 28, 31, 32]. In diaries and letters, colonists describe carrying tobacco to give to Aboriginal and Torres Strait Islander people to assist in establishing relationships [33]. In the early 20th century, a chief protector of Aborigines, W.G. Stretton described tobacco as a ‘civilizing influence’ and as a way of eliciting help from Aboriginal and Torres Strait Islander peoples [34]. He wrote:
There can be no better civilising influence than that of continually moving about among the various tribes, each time taking a little tobacco or coloured cloth. How often has the weary traveller had to trust to the natives for a drink of water! [34]
Once introduced to tobacco, it became a highly desired good and Aboriginal and Torres Strait Islander peoples actively sought it from colonisers [27, 28, 31, 33].
This desire for, and addiction to tobacco was exploited by colonisers to advance their economic, political and social goals [35, 36]. Colonisers often used tobacco as an inducement to labour. In many instances, providing labour in exchange for tobacco meant living in settlements or on missions and adopting European ways of living – including conversion to Christianity [27, 28, 30, 36]. Tobacco was also provided as a part of government and employer rations, which continued until the 1940s, and on some cattle stations until 1968 [37]. Addiction to tobacco acted as a form of bondage as people became more dependent on the rations, including tobacco [33].
Tobacco was also used as an enticement to procure Aboriginal and Torres Strait Islander cultural and intellectual property [27, 28, 30, 36]. Scientists, collectors, and missionaries offered tobacco in exchange for items of material culture, instruction in languages, photographs, stories, witnessing ceremonies, and information about plants and animals. Geologist and anthropologist Charles Chewings (1859–1937) noted: ‘If you desire some article they possess and value you can offer nothing more tempting than tobacco in exchange for it’ [38, p.30].
While it is documented that some Aboriginal communities in the NT, Qld and NSW enacted agency in trading tobacco, the unequal power structures meant that the relationships were ultimately detrimental to them [33]. This detriment was partially intentional or known, in that colonisers knowingly used the addictive nature of tobacco to manipulate people and extort labour, goods and services. It also disrupted Aboriginal and Torres Strait Islander peoples’ culture and connection with Country. Beyond these damages, the introduction of tobacco was detrimental to Aboriginal and Torres Strait Islander peoples’ health, though the extent of the health effects of tobacco use were not known during the early colonial period [33]. The use of tobacco by colonisers served to entrench tobacco use in the population, disrupting the culture, exploiting labour and causing harms to the health of Aboriginal and Torres Strait Islander peoples. Further, it is likely that these processes contributed to widespread use of tobacco by both males and females from the beginning of the tobacco epidemic [33].
In the twentieth century, the use of tobacco by Aboriginal and Torres Strait Islander peoples expanded dramatically [39] with the increasing power and mass-marketing of the tobacco industry, in spite of growing evidence of the harms caused by tobacco in the second half of the century [19, 40].
Extent of tobacco use among Aboriginal and Torres Strait Islander peoples in Australia
Smoking prevalence
The most recent, nationally-representative estimates of Aboriginal and Torres Strait Islander smoking behaviours come from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) [2]. In this survey, current smoking refers to regular smoking of cigarettes, cigars, pipes or other tobacco products [16]. Current smoking includes those who smoke daily (current daily smoking) and those who smoke less than daily (current less-than-daily smoking). When reporting contemporary (2018–19) smoking prevalence, this review presents data for current smoking, as well as the breakdown by daily smoking and less-than-daily smoking.
The earliest data on smoking prevalence comes from the 1994 National Aboriginal and Torres Strait Islander Survey (NATSIS). In this survey, data was only collected on current smoking of any amount (that is, daily and less-than-daily combined). So in this review, when describing long-term trends in smoking prevalence, from 1994 to 2018–19, the prevalence of any current smoking is reported. When describing recent smoking trends, focusing on the last 15 years, only current daily smoking is reported. This is because key national targets around smoking are based on current daily smoking [41, 42]. The vast majority of current smokers do smoke daily, and daily smoking is associated with the strongest negative impacts, compared with less frequent smoking.
In the 2018–19 NATSIHS, the prevalence of current daily smoking among Aboriginal and Torres Strait Islander adults (aged ≥18 years) was 40.2%, and the prevalence of current or less-than-daily smoking was 3.2%. This combines to a total adult current smoking prevalence of 43.4% [2]. Current smoking (daily and less-than-daily combined) prevalence was 39.3% among those aged 18–24, 47.5% among those aged 25–34, 49.8% among those aged 35–44, 44.9% among those aged 45–54, and 35.6% among those aged ≥55 years. Prevalence was similar for males (45.6%) and females (41.2%). Prevalence was lower among those in non-remote settings (39.6%) compared with those living in remote areas (59.3%) [2].
There has been a significant and substantial decrease in adult current smoking prevalence since 1994. Overall, current adult (aged ≥18 years) smoking prevalence decreased by 11.1 percentage points, from 54.5% in 1994 to 43.4% in 2018–2019 [2, 43]. There was relatively minimal change in smoking prevalence between 1994 and 2004–05 [3]. However, there have been recent substantial decreases in smoking prevalence. From the period of 2004–05 to 2018–19, daily smoking prevalence decreased by 9.8 percentage points (95% Confidence Interval: 6.7 to 11.5 percentage point decrease) among adults aged ≥18 years, from 50.0% to 40.2% [2, 44].
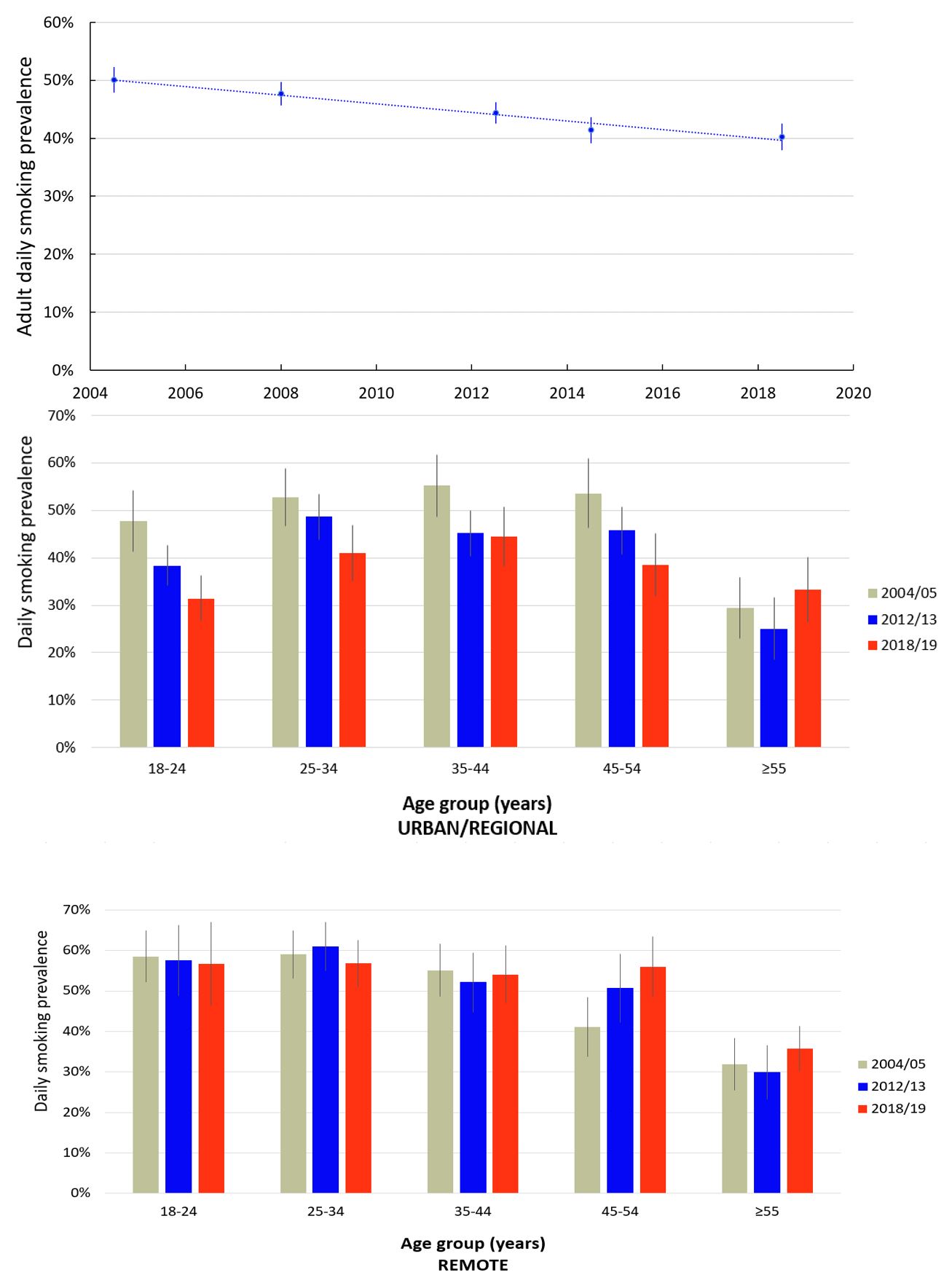
Substantial decreases in daily smoking prevalence from 2004–05 to 2018–19 were observed in younger age groups, with a 14.7% decrease for those aged 18–24 years, 10.6% for those aged 25–34, 8.5% for those aged 35–44 years and 8.7% decrease for those aged 45-54 years [2, 44]. No significant change was observed among people aged ≥55 years.
From 2004-05 to 2018-19, there was a 12.0 percentage point decrease (95% CI: 8.0,14.0) in daily smoking prevalence in non-remote settings. There was no significant change observed for those living in remote areas (0.1% increase, 95% CI: -5.2, 2.5) [44]. Research is needed to understand what underlies reductions in smoking prevalence in non-remote settings, and what is required to support declines in smoking prevalence in remote areas (Figure 1).
Figure 1: Estimated prevalence of daily smoking among Aboriginal and Torres Strait Islander adults by age and remoteness group, 2004–5 to 2018–19
Source: Maddox et al. (2020 in progress) [44] and ABS (2019) [2].
Smoking initiation
There is evidence that young adults are initiating smoking later. Analysis of data from the 2014–15 National Aboriginal and Torres Strait Islander Social Survey (NATSISS) and the 2004–05 NATSIHS found a decrease in the percentage of 18–24 year olds who smoked began smoking daily before the age of 18 (from 84% in 2004–05 to 76% in 2014–15) [45].
Smoking during pregnancy
There has been a substantial decline in smoking during pregnancy among Aboriginal and Torres Strait Islander women. It is estimated that 44% of Aboriginal and/or Torres Strait Islander mothers who gave birth in 2017 smoked during their pregnancy [46]. While this rate is high, there has been a substantial decline of 8 percentage points compared to 2009 rates of 52%. Smoking during pregnancy was less prevalent in major cities (38%) compared with remote (48%) and very remote (55%) areas. Aboriginal and Torres Strait Islander women are motivated to quit smoking during pregnancy and are making quit attempts (see Factors related to quitting for more information) [47, 48].
Second-hand smoke
Second-hand smoke releases thousands of chemicals into the environment [17]. Many Aboriginal and Torres Strait Islander peoples live in homes with people who smoke. In the 2014–15 NATSISS, it was reported that 57% of children aged 0–14 years, and 60% aged 15 years and over, lived in a household with someone who smoked [49]. While many people smoke outdoors to limit the impact of their smoking on others, the 2014–15 NATSISS found that some people live with someone who smokes inside. The survey found that 13% of children and 19% of people over 15 years of age lived in home where people smoke inside.
Research has shown that Aboriginal and Torres Strait Islander people are making changes in smoking behaviour to reduce the impact of second-hand smoke on other people, particularly children [50-52]. In the Talking about the Smokes (TATS) study, 53% of daily smokers reported that smoking was not permitted inside their home [53]. In a qualitative study in NSW, parents expressed strong ideas about protecting their children from second-hand smoke including: stopping other people smoking in their homes, avoiding social situations where people would be smoking, smoking outside and changing clothes after smoking [50].
Chewing native tobacco
In some parts of Australia, largely in Qld, the NT and WA, Aboriginal and Torres Strait Islander people use, and have historically used native plants containing nicotine. Bush tobacco (Nicotiana spp.) is prepared by drying the leaves, mixing them with ash to make nicotine available, and chewing to form a ‘quid’. Quids are then either held in the mouth or stored on the body – often behind the ear – where the nicotine is absorbed through the skin [20-22]. Bush tobaccos contain roughly 1% nicotine [27]. They were historically widely prepared, were used by men, women and children, and continue to be used and traded today [28].
Pituri, (D. hopwoodii) is another form of native tobacco which is prepared and used similarly to bush tobacco. It is a powerful stimulant, containing up to 8% nicotine. Pituri was a valued commodity and its production, distribution and consumption was constrained by social control mechanisms. Knowledge of processing pituri was vested in older males of particular groups in South Western Qld, where most of Australia’s pituri was processed, but it was traded widely [27, 28]. Use of pituri declined as the methods of preparation were lost during the period of early colonisation [28]. While a range of names exist for chewing native tobacco, in some places, the term ‘pituri’ has come to describe all chewing tobacco plants [21, 27, 28].
Chewing tobaccos were (and are) used to enhance mood, to suppress appetite, to reduce stress and pain, and to facilitate and maintain relationships through sharing [20, 21, 27, 28].
There is limited research on contemporary use of chewing tobacco, though its use is understood to be high in some regions of Australia [20]. For example, in Central Australia, high levels of chewing tobacco use were reported particularly among women, with young girls starting to use it between the ages of five and seven years [21]. A study in the Kimberley region of WA found that 39% of participants reported current use of chewing tobacco [54]. This was higher than commercial tobacco use at 35%.
E-cigarettes
There is limited research on the prevalence of e-cigarette use within the Aboriginal and Torres Strait Islander population. Analysis of the TATS study found that one in five (21%) Aboriginal and Torres Strait Islander participants had tried e-cigarettes, compared with 31% of the national population [55, 56]. This may be attributable to relatively low awareness of e-cigarettes, with 38% of Aboriginal and Torres Strait Islander participants reporting to have never heard about e-cigarettes [55]. E-cigarette usage was collected in the NATSIHS for the first time in 2018–19, however, prevalence estimates have not yet been published from these data.
Some studies have looked into the effectiveness of using e-cigarettes as a cessation tool, however the quality of the evidence is low [57, 58]. Further, there is evidence that e-cigarettes are harmful to health and may be linked with future smoking behaviour (see below for more information). As such, many health organisations state that there is insufficient evidence to support use of e-cigarettes as a cessation tool [59, 60].
How smoking affects your body and health
Exposure to the products of tobacco combustion and nicotine from past and current smoking, second-hand and third-hand smoke, and exposure in-utero has detrimental effects across the lifespan. Smoking harms almost every organ and body system. However, quitting smoking has immediate and long-term benefits, regardless of how long a person has been smoking [40].
This section summarises the health effects of tobacco use however, the information on the breadth and magnitude of the effects of smoking on specific health conditions is drawn from studies of non‑Indigenous populations, as the evidence from Aboriginal and Torres Strait Islander populations is sparse. Appendix 2 summarises key evidence from studies with Aboriginal and Torres Strait Islander populations. For more detailed information on the health effects of smoking, see Tobacco in Australia [19], and the US Surgeon General’s report The Health Consequences of Smoking—50 years of Progress [40].
Tobacco use and common chronic conditions
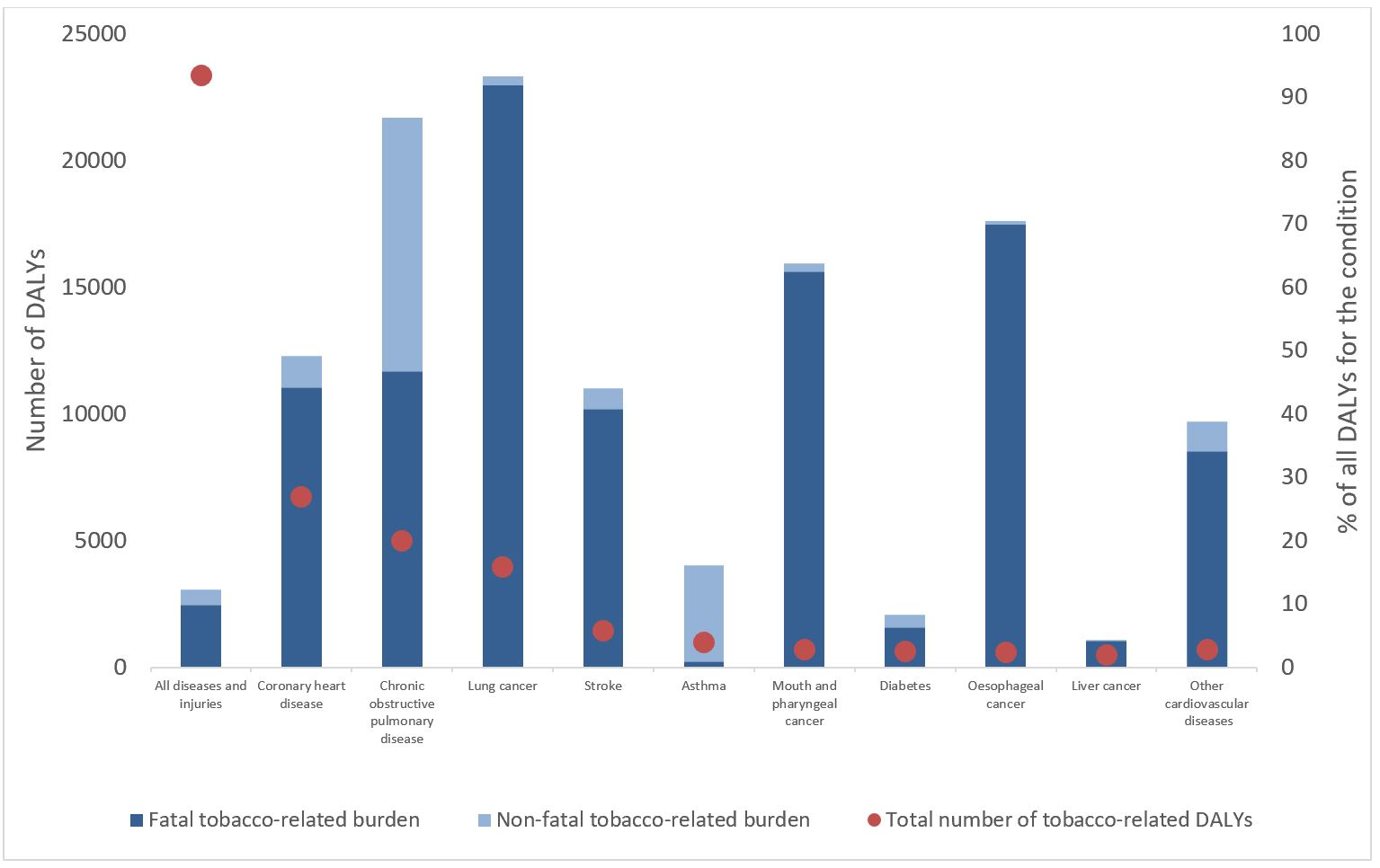
The highest burden of disease from smoking is from atherosclerotic diseases (mainly coronary heart disease (CHD)), cancers, chronic lung disease, and type 2 diabetes (Figure 2) [61]. Smoking is causally linked to a wide range of health conditions, including rheumatoid arthritis, tooth and gum disease, pneumonia and hip fractures [40]. The mechanisms by which smoking causes these chronic diseases are summarised below.
Atherosclerotic diseases: coronary heart disease (CHD), cerebrovascular disease and peripheral arterial disease (PAD)
Large international cohort studies, including the Framingham Study, first established the association between smoking and coronary health disease (CHD, also known as ischaemic heart disease), myocardial infarction (MI, heart attack) and mortality in the 1960s [62]. Further studies have identified how smoking contributes to the development of atherosclerosis, the process that underlies development of CHD, most cerebrovascular disease and peripheral arterial disease (PAD). Atherosclerosis results from damage to the lining (endothelium) of arteries, progression to a chronic inflammatory state, and development of fatty endothelial plaques [40]. Over time, these plaques develop a fibrous cap and, together with the formation of blood clots (thrombosis), can lead to local arterial narrowing. Arterial blockage from ruptured plaques and thromboembolism can cause acute cardiovascular events such as MI and stroke.
Cancer
At least 69 of the more than 7,000 chemicals in tobacco smoke are carcinogens (cancer-causing substances) [40]. The body attempts to detoxify these carcinogens via enzymes, which can lead to metabolic activation of reactive compounds that can alter sections of DNA [63]. If not repaired, this altered DNA can result in cell mutations. Combined with carcinogen-related inactivation of tumour‑suppressor genes and receptor-mediated survival of damaged epithelial cells, these mutations lead to the abnormal and uncontrolled cell growth characterised by cancer. The causal relationships between tobacco smoke and many cancers – including lung, head and neck, pancreatic, liver and colorectal cancers – are well established [40]. Smokers with all types of cancer are at increased risk of death compared with non‑smokers [40, 63].
Chronic obstructive pulmonary diseases
Chronic obstructive pulmonary disease (COPD) – which includes emphysema, chronic bronchitis and chronic asthma – is characterised by chronic irreversible airflow obstruction. The body mounts an immune response to the prolonged irritation and oxidative stress from tobacco smoke that, over time, can lead to permanent changes to the lungs, including widening of the air sacs, excessive mucous secretion, and stiffening of the smaller airways [40].
Type 2 diabetes and diabetes complications
Cigarette smoking can cause diabetes and the risk of disease increases with intensity of smoking [40]. In particular, nicotine contributes to the development of pre-diabetes, type 2 diabetes and the vascular complications of diabetes through three mechanisms:
- decreased sensitivity of body cells to the action of insulin, leading to higher blood glucose levels
- reduced insulin production from pancreatic beta cells, and
- loss of beta cells from prenatal and neonatal exposure to nicotine [64].
Smoking affects the development of the macro-vascular complications of diabetes (atherosclerotic diseases), which are the leading cause of mortality for people with diabetes [65]. However, evidence is limited for the relationship between smoking and the microvascular complications of diabetes: kidney disease (nephropathy), eye disease (retinopathy) and nerve damage (neuropathy).
Evidence indicates that people who already have diabetes who quit smoking:
- reduce their risk of death by around two-thirds
- reduce their risk of cardiovascular disease by over 80%, and
- reduce the risk of stroke to the same as for never-smokers [66].
Smoking in pregnancy
The negative effects of smoking on reproductive health are extensive. The US Surgeon General’s 2014 report summarises that ‘smoking affects the likelihood of pregnancy, the outcome of pregnancy, and the future health of the child’ [40, p.498].
Maternal smoking during pregnancy (and to a lesser extent, exposure of the mother to second-hand smoke) is associated with increased risk of a range of poor birth outcomes, and health effects on the child in infancy and later life [67-71]. These effects may occur through a range of mechanisms, including reduced oxygen delivery to the foetus, imbalances in essential nutrients, DNA changes, and the direct toxic effects of nicotine exposure [63]. Maternal smoking increases the risk of:
- ectopic pregnancy [72]
- spontaneous abortion (miscarriage) [63]
- foetal growth restriction [73]
- preterm delivery [72]
- stillbirth and perinatal mortality, and [74, 75]
- cleft lip and/or palate [76].
A large study of babies born to Aboriginal mothers in NSW found that not smoking in pregnancy reduced the risk of having a baby that was small for gestational age by 65%, and reduced the risk of both perinatal death and preterm birth by 42% [77]. The increased risk of stillbirth and perinatal mortality from maternal smoking probably arise via placenta praevia and placental abruption, preterm delivery, premature and prolonged rupture of the membranes [40].
Maternal smoking during pregnancy is a significant risk factor for Sudden Infant Death Syndrome (SIDS) and Sudden Unexpected Death of the Infant (SUDI), via both a direct mechanism and the associated increased risk of pre-term birth and low birthweight [78].
Evidence also exists for links between maternal smoking and later-life outcomes for the child, including Attention Deficit Hyperactivity Disorder [71], obesity [68], asthma under the age of two years [70], and diabetes after age 16 years [69].
Second-hand smoke
Exposure to second-hand smoke is associated with increased risk of a range of conditions, including COPD, CHD, lung cancer, and stroke [40, 70, 79]. Children exposed to second‑hand smoke are at increased risk of invasive meningococcal disease, middle ear disease, lower respiratory infections and asthma [70, 80, 81].
Evidence suggests that people exposed to second-hand smoke are more likely to start smoking, more likely to have a heavier dependence on nicotine, and are less likely to initiate and sustain quit attempts [82].
Third-hand smoke
Third-hand smoke (THS) consists of the nicotine and combustion products of second-hand smoke that persist on dust and surfaces including carpets, blankets, clothes and skin. These can react with other chemicals in the environment to form new toxins – which can take months to years to disintegrate – and can be repeatedly re-suspended, or re-emitted in gaseous form, into the air [83]. Compounds of THS can be inhaled, absorbed through the skin, or ingested, and children are most susceptible to exposure. The health effects of THS have not yet been quantified, but may include harms to the liver, lungs and skin, and behavioural changes [84].
Chewing tobacco and e-cigarettes
Smokeless tobacco products, like chewing tobacco and e-cigarettes, are thought to be less harmful to health than smoking, yet many still contain harmful carcinogens and nicotine similar to commercial tobacco [85]. While the evidence is sparse in Australia for these forms of tobacco use, there is international evidence that chewing tobacco and e-cigarette use are harmful to health.
There is evidence from other populations that chewing tobacco is linked to increased risk of death from all causes, and specifically linked to death from cancers (tongue, lip, gum, cheek, throat, oesophagus and pancreas), and cardiovascular disease [86]. Using chewing tobacco while pregnant is linked to poor birth outcomes (preterm birth, low birth weight, still birth, neonatal nicotine addiction and withdrawal syndrome) [87-89]. As chewing tobacco research has been conducted largely in international settings with different plants, people and contexts of use, these findings may not be generalisable to Aboriginal and Torres Strait Islander peoples’ use of chewing tobacco [20, 90].
There is international evidence too about the health harms of e-cigarettes. While they are often marketed as being less harmful than smoking cigarettes, there are increasing concerns globally about their health impacts [91]. E-cigarettes have been found to have direct health harms, including increased risk of respiratory disease, cardiovascular disease and carcinogenesis [59, 92]. Further, there is growing evidence that e-cigarette use can be a precursor to smoking (both in young people and in previously non‑smoking adults) [23, 93, 94]. The Cancer Council Australia have issued a statement that, based on the current evidence, the harms of e-cigarettes outweigh the potential benefits [59].
There have also been almost 3,000 cases of lung injuries from e-cigarette use in the United States, leading to hospitalisations and 68 deaths as of February 2020 [95]. While evidence is not yet sufficient to rule out other chemicals of concern, vitamin E acetate has been strongly linked to the outbreak and tetrahydrocannabinol (THC) has also been linked to most cases. The number of new cases of lung injury was declining in early 2020.
Tobacco-related disease burden
The burden of disease is the combined impact of living with and dying from diseases, health conditions and injuries. The burden can be measured in years of ‘healthy’ life lost due to ill health, disability and premature death, using Disability-Adjusted Life Years (DALYs) [96]. One DALY can be interpreted as one year of healthy life lost. Adding these DALYs up for a population estimates the total burden of disease. It also gives an indication of the gap between the current health situation and an ideal situation where the whole population lives a long life, free of disease and disability.
In 2011, more than 12% of all disease burden in the Aboriginal and Torres Strait Islander population was attributed to tobacco use (equivalent to >23,000 DALYs or 23,000 years of healthy life lost) (Figure 2) [61]. This includes the contribution of past and current tobacco use, and exposure to second-hand smoke in the home, but it does not include exposure to smoking in-utero. Most of the total tobacco-related burden was due to CHD (6,747 DALYs); tobacco explains 49% of the total burden of CHD. Tobacco contributes to the majority of the lung cancer (93%) and COPD burden (87%) in the population, but these conditions contribute to fewer DALYs (3,970 and 4,993, respectively) because they are less common in the population.
Lung cancer accounted for 2.4% and 2.2% of total DALYs among Aboriginal and Torres Strait Islander males and females, respectively [61]. Results from a 15 year follow-up study with 2,273 Aboriginal and Torres Strait Islander adults from remote Far North Qld found a four-fold increase in lung cancers among smokers compared to non-smokers. No participants had cancer at the beginning of this study [97].
The most recent analysis of tobacco-related hospitalisation data from 2007 to 2009 showed that 3.3 hospitalisations per 1,000 in the population were for a tobacco-related diagnosis [98].
Figure 2: Burden of disease attributable to tobacco use as number and percentage of DALYs, by disease, Aboriginal and Torres Strait Islander peoples, 2011
Note: The proportion of DALYs attributable to tobacco use has been further divided into fatal and non-fatal burden
Source: AIHW (2016) [61]
Tobacco-related mortality
The 2011 Burden of Disease Study did not estimate the contribution of smoking to deaths in the population [61]. In the 2003 Burden of Disease Study, it was estimated that 20.0% of all deaths were attributed to smoking [99]. A report on the social costs of tobacco in Australia in 2015/16 estimated that at least 886 Aboriginal and Torres Strait Islander premature deaths are caused by smoking each year [100]. This estimate includes 491 male deaths and 395 female deaths, 82 deaths at age 25-44 years, 441 deaths at age 45-64 years, and 361 deaths at age 65 years and over. Earlier studies, from the 1990s, indirectly estimated the proportion of all Aboriginal and Torres Strait Islander deaths caused by smoking [101, 102], and the potential gains in life expectancy if tobacco-related deaths were avoided [103], using the aetiologic fractions method. All of these estimates of smoking-attributable mortality are based on indirect methods, incorporating evidence from other populations. There is a need for evidence specific to Aboriginal and Torres Strait Islander peoples on the relationship between smoking and mortality, and the contribution of smoking to deaths at the national level; this work is underway [104].
Impact on community and culture
Given that tobacco use is the biggest contributor to burden of disease and mortality among Aboriginal and Torres Strait Islander smokers, it has a great impact on the community. The burden of grief that comes with the loss of older generations can have significant impacts on families and communities [105]. Wiradjuri woman, Jenny Munro, speaking about high mortality rates in Aboriginal and Torres Strait Islander communities shared:
You get to a point where you can’t take any more and many of our people withdraw from interacting with other members of their community because it’s too heartbreaking to watch the deaths that are happening now in such large numbers… In 227 years we have gone from the healthiest people on the planet to the sickest people on the planet. [106, paragraph 35]
Premature deaths of community members, including Elders and older community members prevents the transmission of generational knowledge, kinship, language, customs and law which are interconnected components of Aboriginal and Torres Strait Islander culture [107-109].
Factors related to tobacco use among Aboriginal and Torres Strait Islander peoples
Tobacco use is a complex behaviour, shaped by a range of historical, cultural, community, family and personal factors. It is important to understand the multi-layered factors that have led to high prevalence of tobacco use among Aboriginal and Torres Strait Islander peoples. Unless explicitly stated, literature and evidence presented in this section is specific to the Aboriginal and/or Torres Strait Islander population.
Tobacco industry
The tobacco industry is responsible for the harms caused by tobacco. In Australia, almost all cigarettes are from three transnational tobacco companies Philip Morris International (PMI), British America Tobacco (BAT), and Imperial Tobacco [110]. Australia no longer grows commercial tobacco or manufactures tobacco products. An estimated 14,062 million cigarettes were sold in Australia in 2017, excluding roll‑your-own tobacco [111]. In January 2019, there were 60 brands and sub‑brands of factory-made cigarettes, including 327 unique variant and pack size combinations on the Australian market [110]. The tobacco industry promotes tobacco sales and consumption and interferes with and opposes tobacco control policies and activities to reduce tobacco use in Australia. The tobacco industry has:
- exploited and appropriated Indigenous names and imagery [32]. Winfield used an image of an Aboriginal man playing the digeridoo to market their cigarettes overseas as ‘Australians’ answer to the peace pipe’ [112, 113]
- targeted Aboriginal and Torres Strait Islander communities through advertising. For example, one brand attempted to promote good will through providing funding from the sales of their cigarettes to buy jerseys for local sports teams [27, 112]
- monitored tobacco control research and activities in Aboriginal and Torres Strait Islander communities [113]
- obstructed the implementation of public health measures [114], including funding organisations to mislead and distract the public, as well as opposing tobacco control legislation and the FCTC [110], and
- advanced misinformation about the harms of tobacco use [110, 114].
Recently, the tobacco industry has purported to ‘rebrand’ themselves as helping to reduce the harms caused by tobacco use [110]. For example, PMI has sent letters to Aboriginal organisations promoting its e-cigarettes as a tobacco control measure [115]. PMI also provided US$1 billion in funding to establish the Foundation for a Smoke-Free World [116]. The Foundation’s mission is to ‘end smoking in this generation’, and has specifically targeted Indigenous peoples with its funding of the Centre of Research Excellence: Indigenous Sovereignty & Smoking in Auckland [32, 116]. BAT has also stated that its work aligns with the United Nations Strategic Development Goals in an attempt to establish its corporate social responsibility [110, 117]. Despite these attempts at changing their public-facing agenda, to be genuinely socially responsible, the tobacco industry would have to cease the sale of tobacco and their opposition to tobacco control [32, 110, 114, 118].
There is a proud history of examples of Aboriginal and Torres Strait peoples and organisations resisting offensive tobacco industry marketing of its products, and many Indigenous leaders have opposed this latest tobacco industry initiative [32, 113].
Governments, health services and individuals need to understand how tobacco industry tactics are used to undermine public health efforts. The Australian Government has a responsibility as a signatory to the FCTC to protect public health policies from the vested interests of the tobacco industry [11]. The misinformation, promotion and targeted advertising can erode self-determination.
Ongoing impacts of colonisation
As noted earlier, colonial processes have directly led to tobacco use and addiction among Aboriginal and Torres Strait Islander peoples [27, 28, 30, 36]. In addition to these direct pathways, there are profound ongoing impacts of colonisation and subsequent government policies that contribute to the use of tobacco today. For example, colonial processes have contributed – and continue to contribute to – Aboriginal and Torres Strait Islander peoples disproportionately experiencing barriers to employment, poverty, higher disease burden, intergenerational trauma, discrimination [7]. These factors, in turn, are associated with smoking and/or are barriers to quitting [31]. Given the complex negative impact colonisation has had on Aboriginal and Torres Strait Islander peoples’ health through generations, colonisation is considered a social determinant of health for Indigenous peoples [6, 119, 120]. However, there is a dearth of studies that specifically explore the impacts of colonisation on tobacco use [121]. The available evidence is outlined below.
Trauma
Colonialism and subsequent government policies have caused extensive and ongoing trauma [7]. Many Aboriginal and Torres Strait Islander peoples have been removed from their lands, their families and culture [31]. These processes occurred historically, but also continue today, such as through contemporary child removal and incarceration. The trauma from these experiences impacts health and other outcomes across generations [120, 122]. Trauma is linked to a range of outcomes, including substance use and poorer social and emotional wellbeing, which, in turn, are associated with higher tobacco use [31, 123].
Stolen generations and contemporary removal of children from families
The removal of children from their families is linked with smoking. The evidence shows that:
- people removed from their families during the Stolen Generations were more likely to be a current smoker (50%) than those who were not removed (40%) [122], and
- contemporary removal of children also increases the likelihood of smoking. Those aged 15 to 39 years who were removed from their family were more likely to be current daily smokers (66%) than those who were not removed (45%) [124].
Social and emotional wellbeing
The evidence shows that Aboriginal and Torres Strait Islander peoples experience a disproportionate burden of poor mental health and/or poor social and emotional wellbeing [125]. Social and emotional wellbeing is linked to tobacco use.
- Analysis from baseline data (collected 2006–08) of a longitudinal study of Aboriginal adults aged 45 years and over in NSW found that the risk of smoking was significantly lower among those with low or moderate levels of psychological distress compared to those with high or very high distress [126].
- Analysis of the 2014–15 NATSISS found that people with a mental health condition were more likely to be a daily smoker (46%), compared with those without a mental health condition (33%) [127].
- Having a mental health condition can be a reason people continue to smoke. Young people have reported smoking to cope with their depression [128].
- Having a mental health condition can make it harder to quit. Those with mental health conditions have lower levels of access to quit services. Further, though they make similar numbers of quit attempts to those without a mental health condition, they are less likely to maintain a quit attempt [129].
Exposure to racism
Colonialism and government policies have embedded racism within systems (structural racism) and within individuals (interpersonal and internalised racism). As a result, many Aboriginal and Torres Strait Islander peoples have commonly experienced both kinds of racism [49, 130]. Much less is known about internalised racism and how it links to health and health behaviours. However, it is well established that experiences of racism lead to negative health and wellbeing outcomes for Aboriginal and Torres Strait Islander peoples [130, 131].
Racism has been linked with smoking behaviour [123, 125, 130, 132].
- Racism, stereotyping and stigma from media and government interventions contribute to stress that people then attempt to ameliorate by smoking [123].
- Racism has also been linked to early experimentation with tobacco. Analysis of data from the Footprints in Time: The Longitudinal Study of Indigenous Children (LSIC) dataset found that young people (10–12 years) were seven times more likely to have tried smoking if they had experienced racism between the ages of 4 and 11 years, compared with those who had not experienced racism [131].
- The TATS study found that people who said they had been treated unfairly in the past year because they were Aboriginal or Torres Strait Islander were less likely to have made a quit attempt in the past year or have ever made a quit attempt; however, these smokers who had reported racism in the previous year were no more or less likely to quit or sustain a quit attempt in the subsequent year [133, 134].
Exclusion from economic structures
Aboriginal and Torres Strait Islander peoples are significantly more likely than non-Indigenous Australians to be excluded from economic opportunity. This is evidenced by lower incomes, higher levels of unstable housing and/or higher levels of unstable employment, and lower levels of formal education [125]. Conversely, relative advantage across these social determinant indicators is linked to non-smoking among Aboriginal and Torres Strait Islander adults [122, 126, 135, 136].
- A study in 2015 in the ACT found that people who completed Year 12 were more than 21 times more likely to be non-smokers than those who did not [137].
- Analysis of the TATS study data found that positive changes in socio-economic factors, such as getting a job or buying a home, have also been associated with sustaining smoking abstinence. However, baseline measures of socio-economic advantage were not significantly associated with starting or sustaining a quit attempt in the next year [138].
- A qualitative study in Qld found that narratives of empowerment and a greater sense of control contribute to sustained cessation [139].
It is important to highlight that many people who do experience socio-economic disadvantage are able to quit smoking or stay never-smokers. Socio-economic disadvantage need not be seen as an insurmountable obstacle to quitting, but there remain many other reasons to address these socio‑economic factors [138].
Incarceration
Aboriginal and Torres Strait Islander peoples are severely over-represented in prisons, making up 28% of the adult prison population and 59% of in youth detention in 2018 [140, 141].
The evidence shows that people who have been incarcerated, detained, or arrested are more likely to be smokers.
- In 2018, 80% of Aboriginal and Torres Strait Islander peoples who entered prison reported that they were current smokers at the time they entered [142].
- In 2015, 90% of young Aboriginal and Torres Strait Islander people in detention in NSW had smoked, and 81% were daily smokers prior to being placed in detention [143].
- Those who had not been arrested or incarcerated within the last five years were, respectively, 4.5 and 4 times more likely to be non-smokers than those who had been arrested or incarcerated [135].
Though smoking is banned in prisons in all states and territories except WA [125], many people who have been incarcerated resume smoking when they leave prison [142].
Substance use
The evidence shows that both alcohol and cannabis use is linked with tobacco use.
- Not consuming alcohol is linked to lower likelihood of smoking. Analysis of the 2002 NATSISS data found that people who had not consumed alcohol in the last 12 months were significantly more likely to be a non-smoker compared to those who had consumed alcohol [135].
- Increased or risky alcohol intake is associated with higher likelihood of smoking.
- A study of older adults in NSW from 2006–08 found that people who consumed no, or low levels of alcohol (1–14 standard drinks per week) were significantly less likely to smoke than people who drank more than 14 standard drinks a week [126].
- Analysis of the 2008 NATSISS found that people who reported risky (short and long term) drinking, chronic alcohol consumption were more likely to be current daily smokers than people who drank at low-risk levels [144, 145].
- Risky drinking impacts quitting. Analysis of the TATS study data found that people who report risky drinking were less likely to want to quit [146] and less likely to make a quit attempt [147] than those who did not.
- The use of cannabis has also been linked with tobacco use; however, the direction of the association is not clear.
- Analysis of 2008 NATSISS data found that current daily smokers were more likely to have used illicit substances such as cannabis, than those who have never smoked [144, 145].
- An analysis of the 2012–13 NATSIHS and the TATS study data found that cannabis use was common (32% and 24% respectively) among Aboriginal and Torres Strait Islander smokers [148].
- In the NATSIHS, smokers were almost five times as likely to have used cannabis in the last 12 months than non-smokers [148].
- Further, in the TATS study, 24% of smokers, smoked something other than tobacco (e.g. cannabis), and that 92% of these people reported mixing tobacco and cannabis together to smoke [148].
Using one substance (tobacco, cannabis or alcohol) significantly increased the likelihood of using the other substances. A survey of substance use with Aboriginal and Torres Strait Islander women during pregnancy found that among women reporting current substance use, 56% reported using one substance only and 44% reported using two or three [149].
Stress
On average, Aboriginal and Torres Strait Islander peoples experience high levels of stress, resulting from colonisation and its ongoing impacts [7]. Evidence indicates that stress is related to smoking [49, 135, 150, 151]. Moreover, experiencing multiple life stressors (such as a serious illness, death of a family member, violence, relationship problems) is associated with increased levels of smoking compared to experiencing no life stressors [135].
Aboriginal and Torres Strait Islander peoples report that a key reason for starting and continuing smoking is for stress management [31, 50, 123, 139, 152]. Smoking has been described as a way of taking a moment to oneself to relax and de-stress [35]. However, much of the stress relief from smoking may be because smoking another cigarette relieves the symptoms of nicotine withdrawal [129].
Smoking’s role in stress management means that high levels of stress can be a barrier to quitting and maintaining quit attempts [151]. Indeed, stress arising from life crises, such as a death in the family, have been reported as causing increased smoking intensity and relapse after a quit attempt [35, 153, 154].
However, the TATS study has shown that higher baseline stress predicted quitting smoking and maintaining a quit attempt for at least a month [147]. Particular forms of stress – such as stress about the health impacts of smoking, financial stress caused by spending on tobacco, and stress related to the stigma of smoking – may actually support people to quit smoking [139, 147, 155]. It may be that stress can motivate people to improve both their health and their financial situation through quitting smoking. This is important because, while we know stress is a key reason for why people do smoke, it may not be an insurmountable barrier to quitting.
Financial stress
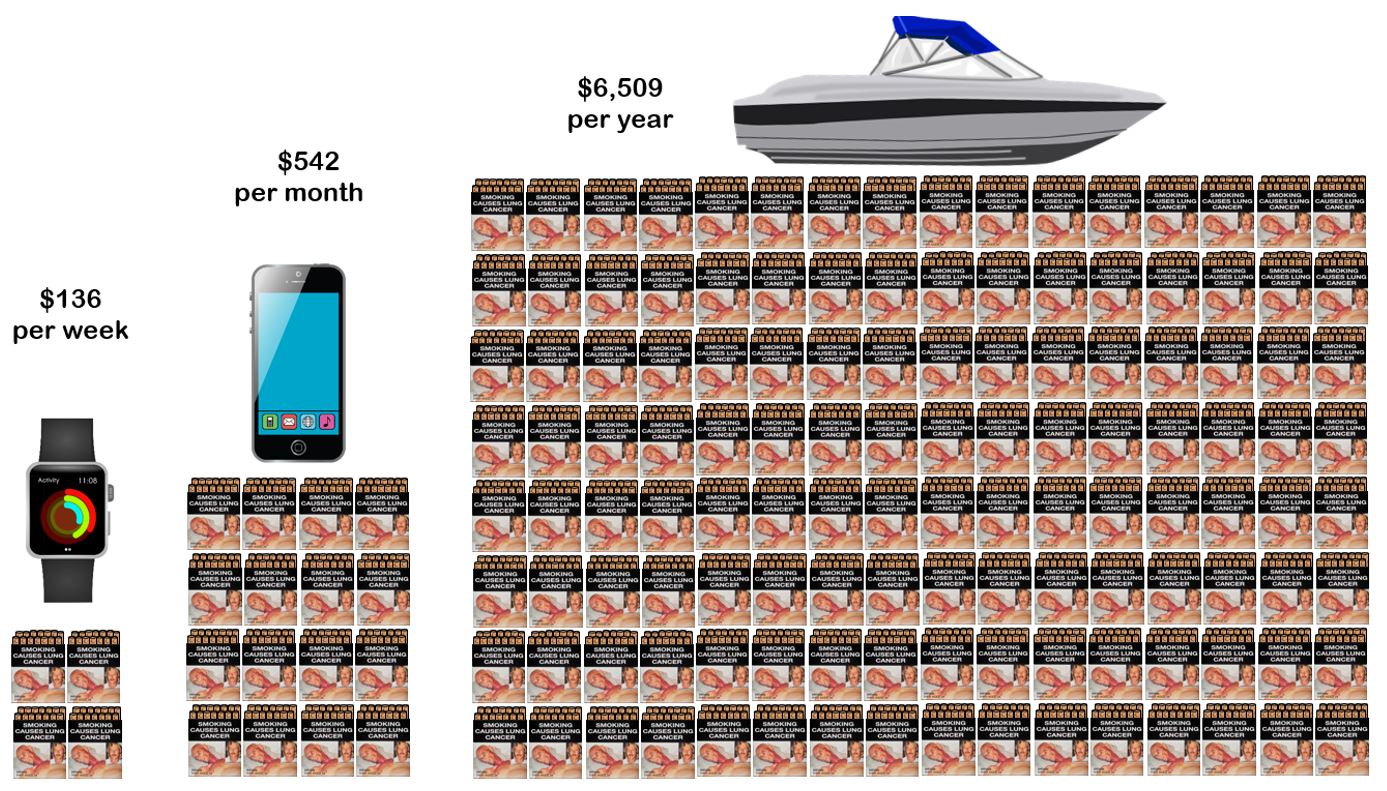
Financial strain is one form of stress that is closely linked with smoking. People may use smoking as a mechanism to cope with financial strain; however, the cost of smoking, in turn, can increase financial strain. Smoking can be expensive. In 2019, the average price of a 25 packet of cigarettes was $33.90 [156]. According to the National Drug Strategy Household Survey 2016, the mean number of cigarettes smoked per week by Aboriginal and Torres Strait Islander people 18 years and over who smoke was 95.8 or approximately four packs (based on a 24 pack of cigarettes) [157]. Therefore, the average Aboriginal and Torres Strait Islander adult who smokes will spend $136 per week, $542 per month or $6,509 per year on cigarettes [56]. Figure 3 shows an example of what the money could be spent on if someone were to quit smoking.
Figure 3: Money saved if an average smoker quit smoking, 2017
Source: Derived from AIHW data (2017) [56]
Normalisation of smoking
Due to high prevalence, some communities and families see tobacco use as the norm [108]. Perceived norms around smoking can be an important factor influencing tobacco use attitudes and behaviours [31, 158]. For example:
- viewing adults smoking in the household or community can lead young people to see smoking as a normal part of being an adult [128].
- smoking behaviour among family and friends can be influential in smoking initiation for young Aboriginal and Torres Strait Islander people [152]. A 2015 study in the ACT found that the likelihood of smoking increases as the proportion of people in a household who smoke increases [137].
- smoking behaviour of friendship groups also plays a large role in young people beginning to smoke [31].
- youth are less likely to smoke if they perceive it as socially unacceptable, and if family and friends do not smoke [152].
Studies have demonstrated that in contexts where smoking is normalised, smoking can have positive impacts on social relationships. Tobacco use has been found to:
- be an effective mechanism to maintain and strengthen kinship and social relationships, and promote belonging and social cohesion [159], and
- provide a sense of community, belonging and connection [160].
Social role of smoking
Smoking can play a social function, potentially fostering an environment that can lead to the continuation of smoking and acting as a barrier to quitting [152, 161]. Smoking and sharing cigarettes have been viewed as ways of maintaining and strengthening relationships by Aboriginal youth in urban NT [162]. The maintenance of relationships is a high priority in many Aboriginal and Torres Strait Islander cultures, often given precedence over individual wishes [31]. In this context, obligations to share resources, and to provide and receive gifts is a vital part of social life [14]. Gifts of tobacco have been described as a key way of partaking in reciprocal exchange, an expected part of relationships, and a way of showing care, love and respect [14, 21, 31].
For example, Aboriginal Health Workers (AHWs) in South Australia (SA) reported that smoking provides an opportunity to socialise with co-workers and facilitates relationships with community members [35]. Other people have reported smoking to gain entry into a particular social group, or as a way of having important conversations with peers who smoke [152]. Smoking can also provide a source of identity, status and a sense of belonging to a certain group [31, 35].
Factors in the initiation of tobacco use
Initiation occurs most commonly when people are young (see Smoking initiation for more information) [43].
It is important to note that initiating smoking, or indeed choosing not to smoke, is not a one-off event but rather a complex pattern of behaviour that varies from person-to-person [163]. For some people, initiation occurs in stages, for example: first try and experimentation, social or casual smoking and then established smoking [162]. Though, not all people who experiment or socially smoke will become established smokers.
The influence of family and friends is a major factor in the initiation of smoking by young Aboriginal and Torres Strait Islander peoples [121, 162]. Specifically, family and friends who smoke increase the accessibility of tobacco products, and social desirability of smoking and influence the normative attitudes towards tobacco use.
- Young people have reported sourcing their first cigarettes from family members (with and without permission or approval) [162].
- Young people have also reported that progression to social and established smoking was influenced by smoking behaviours in their broader social networks [162].
- Almost 60% of people from a 2015 study in the ACT reported that a friend or acquaintance gave them their first cigarette [137].
- Smoking is also reported as a behaviour people do to gain ‘cool’ status, to seem older, to assert their membership to the group and to live their Aboriginal identities. This internalisation of smoking as a way of being Aboriginal may have resulted from the high prevalence of smoking in these rural coastal communities. For them, smoking was a way to be like others, socialise and belong to a group [31].
The large role that the smoking behaviour of others plays in an individual’s initiation of smoking highlights the importance of addressing smoking behaviour at the community level, as well as working with young people to not start smoking [121].
Quitting
Evidence shows that smokers want to quit [133, 164]. The TATS study found that 70% of people who smoke daily want to quit, 69% of people who smoke daily had ever made a quit attempt, and 48% had made a quit attempt in the past year [164]. However, it also found that only 30% of people who tried to quit in the past year sustained the quit attempt for longer than one month [133].
Evidence also shows that quit attempts are increasing. The percentage of people who smoke who attempted to quit increased from 45% in 2008 to 50% in 2014–15 [43]. Females were more likely to attempt to quit compared to males (54% compared to 47%) and those living in remote areas were more likely to attempt compared to non-remote daily smokers (58% compared to 48%).
Successful quit attempts are also increasing. In 2014–15, 36% of adults who had ever smoked had a successful quit attempt [43]. This is an increase of 12 percentage points from 2002 (24%). The percentage of successful quit attempts was similar among males (34%) and females (37%) and higher in non‑remote areas (39%) compared to remote areas (24%). These findings suggest that despite more quit attempts being made by remote daily smokers, the success rate of these quit attempts is lower than for their non-remote counterparts.
Factors related to quitting
Knowledge about the health effects of tobacco
Direct health impacts
While knowledge on its own is not enough, knowledge of the direct health effects of smoking can be influential in changing smoking behaviour. Concern about these effects is reported as a reason why some people do not initiate smoking and is associated with wanting to quit and making quit attempts [134, 152, 165]. Analysis of the TATS study found that concern for personal health was the most common reason for making a quit attempt, with 93% of smokers citing it as a reason for making a quit attempt in the last six months [134].
Health messaging seems to be particularly effective when it aligns with resonating personal experience. Participants in studies in NSW and SA reported that experiencing smoking‑related health complications, or knowing someone who had, made them want to quit [50, 51]. Another salient concern for some people was the impact of smoking on their fitness and ability to participate in sporting activities [51, 152]. Analysis of the 2014–15 NATSISS data found that 40% of people who tried to quit or reduced their smoking reported improving their fitness as a motivation factor [150].
Impacts of tobacco use during pregnancy
For many women, pregnancy motivates a change in tobacco use [151, 166]. The National Perinatal Data Collection showed that, in 2017, 12% of women who smoked in the first 20 weeks or pregnancy had quit in the second 20 weeks [167]. A 2012 study of pregnant women in NT and NSW found that, of those who were smoking prior to their pregnancy, most (68%) took a step towards quitting, with one in five (21%) quitting and almost half (47%) reducing tobacco use during their pregnancy. Those who did, were found to have a better understanding of the smoking-related risks including miscarriage, low birth weight, infant illness and child behavioural problems, than those who continued smoking [168]. This finding shows that knowledge of the health effects of smoking during pregnancy is a motivator for behavioural change to quit smoking. A 2018 qualitative study with Aboriginal women from Qld, NSW and SA found that, while participants understood smoking was harmful they reported wanting more information to better understand the impacts of smoking during pregnancy [169]. This finding shows that there are still improvements in communicating the health impacts of smoking during pregnancy which is particularly important given the role health knowledge plays in quitting smoking.
Impacts of second-hand smoke exposure
Research has also demonstrated that health information focusing on the indirect health impacts on others can be particularly influential in changing smoking behaviour. Concern for others and the importance of family wellbeing and protecting family members from the negative impacts of smoking can be a key motivator for people to quit smoking [14]. Further, findings indicate that the impact of smoking on others is more influential than the direct effects on the person who smokes. High levels of knowledge of the harmful effects of second-hand smoke is linked with health worry, wanting to quit and making quit attempts, even though knowledge of the direct health impacts alone was not linked with these outcomes [165]. Another study found that 75% of people who made quit attempts reported concern for the effect of cigarette smoke on non-smokers as a reason for quitting [134].
Individuals, organisations, and communities have demonstrated strong support for smoke-free homes and cars. Supporters of these policies are more likely to be non-smokers, compared to people who do not support them [50, 52, 136, 170].
Community factors
Denormalisation
Decreases in smoking prevalence contribute to a denormalisation of tobacco use in communities [171]. Denormalisation of smoking sees a change in the social norms of smoking and a push towards smoking being perceived as an undesirable activity. Community attitudes can influence tobacco use. For example, people who felt that the community leaders where they live disapproved of smoking were almost twice as likely to want to quit than those who did not have that perception [146].
While the denormalisation of smoking can be beneficial in further encouraging smoking cessation and non-initiation, it can also negatively impact on the wellbeing of people who feel stigmatised for continuing to smoke. For many women, tobacco use, even during pregnancy has often been perceived as a socially acceptable response to stress [108]. However, with changing attitudes towards smoking, people who smoke are increasingly concerned about being judged for smoking. A systematic review and thematic synthesis of several studies involving Indigenous women from Australia and New Zealand found that many women wanting to quit felt shame and guilt for their behaviour and concern about stigmatisation. Consequently, these women hid their smoking behaviour to avoid judgement [160].
In addition, studies have found that general practitioners (GPs) and midwives, recognising this fear of judgement, are reluctant to discuss the consequences of smoking with pregnant women as it may be damaging to their relationship [172]. A key informant from Central Australia stated that young pituri users will re-position a quid in their mouths to obscure its presence to avoid feeling ashamed [21]. People who smoke have reported that it is harder for people to smoke nowadays and that they feel the need to smoke in secrecy, together with feelings of guilt for smoking [51]. The TATS study found that 70% of people who smoked daily strongly agreed or agreed that there are fewer and fewer places where they felt comfortable smoking [173].
Family and friends
Given the social role of smoking, the support of family and friends is vital in supporting quit attempts. The evidence shows that people who smoke and who have support from family and friends to quit, make a quit attempt and sustain the quit attempt for at least a month, compared with those who do not have that support [174].
Reports of tobacco use among family, friends and co-workers can discourage quit attempts and make it harder to successfully quit. For someone attempting to quit, the presence of other people smoking and of tobacco creates constant thoughts about smoking. Living in a household with another person who smokes is associated with the maintenance of smoking, including for pregnant women who want to quit [152]. Additionally, people who live with other adults who smoke and people whose five closest friends all smoke are both less likely to make a quit attempt over time [174].
A salient concern commonly reported is that those who choose not to smoke or have quit smoking may risk social isolation [31, 50, 152, 160].
- The TATS study found that over a quarter (27%) of people who smoke daily said that they believed non‑smokers missed out on all the good gossip/yarning [173].
- A 2012 study with SA AHWs found that AHWs feel a need to smoke to facilitate socialisation and connection to community or clients. They feel a social pressure to smoke and fear social exclusion if they were to quit [154].
Role modelling
Many adults have described wanting to be a role model as a key factor in deciding not to smoke, or to quit smoking [14, 134]. Evidence suggests that role models can champion and facilitate smoke free norms [137]. Non-smoking role models have also been found to be influential in preventing smoking initiation [128].
- The TATS study found that 90% of people who smoked daily either agreed or strongly agreed that being a non-smoker sets a good example to children [173].
- It also found that four in every five people who smoke or smoked in the past reported setting an example for children as a reason for thinking about quitting, making quit attempts and helping them to stay quit [134].
- Further, a 2016 study with people from SA, found that both men and women reported changing their smoking behaviour to be good role models to their children to improve their children’s future health outcomes [51].
- In SA and East Arnhem Land in the NT, AHWs have also reported wanting to be good role models for their clients [35, 175]. They explained that quitting smoking would help them advise and help their clients, and keeping smoking would negatively impact their relationships with clients and effectiveness of their messaging.
What is linked with wanting to quit?
Analysis of the TATS study highlights personal attitudes and factors that are linked to individuals wanting to quit smoking. They include:
- Regretting starting
- People who regretted ever starting to smoke were almost three times more likely to want to quit than those who did not have such regrets [146].
- People who agreed that if they had their time again they would not have started smoking have also been found to be more than twice as likely to have made a quit attempt between baseline and follow-up surveys [134].
- Perceived benefits from quitting
- People who perceived high levels of benefits from quitting smoking were almost four and a half times more likely to want to quit than those who did not have such perceptions [146].
- The study also showed that recent quitters had positive attitudes about quitting. Of people who recently quit, 87% said they have more money since they quit, 74% said they cope with stress as well as when they were smoking, and 90% said their life is better now they no longer smoke [161].
- Having lots of worries
- People who reported often having too many worries to deal with were two and a half times more likely to want to quit than those who reported not having too many worries [146].
- Spending too much money on cigarettes
- Eighty-one percent of people who smoke daily reported spending too much money on cigarettes. People who reported spending too much money on cigarettes were more than two times as likely to want to quit and almost one and a half times as likely to have attempted to quit in the last year [161].
- This finding is supported in an analysis of the 2014–15 NATSISS data which found that 59% of people who tried to quit or reduce their smoking reported cost as one of the reasons for doing so [150].
What is linked with not wanting to quit?
In contrast, there are several attitudes that can contribute to people not wanting to stop using tobacco. These include enjoying smoking and believing it is very difficult to quit smoking. Analysis of the TATS study found that people who held these attitudes were less likely to want to quit than those who did not report these attitudes [146].
Some other attitudes that have been reported as contributing to not wanting to quit. These include:
- believing there is no point in their quitting smoking when they were exposed to high levels of second-hand smoke from family and friends who smoke [152]
- believing quitting smoking is not their highest health priority in the context of complex health concerns, such as weight management related to diabetes or heart disease [35, 139, 152], or alcohol or other drug use [152]
- maintaining a fatalistic view of their ill-health, believing that their health was outside of their control [139, 165]
- not trusting, valuing or respecting information about quitting because they:
National policies and strategies impacting tobacco use
Australia has a long history of tobacco control, with the Australian Government taking action to raise awareness about the harms of tobacco use from the early 1970s [19]. A broad range of national, state and territory policies have been developed to address tobacco use in Australia [1, 19]. These include: tobacco tax increases, limiting the tobacco industry’s advertising and promotion, anti‑tobacco mass media campaigns, smoke free legislation and regulation, and support for smoking cessation. Figure 4 provides a timeline of tobacco control policies mapped onto smoking prevalence.
Figure 4 Estimated timeline of tobacco control measures and prevalence of tobacco use
Source: Lovett et al, 2017 [39]
Tobacco control policies and their impact on Aboriginal and Torres Strait Islander peoples
Though not specifically designed or targeted towards Aboriginal and Torres Strait Islander peoples, key tobacco control policies have shaped the tobacco environment for all Australians [121]. Evidence is presented below on the impact of these policies for tobacco use among Aboriginal and Torres Strait Islander peoples.
Tax increases
The cost of cigarettes is a commonly cited reason for Aboriginal and Torres Strait Islander peoples to never smoke or to stop smoking [121, 124, 134, 158]. However, increasing the price after the 2010 tax rise was not found to decrease tobacco consumption in remote communities [176]. This may be because after the price increase smokers just increased the sharing of cigarettes and reliance on family and friends with more disposable income to spend on cigarettes [176].
Plain packaging and health warning labels
Plain packaging and health warning messages on tobacco packaging have improved smokers’ awareness of the health impacts of smoking, and influenced their smoking behaviour [177, 178].
- The introduction of plain packaging has been found to reduce the incorrect perception that some brands of cigarettes were less harmful than others and that some brands were more prestigious than others [179].
- Warning labels have been found to increase smokers’ knowledge of the health impacts of smoking. The TATS study found that people who reported often noticing the warning labels were more likely to correctly answer questions about the health effect of smoking shown in the warnings than people who never or only sometimes noticed the warnings [178].
- The TATS study also found that warning labels impacted smoking behaviour.
- Participants who noticed the warning labels often, as opposed to never or only sometimes, were more likely (78% vs 48%) to want to quit smoking [177]
- A third of participants said that warning labels stopped them from having a cigarette when they were about to have one [177]. This reaction to warning labels was associated with attempting to quit [178].
Smoke-free policies
Smoke-free policies have been shown to be influential on smoking behaviour for Aboriginal and Torres Strait Islander peoples. The TATS study found that:
- those who worked in a smoke-free workplace were almost three times more likely to have smoke-free homes than those who worked in places where smoking was allowed [180], and
- people living in smoke-free homes are also significantly more likely to want to quit, to have made a quit attempt in the past year and to have sustained a quit attempt for one month or longer [180].
Emerging tobacco control approaches
There are numerous emerging tobacco control initiatives [181-183]. These include but are not limited to:
- limiting tobacco retail licenses on a per capita basis
- limiting tobacco retail licenses near schools and community spaces
- smoker’s license or prescription to purchase tobacco
- phasing out tobacco sales
- phasing out the sale of tobacco products to those born in or after a specified birth year. For example, prohibiting the sale of tobacco products to people born in or born after the year 2010
- alternative nicotine delivery systems
- reducing quotas or ’sinking lid’ on tobacco supply by decreasing quotas on sales and/or imports of tobacco products, and
- regulating the cigarette to make it unappealing, specifically regulating nicotine content to limit and/or reduce the amount of nicotine in products over time.
Given the disproportionate impact of tobacco control on Aboriginal and Torres Strait Islander peoples, the consideration, development and implementation of these emerging tobacco control initiatives must align with the UNDRIP and FCTC. Specifically, initiatives must include Aboriginal and Torres Strait Islander voices, leadership and engagement from development to implementation and evaluation.
Policies related to tobacco use among Aboriginal and Torres Strait Islander peoples
In addition to national policies affecting all Australians, there are policies specifically targeted towards Aboriginal and Torres Strait Islander peoples who are a priority population for tobacco initiatives [184]. Table 1 summarises the policies and their targets. While states and territories have developed and implemented their own policies and strategies to reduce tobacco use, this review focuses on national policies and strategies.
Table 1. Aboriginal and Torres Strait Islander peoples-specific tobacco control targets
| Policy name and years | Targets related to tobacco use among Aboriginal and Torres Strait Islander peoples |
| National Aboriginal and Torres Strait Islander Health Plan 2013–2023
|
· Reduce the rate of Aboriginal and Torres Strait Islander youth aged 15–17 years who smoke from 19% to 9%.
· Increase the rate of Aboriginal and Torres Strait Islander youth aged 15–17 who have never smoked from 77% to 91%. · Increase the rate of Aboriginal and Torres Strait Islander youth aged 19–24 who have never smoked from 42% to 52%. · Reduce the smoking rate among Aboriginal and Torres Strait Islander peoples aged 18 plus from 44% to 40%. · Decrease the number of Aboriginal and Torres Strait Islander women who smoke during pregnancy from 47% to 37% [185]. |
| The National Tobacco Strategy 2012–2018 | · Reduce the national adult daily smoking rate from 19% in 2008 to 10% in 2018. This includes reducing smoking among Aboriginal and Torres Strait Islander people, groups at higher risk from smoking, and other populations with a high prevalence of smoking.
· Halve the Aboriginal and Torres Strait Islander adult daily smoking rate from 48% in 2008 to 24% by 2018 [42]. |
| National Aboriginal and Torres Strait Islander Peoples’ Drug Strategy 2014–2019 | · Reduction in the proportion of Aboriginal and Torres Strait Islander people smoking tobacco.
· Four priority areas: 1. build the capacity and capability of services, 2. increase access to culturally appropriate services, 3. strengthen partnerships, and 4. establish meaningful performance measures to support monitoring and evaluation [186, 187]. |
| National Preventative Health Strategy 2009 | · Contribute to the Closing the Gap target to reduce the life expectancy gap between Aboriginal and Torres Strait Islander peoples and non-Indigenous people.
· Work in partnership with Aboriginal and Torres Strait Islander peoples to reduce smoking and exposure to second-hand smoke [188]. · The Strategy was discontinued in 2014 and a new National Preventive Health Strategy is being developed for release in 2020. |
| Council of Australian Governments National Healthcare Agreement 2008 | · Halve smoking prevalence (47.7% to 23.9%) among Aboriginal and Torres Strait Islander people by 2018 [189].
· While this target was not met, positive progress was made in the reduction of tobacco use, especially in younger age groups and people living in urban/regional areas [1]. · This target could be met in the next twenty years if tobacco use continues to decrease at its current rate [1]. |
| Closing the Gap 2008 | · To close the gap in life expectancy between non-Indigenous Australians and Aboriginal and Torres Strait Islander peoples by 2031 [190].
o Includes the indicator: rate of current daily smokers among Australians aged 18 and over, by Indigenous status [191]. · To halve the gap in mortality rates for Indigenous children under 5 within a decade (by 2018) [190]. o Includes the indication: the proportion of mothers who smoked during pregnancy, by Indigenous status [192]. · The 2020 Closing the Gap report stated that the target to halve the gap in life expectancy is on track, and that although there was progress in targets for maternal and child health, the 2018 target was not met [193]. · A new Closing the Gap Framework is under development that aims to work more closely with Aboriginal and Torres Strait Islander peoples [193]. |
| The Framework Convention on Tobacco Control (FCTC) 2003 | · Reduce tobacco use nationally, prioritising at‑risk groups, including Aboriginal and Torres Strait Islander people.
· Take measures to promote the participation of Indigenous individuals and communities in the development, implementation and evaluation of tobacco control programmes that are socially and culturally appropriate to their needs and perspectives [11]. |
Programs to address tobacco use among Aboriginal and Torres Strait Islander peoples
This section will describe the characteristics of successful programs, the key funding for tobacco programs, and the types of programs delivered in Australia. It will synthesise learnings across programs where possible, and provide case studies to highlight what is working. As previously discussed, many population-level tobacco control efforts can work for Aboriginal and Torres Strait Islander communities [121]. However, it is important that programs and services are appropriate for Aboriginal and Torres Strait Islander peoples [194-200].
Characteristics of effective programs
There is currently limited evidence specific to Aboriginal and Torres Strait Islander peoples for most tobacco control programs [194] and more research, monitoring and evaluation of Aboriginal and Torres Strait Islander-specific tobacco control is needed at local, regional and national levels. However, several program features have been highlighted as vital to being successful in addressing tobacco use among Aboriginal and Torres Strait Islander peoples. These features include being culturally appropriate, having a holistic approach to health and being multifaceted in nature [194-199, 201].
Culturally appropriate
The cultural relevance and appropriateness of programs has been shown to be an important factor for their success [194-200]. For a program to be culturally appropriate the program should:
- be developed by, or with Aboriginal and Torres Strait Islander communities
- prioritise and incorporate Aboriginal and Torres Strait Islander voices and leadership to support self-determination and program effectiveness [11, 198]
- build long-term, trusting relationships between program staff and community members to increase community interest and program credibility [198], and
- enable flexible program delivery, to adapt to community needs.
Holistic approach that addresses the social determinants of health
It is vital that programs are based on Aboriginal and Torres Strait Islander ways of knowing and doing. This includes viewing health as holistic and addressing the social determinants of health [194-200]. Aboriginal and Torres Strait Islander perspectives of health and wellbeing, differ from Western medicalised perspectives:
Aboriginal and Torres Strait Islander health means not just the physical well-being of an individual but refers to the social, emotional and cultural well-being of the whole Community in which each individual is able to achieve their full potential as a human being thereby bringing about the total well-being of their Community. It is a whole of life view and includes the cyclical concept of life-death-life. [187, p.36]
Health and wellbeing encompass physical health alongside environmental, spiritual and cultural wellbeing. The historical, cultural and social factors (social determinants) explored earlier in this review should also be considered in holistic programs [187, 197].
A comprehensive multi-faceted approach
Programs that are likely be the most successful in reducing tobacco use are those that incorporate multiple aspects. Programs should involve collaboration and coordination with different community sectors and adopt a whole-community approach [194-199]. This approach allows for the creation of a supportive environment for cessation, in addition to the specific tools and education needed to quit [197].
Programs to address tobacco use among Aboriginal and Torres Strait Islander peoples have largely taken this multi-faceted approach. In a systematic review of international Indigenous tobacco control interventions, all Australian programs included a range of interventions at the individual, community and legislative level such as brief intervention, pharmacotherapy, media campaigns, education, peer support, Quitline, smoking bans, and sale restrictions [198].
Overview of tobacco control programs
Tobacco control programs aim to help smokers and communities understand the health risks of tobacco use and exposure to second-hand and third-hand smoke, and provide smokers with the skills necessary to quit [197, 198, 200]. Tobacco control programs can target individuals (behaviour change programs, training for health workers, and pharmacotherapy), and/or the community (awareness campaigns, community events and promotion of smoke-free environments). Certain programs also target specific subsets of the community, such as youth and pregnant women.
Behaviour change programs
Many behaviour change programs are conducted at an individual level, where health professionals provide advice to patients about the health effects of smoking, the benefits of quitting and provide information on how to quit [198]. The programs often aim to encourage people to attempt to quit smoking and provide support for quitting. Behaviour change programs are often combined with pharmacotherapy.
Brief intervention
A common behaviour change program is the provision of information about quitting smoking by a health professional, called a brief intervention. The 2018 National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people recommends screening all patients for smoking and conducting brief interventions with all current smokers [202]. The health professional: provides clear, specific and personalised behaviour change advice, agrees on a cessation plan with the patient, assists them to arrange cessation support (which could include further information, referral or pharmacological prescriptions) and arranges follow-up visits [202, 203].
The responsibility to conduct brief interventions extends beyond GPs, and is everybody’s business. Nurses, reception staff, Aboriginal and Torres Strait Islander Health Professionals, and other health professionals can all play a role in incorporating the recording smoking status and providing brief interventions for smokers into regular practice [204].
Brief interventions are widely practiced. The TATS study reported that 75% of Aboriginal and Torres Strait Islander people who smoked daily who had seen a health professional in the past year had been advised to quit. Some patients were provided with a brochure or were referred to quit services including Quitline and websites or quit groups [205].
Brief interventions have been shown to be successful in the non-Indigenous population [206]. It is difficult, however, to determine how much change can be attributed specifically to the brief intervention given they are often run in conjunction with other types of interventions [197].
There is some evidence that brief interventions promote change in tobacco use attitudes and behaviours for Aboriginal and Torres Strait Islander peoples. Evidence shows that:
- being advised to quit by a health professional increases smokers’ motivation to quit [146], and
- patients advised to quit by a health professional in the past year were twice as likely to attempt to quit compared with those who were not [205].
Some Aboriginal and Torres Strait Islander peoples have also stated that brief interventions and one‑on-one support were their preferred form of quit support [207].
Brief interventions, and all tobacco programs, should be culturally appropriate. A 2010 study in the NT found that brief interventions were effective in a primary care setting. However, additional training of staff members was required to ensure the appropriateness of the intervention for Aboriginal and Torres Strait Islander peoples [208].
To support the delivery of culturally appropriate brief interventions, an Aboriginal and Torres Strait Islander people-specific brief intervention program called SmokeCheck was developed. The program provides training to health professionals, including: AHWs, doctors, nurses, social workers, counsellors and alcohol, drugs and tobacco workers, to deliver more appropriate and supportive mechanisms to assist Aboriginal and Torres Strait Islander peoples to quit [209, 210]. An evaluation of the program published in 2011 found that health professionals who undertook the SmokeCheck training felt more confident to deliver culturally appropriate advice and information. Further, Qld Health report an increase in quit attempts and a decrease in smoking prevalence since the implementation of the program [210, 211]. However, it has been noted that, as with other brief interventions, implementation of SmokeCheck is challenged by competing health priorities and time constraints of health workers [212].
Telephone support: Quitline
Health professionals can refer patients to Quitline, a one-on-one phone-based quit counselling service [213]. Quitline services have dedicated Aboriginal and Torres Strait Islander quit counsellors and staff to assist Aboriginal and Torres Strait Islander smokers in quitting [207, 213]. People can also self-refer to Quitline. In fact, most (58%) calls made in 2017 were self-referrals rather than health professional referrals [207]. Between January 2016 and December 2017 there were 7,629 calls made to Quitline by Aboriginal and Torres Strait Islander people, representing a 12% increase in the number of calls [207].
There is scope to increase the number of health professionals referring patients to Quitline. The TATS study found that, of participants who were advised to quit smoking only 28% were referred to Quitline [205]. Further, utilisation of the service once referred could be improved. The TATS study found that less than 20% of those referred to Quitline actually used the service [205]. A study in SA found that Aboriginal and Torres Strait Islander peoples made up only 2.8% of callers who signed up for call back services. This was only about 3.6% of all Aboriginal and Torres Strait Islander smokers in SA [213].
A national survey found that those who were referred to Quitline were more likely to make a quit attempt than those who were not (60% vs 55%) [205]. A study in SA found that 4.3% of people who called Quitline had set a date that they would quit by, and 2.5% of callers reporting they were still quit three months after the first call [213].
Support groups
In addition to one-on-one counselling and support, there are also programs where smokers work together to change their behaviour [207]. These programs are often run by an AHW or an Aboriginal or Torres Strait Islander ex-smoker. Support groups can either be solely focused on smoking and helping people quit, or can be focused on healthy lifestyles or walking groups where smoking is one of the focuses [207].
Though many tobacco control programs include an element of peer support, there is as yet little robust Aboriginal and Torres Strait Islander-specific evidence for the outcomes of support groups [197]. A 2014 evaluation of community-based tobacco control programs in remote north Qld found that the ‘Smoke Rings’ group support program had low uptake and engagement and was not implemented as originally intended. From this study, challenges in running a support program include: finding a health worker to run the programs, targeting current smokers, participation drop-off, with fewer participants attending in each subsequent session [212].
Pharmacotherapy
There are three main pharmacotherapies used in Australia to support tobacco cessation: (1) nicotine replacement therapy (NRT), (2) bupropion, and (3) varenicline, which are all subsidised through the Pharmaceutical Benefits Scheme (PBS) [214]. NRT provides lower doses of nicotine than tobacco and does not contain some of the other harmful components of tobacco use. NRT is suitable for most of the population over the age of 12 years and should be used for 8–12 weeks [215]. Varenicline and bupropion do not contain nicotine, but treat nicotine withdrawal symptoms [215]. They have potential side effects and are not recommended for all population groups. If smokers are having difficulty quitting using only NRT, it is possible to use NRT in combination with varenicline or bupropion [215].
In the TATS project, 37% of Aboriginal and Torres Strait Islander daily smokers had ever used a NRT product or bupropion or varenicline, with 23% using one of these products in the last year [214].
Research indicates that cost was a major barrier to accessing pharmacotherapy [208]. Subsidised NRT patches became available to Aboriginal and Torres Strait Islander peoples in 2009 under the PBS, bupropion in 2001 and varenicline in 2008. Remote Aboriginal health services have been able to dispense these PBS items at no cost under Section 100 of the National Health Act 1953. Non-remote services have been able to reduce or eliminate the co-payment for PBS medicines for Aboriginal and Torres Strait Islander peoples since 2010 under the Indigenous health Incentive of the Practice Incentives Program [214]. Since the introduction of these measures, the TATS study found that 74% of smokers in 2012–13 had received their last NRT at low or no cost [214]. Provision of NRT at low or no cost is a component of many tobacco control programs at Aboriginal community controlled health services (ACCHSs). The TATS study found that 25 of the 32 ACCHSs they surveyed provided NRT at low or no cost for their patients [170]. This may improve accessibility of these products and increase their uptake [216].
Pharmacotherapy has been shown to assist smokers to quit, especially when combined with additional support from health professionals and behaviour change programs [195]. While there is little evidence of the effectiveness of these therapies for Aboriginal and Torres Strait Islander peoples, the TATS study found that people who had used pharmacotherapy believed these products had helped them to quit and that they would use them in the future [214].
Social and mass media campaigns
Social and mass media campaigns make use of a whole range of media forms to increase knowledge about the harms of tobacco use and exposure to second-hand smoke. Media forms used include: television advertisement, social media advertisement, and smartphone applications and sponsorship of community, cultural and sporting events [207].
General tobacco control messaging is an effective way to raise awareness and encourage Aboriginal and Torres Strait Islander peoples to think about quitting; however, implementing specific targeted messaging has been shown to increase the impact within community [146]. Targeted messaging should be developed with Aboriginal and Torres Strait Islander peoples and communities and present information in a culturally appropriate way [217]. Due to place-based Tackling Indigenous Smoking (TIS) funding, there has been an increase in the number of Aboriginal health services running localised social and mass media quit and education campaigns [207] (see below for more on the TIS program).
In the Cultural and Indigenous Research Centre Australia (CIRCA) evaluation of the TIS program community members stated that having ads with local champions were motivational and memorable. One participant stated:
…you look up to those Elders, it’s really good it makes us stand up a little bit more and have another think about it. It’s good to have someone who has been there and smokes, ‘cos you know they have been there and done that, if they can do it I can do it. [207, p.24]
The rationale being that smokers see people who have successfully quit or who are healthy and want to be more like them.
This suggests that incorporating community leadership in the development of messages make them more impactful [146]. Social media is common, with 74% of Aboriginal and Torres Strait Islander peoples being a member of a social networking site in 2014 [218]. Tobacco control messaging on social media platforms has the potential to reach large proportions of the population. One way in which health services can harness this potential is to incorporate local social media influences or ambassadors to promote and share videos within their network [219].
One example of a community awareness campaign is Deadly Choices, which raises awareness of healthy choices people can make to improve their health [220]. The program aims to build community capacity and engagement and incorporates community-based education with social media health education. The key smoking education messages include highlighting the chemicals in cigarettes and the negative health effects of smoking and passive smoking. Participants can also take a carbon monoxide test (also commonly referred to as a smokerlyzer test) to determine exposure to smoke [220]. Deadly Choices activities are held across South East Qld in conjunction with the local Aboriginal and Torres Strait Islander health services. The community-based education has seen Aboriginal and Torres Strait Islander health professionals support communities to make more informed health decisions and promote smoking cessation, as well as referring people for additional supports [220]. Large community educational programs, such as Deadly Choices, have improved community awareness and education about smoking [220].
While awareness campaigns can help to shift attitudes around smoking [200], they are not always linked to cessation attempts [221]. These campaigns should be run in conjunction with other forms tobacco control initiatives to successfully reduce tobacco use [221].
Community and cultural events
Sponsoring of community events and/or holding stalls at local cultural or sporting events is one of the most common awareness raising and smoking cessation activities within communities [207]. Community events are an opportunity for local health workers and smoking resistance teams to engage with communities and raise awareness of their work. Stalls at community events often consist of educational and health promotion materials, as well as carbon monoxide testers [207]. In 2017, 93% of TIS workers surveyed stated that they agreed or strongly agreed that community events increase community understanding of the health impacts of tobacco use [207]. These events are also an opportunity to run smoke-free events to reduce exposure to second-hand smoke and de-normalise tobacco use [222].
Tackling Indigenous Smoking – an example of a tailored, multi-faceted approach
The national funding model for programs to address tobacco use among Aboriginal and Torres Strait Islander peoples is the Tackling Indigenous Smoking (TIS) program (2016–2022). TIS is designed to allow for local tailoring and takes a multifaceted approach. It emphasises: the use of evidence-based approaches; promotion of best‑practice approaches to tobacco control; building partnerships across services; reducing tobacco use; and increasing collaboration in the delivery of tobacco campaigns [223].
TIS is comprised of a number of elements (Figure 5) [207, 222].
- Regional Tobacco Control Grants – provided for 37 organisations to undertake multi‑level and evidence-based population health approaches that suit their context and utilise their community strength.
- The National Best Practice Unit – supports grant recipients in their planning and implementation of approaches and generation of evidence.
- The National Coordinator Tackling Indigenous Smoking – provides support and leadership for both grant recipients and the Commonwealth Government.
- Innovation grants for priority groups – supports activities for pregnant women, youth and smokers in remote areas.
- Quitline enhancements grant – supports the improvement of Quitline’s capacity to service target populations.
- Quitskills training – intervention and motivational interview training in best-practice methods.
- National evaluations – process evaluation and program improvement evaluation and an impact and outcome evaluation.
Figure 5: Tackling Indigenous Smoking Program
Source: Australian Indigenous HealthInfoNet (2019) [222]
TIS has been structured to meet the need for culturally appropriate, local, Aboriginal and Torres Strait Islander-led and, multifaceted approaches to tobacco control. Thirty-seven organisations, mostly Aboriginal community controlled health organisations (ACCHOs) received Regional Tobacco Control Grants to undertake prevention programs within their local area [222]. Most TIS activities are focussed on the community and include:
- increased involvement in tobacco control activities
- education about the harmful effects of tobacco use, and the positive health outcomes of being a non-smoker
- increasing smoke-free environments and reducing passive smoke exposure, and
- providing clinical support.
The TIS program is currently undergoing a process evaluation and program improvement evaluation as well as an impact and outcome evaluation. Conducted by CIRCA and the Australian National University respectively, these two comprehensive reviews will analyse if the approach used by TIS is reducing Aboriginal and Torres Strait Islander peoples’ tobacco use. These evaluations are expected to help to address the evidence gap.
Priority group programs
Reducing smoking rates within at-risk populations, including pregnant women and young people, is a priority within communities, the Government and the health sector [185].
Pregnant women
Interventions already outlined in this section, primarily NRT and behavioural change programs have been shown to have some success in reducing smoking rates among pregnant women in the general population, but have largely not been measured for Aboriginal and Torres Strait Islander peoples [224, 225]. Pregnant women are a priority population and a key component of TIS. TIS teams run pregnancy groups and support sessions for expectant and new parents with a focus on education and cessation support [222, 226]. There are some key differences in providing cessation support to pregnant women, compared to other people who smoke.
Firstly, varenicline and bupropion are not recommended during pregnancy, but if counselling alone is unsuccessful short-acting NRT can be considered [222]. NRT (e.g. inhaler or lozenge) has been shown to be an effective intervention during pregnancy. However, pregnant women metabolise nicotine at a faster rate meaning they require higher doses of NRT compared to non‑pregnant women [227, 228]. National guidelines recommend using intermittent oral NRT (e.g. inhalers or lozenges) [202]. A 2015 systematic review found that use of NRT increased cessation in pregnant women by 40% [229]. Despite these findings, a cross sectional survey of the provision of smoking cessation care given to pregnant women found that only 11% of health professionals reported always prescribing NRT to pregnant women, suggesting the need for training and updating standard practice to ensure optimal care for expecting families [230].
Secondly, in developing tobacco programs for expectant mothers it is important to ensure the programs not only target mothers, but also communities and families in order to foster a more supportive environment for quitting and address the broader context and lives of the women [226]. This broader approach to quitting smoking has been found to be particularly important for Aboriginal and Torres Strait Islander expectant mothers. A 2019 study in urban Qld highlighted the importance of holistic care for women in pregnancy [108]. The program involved three components: activities that celebrated culture and aimed to enhance social and emotional well-being; case management support; and individual cessation support including motivational interviewing, NRT and financial incentives. Nearly all participants reported making positive changes in their smoking behaviours, four women (36%) quit during their pregnancy, and two remained smoke-free in the early post-partum follow up period. In addition to changes in smoking behaviour, the program addressed the context of the women. The researchers found that many women participating in the program were experiencing multiple stressors. Women in the study reported that building trusting relationships with the case managers supported them to have a more positive outlook, bond with their unborn child and make positive changes to their smoking attitudes and behaviours [108]. This study highlights the importance not only of direct intervention in smoking behaviour, but in providing support to address the social determinants of health which acts as barriers for quitting smoking, particularly for pregnant women.
While evidence of tobacco control programs for pregnant women is sparse [224], there are some tobacco control programs designed specifically to support Aboriginal and Torres Strait Islander women to quit smoking during pregnancy for which there is some research and evaluation evidence available.
Yarning circles with Aboriginal women from NSW, SA and Qld found that the women were interested in interactive, informational, non-pharmacological resources to help them quit smoking [48]. It is also important that resources are culturally appropriate, engage with the family and communities of the pregnant women, practical to use in the short time frames health professionals have with patients [231].
A randomised controlled trial of intensive quit-smoking interventions for pregnant Aboriginal and Torres Strait Islander women found no significant difference in smoking rates for women who received the intervention than women who received usual care. These results may have been affected by the large number of people who left the study before it was complete [47]. Although the trial did not see significant results, intensive interventions should not be discounted, but rather more evidence is needed to determine interventions which reduce tobacco use in pregnant women [232].
ICAN QUIT
The Indigenous Counselling and Nicotine (ICAN) QUIT in Pregnancy aims to train health professionals (GPs, AHWs, midwives) to provide culturally responsive, evidence based cessation care to expectant Aboriginal and Torres Strait Islander women [231]. It was developed in collaboration with AMSs, Aboriginal and Torres Strait Islander women, and communities. The ICAN QUIT program provided: training for health professionals on brief interventions and the use of NRT for pregnant women, free oral NRT for the women, and a carbon monoxide breath meter (sometimes known as a smokerlyzer or CO monitoring) for health professionals [228].
While the knowledge of health professionals improved in a pilot study of ICAN QUIT, self-reported practices remained unchanged, including prescription of NRT [233]. More intensive measures are needed to change NRT prescription rates.
Financial incentives
An intensive strengths-based smoking cessation program using financial incentives for pregnant Aboriginal women called Stop Smoking in its Tracks was piloted in three rural sites [234]. The program used individually-tailored counselling, free NRT, household engagement and support, educational resources, peer support groups and contingency-based financial rewards. This was the first study to assess the use of contingency-based financial rewards for smoking cessation among pregnant women. An evaluation found that 19 of the 22 participants completed the program. Fifteen (79%) of the participants reported a sustained quit attempt lasting more than 24 hours and eight were not smoking in late pregnancy. The health professionals delivering the program reported that the program was positive, comprehensive and valued by the participants. The program intensity provided challenges for staff and participants, but this sustained, regular support was deemed critical to supporting quit attempts. It was noted that this support helped to address the other social issues women were facing, and included support for other members of their household which can be barriers to quitting smoking [234].
Youth and children
Tobacco programs have been specially designed to discourage and prevent smoking uptake by young people and encourage young people to quit smoking. Tobacco workers and qualitative studies with youth highlight the importance of prioritising youth and shifting social norms around smoking in the community and immediate social environment of youth [162, 207]. Specific youth programs include: school‐based programs, mass media campaigns, targeted advertisement campaigns, multi‑component community interventions involving schools and families, and local peer role models and ambassadors [196, 207]. Parental attitudes and smoking are important determinants of youth uptake of smoking, so programs to reduce adult smoking and to promote smoke-free homes are also part of reducing youth uptake [235].
An example of a targeted mass media campaign is the No Smokes project which was designed to give youth access to targeted anti-tobacco messaging, educate them on the adverse effects of smoking and provide knowledge about quitting strategies [236]. The project found that youth were most likely to recall hard-hitting or personally relevant messages. Factual videos and repetition of key messages were the most effective in increasing knowledge about the adverse effects of smoking and humorous videos were least effective. The use of unfamiliar or technical terminology undermined access to anti-tobacco messaging [236].
Social media also plays an important role in youth programs. Deadly N Ready, is a youth-led social marketing campaign focused on preventing smoking initiation in young people. Following the campaign, youth reported encouraging someone to quit smoking and, prompting conversations about smoking with friends and family [207]. TIS teams also report using social media to target youth [207].
While many tobacco programs targeting youth have been trialled, few have yet been rigorously evaluated [199, 237]. A 2017 overview of systematic reviews found that results of studies targeting Aboriginal and Torres Strait Islander youth were unclear and non-significant for tobacco use at final follow-up [194]. Another systematic review of 91 tobacco cessation and prevention studies (including eight programs targeting Aboriginal and Torres Strait youth) found unclear results for youth but that interventions with more components, and greater intensity, were more likely to be effective than those of shorter duration and lower intensity [195].
Opportunities in addressing tobacco use
Programs aimed at reducing tobacco use could be enhanced through expanded and long-term funding and rigorous evaluation evidence.
Most programs have intermittent short-term funding which leads to short program duration and scale [238]. A systematic review of 91 smoking cessation and tobacco prevention studies for global Indigenous populations found 25 tobacco cessation interventions which included final results. Of these interventions, none were run for longer than 12 months and 80% were six months or less [195]. Short-term funding can undermine community control of programs as researchers and funders can have unrealistic expectations of the outcomes of programs compared to what is achievable by the community in short time frames [239].
In part due to the funding issues, there is not published evaluation evidence of most programs [197, 240]. Without robust evidence in the public domain, it is difficult to identify the components of existing programs that successfully lead to long‑term changes in smoking attitudes and behaviours. This evidence is vital to the planning of services, and in securing long-term funding for programs [195]. The cyclical nature of the problem means that limited funding contributes to a lack of program evaluations, which in turn reduces the ability to obtain ongoing funding. A systematic review found that interventions run for a longer period of time are more likely to be successful than those run over short periods of time [195].
There is opportunity to conduct both local and large-scale evaluations of tobacco programs and policies to reflect the diversity of Aboriginal and Torres Strait Islander peoples and communities.
Concluding comments and future directions
There have been significant reductions in tobacco use among Aboriginal and Torres Strait Islander peoples in recent decades [1, 3]. However, the prevalence of tobacco use is still too high, and further reductions are achievable.
As detailed throughout the review, the negative effects of smoking, and the benefits which come from quitting and being smoke free, are substantial [40, 104, 241-246]. Successful smoking cessation and avoiding smoking initiation are complex behaviours influenced by historical and contemporary systemic factors [19]. Reducing tobacco use at the population level requires a suite of comprehensive approaches to halt initiation and promote cessation [11, 194]. These approaches must reduce underlying social and economic exclusionary factors. As discussed in this review, Aboriginal and Torres Strait Islander peoples experience structural discrimination and barriers to participating in education and employment, which are key factors protective against smoking. To reduce smoking, it is therefore important to ensure all Aboriginal and Torres Strait Islander peoples have access to appropriate education and employment opportunities. Information about tobacco addiction and harms needs to be available facilitate empowered Aboriginal and Torres Strait Islander peoples to make informed choices about tobacco use.
The United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) and the Framework Convention on Tobacco Control (FCTC) provide the foundation for Aboriginal and Torres Strait Islander tobacco control. UNDRIP states that ‘Indigenous peoples have the right to self‑determination’ and that ‘Indigenous peoples have the right to maintain, control, protect and develop their cultural heritage, traditional knowledge and traditional cultural expressions’ [10, p.4, 22]. Further, the FCTC is an evidence‑based treaty that reaffirms the right to the highest standard of health and recognises the disproportionate harm of tobacco use among Indigenous peoples. The FCTC complements the UNDRIP, recognising the fundamental need to engage with Indigenous peoples in planning, delivering, and evaluating tobacco control [11]. In other words, Aboriginal and Torres Strait Islander self‑determination is critical to tobacco control and tobacco use.
We propose key actions required to further reduce tobacco use. These actions are in the domains of: the historical and social determinants of tobacco use; legislation and policies; social marketing; comprehensive programs; and research and evaluation. The actions, those responsible for undertaking each action, and the nature of that responsibility, are summarised in Table 2.
Substantial recent progress has been made in reducing tobacco use which will translate to reductions in tobacco related morbidity and mortality both in the short and long term. While this is positive news, there are opportunities to accelerate declines in smoking, and associated health gains. To this, we need to expand the evidence base on what works to reduce smoking, incorporating knowledge from Aboriginal and Torres Strait Islander peoples and service providers. To enhance these current positive trends, all Aboriginal and Torres Strait Islander peoples, regardless of location or other characteristics, need to have access to effective and appropriate tobacco control programs and initiatives.
Table 2: Recommended future actions in Aboriginal and Torres Strait Islander tobacco control
| All action must be driven and governed by Aboriginal and Torres Strait Islander communities, in line with local and/or national needs. | ||||||
| Domain | Action | Responsibility | ||||
| Australian Government | State and Territory governments | Aboriginal and Torres Strait Islander health organisations | Evaluators, research and academic institutions | Non-government organisations | ||
| Historical and social determinants of tobacco use | Recognise the ongoing contribution of colonisation to tobacco use by Aboriginal and Torres Strait Islander peoples. | Incorporation into policy and frameworks | Incorporation into policy and frameworks | Advocacy | Advocacy and evidence | Advocacy |
| Deliver programs to support Aboriginal and Torres Strait Islander peoples to heal from the intergenerational trauma stemming from colonisation. |
Secure funding commitment
|
Secure funding commitment | Delivery and partnerships | Collecting and disseminating evidence of wise practice | Partnerships | |
| Strengthen commitment to reducing systemic barriers to health, specifically employment and education. | Legislation, policy and programs | Legislation, policy and programs | Advocacy | Advocacy and evidence | Advocacy | |
| 1 Legislation and policies
|
Aboriginal and Torres Strait Islander peoples to guide the development and review of legislation. | Collaboration | Collaboration | Advocacy and collaboration | Advocacy | Advocacy |
| Protect Aboriginal and Torres Strait Islander-specific and general tobacco control policies. | Policy commitment | Policy commitment | Advocacy | Advocacy | Advocacy | |
| Design legislation and policies to ensure that all Aboriginal and Torres Strait Islander peoples have access to population-based tobacco control (including social marketing) and individual cessation support. | Collaboration | Collaboration | Advocacy and collaboration | Advocacy | Advocacy | |
| Ensure ongoing policy monitoring and review that includes Aboriginal and Torres Strait Islander voices. | Funding and collaboration | Funding and collaboration | Advocacy and collaboration | Collecting and disseminating evidence | Advocacy | |
| 2 Social marketing
|
Implement and expand Aboriginal and Torres Strait Islander-specific national, state and territory tobacco campaigns, including a balance of existing material with proven effectiveness and a suite of new materials. | Delivery | Delivery | |||
| Tailor social marketing activities and other health promotion activities to meet the needs of Aboriginal and Torres Strait Islander peoples. | Collaboration | Collaboration | Collaboration | Collecting and disseminating evidence | ||
| Monitor the effectiveness of recommended media weights and media types/channels, including exploration of the role of digital media. | Funding | Funding | Collecting and disseminating evidence | |||
| 3 Comprehensive programs
|
Develop and deliver holistic, culturally safe tobacco services. | Funding | Funding | Delivery | Collecting and disseminating evidence | |
| Fund health services and programs to support ongoing, long-term and sustainable delivery. | Funding | Funding | Advocacy | Advocacy | Advocacy | |
| Streamline administrative processes for application and reporting on tobacco services. | Rationalisation | Rationalisation | Advocacy | Advocacy | Advocacy | |
| Research and evaluation
|
Conduct appropriate research, monitoring and evaluation of Aboriginal and Torres Strait Islander tobacco use and tobacco control at local, regional and national levels. | Funding | Funding | Sharing and collaboration | Collecting and disseminating evidence | |
| Create opportunities for health workers and other relevant professionals to network, communicate and share information and wise practices regarding Aboriginal and Torres Strait Islander tobacco control. | Facilitate | Facilitate | Sharing and collaboration | Collecting and disseminating evidence | ||
Appendix 1: Glossary and acronyms
Glossary
| Atherosclerosis | Atherosclerosis is a condition that occurs when too much plaque builds up in arteries, causing them to narrow. It is the process that underlies the development of coronary heart disease, most cerebrovascular disease, and peripheral arterial disease. |
| Bronchiolitis | A condition affecting the small breathing tubes in the lungs caused by a viral infection. It is common in babies under six months of age, although it can occur in babies up to 12 months. |
| Bush tobacco | Bush tobacco (Nicotiana spp.) is prepared by drying the leaves, mixing them with ash to make nicotine available, and chewing to form a ‘quid’. Quids are then either held in the mouth or stored on the body – often behind the ear – where the nicotine is absorbed through the skin. Bush tobaccos contain roughly 1% nicotine. |
| Carcinogen | A substance that causes cancer in the body. |
| Cerebrovascular disease (CBVD) | A disease of the vessels that supply blood to the brain, which can result in stroke. Ischaemic cerebrovascular disease, caused by build‑up of plaque in the blood vessels, is the most common form. A smaller proportion of this disease is haemorrhagic (due to rupture of blood vessels). |
| Chronic obstructive pulmonary disease (COPD) | A group of lung diseases in which there is chronic irreversible airflow obstruction due to permanent changes in the airway tissue. Includes emphysema, chronic bronchitis and chronic asthma (as opposed to asthma in which the airflow obstruction is reversible). Bronchiectasis is sometimes included in this disease. |
| Coronary heart disease (CHD) | A cardiovascular disease caused by plaque build-up in the wall of the arteries that supply blood to the heart (called coronary arteries) that can lead to angina and heart attack. Coronary heart disease is also known as ischaemic heart disease. |
| Disability-adjusted life years (DALY) | The total years of potential life lost due to early death and the years of productive life lost due to disability. One Disability-adjusted life year is equal to one lost year of healthy life. |
| E-cigarettes | E-cigarettes are battery operated devices that heat a liquid which produces an inhalable vapour. The liquid varies in composition, typically containing solvents and flavouring agents, and may or may not contain nicotine. |
| Ectopic pregnancy | When a fertilised egg implants itself outside the womb, usually in one of the fallopian tubes. This means the embryo will not be able develop into a baby as the fallopian tube is not large enough to support the growing embryo. |
| Endothelium | The lining of blood vessels. |
| Fibrin | A clotting material in the blood. |
| Myocardial infarction (MI) | Also known as heart attack. A heart attack occurs when a blockage in one or more coronary arteries reduces or stops blood flow to the heart, which starves part of the heart muscle of oxygen. |
| Neonatal | Newborn (usually considered to be the first month of life). |
| Perinatal deaths | Stillbirths and deaths of babies within the first 28 days of life. |
| Peripheral arterial disease (PAD) | The narrowing or blockage of the vessels that carry blood from the heart to the legs, caused by the build-up of fatty plaque in the arteries. It can occur in any blood vessel, but it is more common in the legs than the arms. Peripheral arterial disease can lead to foot ulcers, necrosis and amputation. |
| Pituri | (D. hopwoodii) is a form of native tobacco which is prepared is by drying the leaves, mixing them with ash to make nicotine available, and chewing to form a ‘quid’. Quids are then either held in the mouth or stored on the body – often behind the ear – where the nicotine is absorbed through the skin. It is a powerful stimulant, containing up to 8% nicotine. |
| Placenta praevia | When the placenta attaches in an abnormal position inside the uterus near or over the cervical opening. |
| Placental abruption | When the placenta detaches early from the uterus. |
| Pre-diabetes | A condition in which blood glucose levels are higher than normal, although not high enough to be diagnosed with type 2 diabetes. Pre-diabetes has no signs or symptoms. People with pre-diabetes have a higher risk of developing type 2 diabetes and cardiovascular (heart and circulation) disease. |
| Preterm delivery | Birth of a baby before 37 weeks of pregnancy. |
| Quid | A portion or wad of tobacco to be chewed. |
| Second-hand smoke | The ambient smoke that is a by-product of active smoking. It is mainly made up of exhaled smoke and sidestream smoke (smoke that comes from the lighted end of a burning tobacco product) mixed with air. |
| Small for gestational age (SGA) | A baby is smaller than expected for the number of weeks of pregnancy. Although some babies are small because their parents are small, most babies who are small for gestational age have growth problems that happen during pregnancy. |
| Stillbirth | The death of a foetus weighing at least 400 grams or having a gestational age of at least 20 weeks. |
| Sudden Infant Death Syndrome (SIDS) | The sudden and unexpected death of a baby less than one year old, apparently occurring during sleep, which remains unexplained after a thorough investigation |
| Sudden Unexpected Death of the Infant (SUDI) | The sudden and unexpected death of a baby less than one year old in which the cause was not obvious before investigation. |
| Third-hand smoke | Components of tobacco smoke that remain on surfaces and in dust after tobacco has been smoked. These substances are then re‑emitted as gases or react with other compounds in the environment to create other substances. |
| Thromboembolism | Blockage of a blood vessel by a blood clot that has become dislodged from another site in the circulation. |
| Thrombosis | The formation or presence of a blood clot within a blood vessel |
| Type 2 diabetes | A chronic condition in which body cells do not respond to insulin properly (insulin resistance) and the pancreas does not produce enough insulin, so glucose builds up in the blood instead of getting into cells for energy. High blood glucose levels over time can contribute to the development of coronary heart disease, cerebrovascular disease, peripheral arterial disease, kidney and eye disease and dementia. |
Acronyms
| ABS | Australian Bureau of Statistics |
| ACCHO | Aboriginal community controlled health organisations |
| ACCHS | Aboriginal Community Controlled Health Service |
| ACT | Australian Capital Territory |
| AHW | Aboriginal Health Worker |
| BAT | British America Tobacco |
| CHD | Coronary heart disease |
| CIRCA | Cultural and Indigenous Research Centre Australia |
| COPD | Chronic obstructive pulmonary disease |
| DALYs | Disability-Adjusted Life Years |
| DNA | Deoxyribonucleic acid |
| GP | General practitioner |
| LSIC | Footprints in Time: The Longitudinal Study of Indigenous Children |
| MI | Myocardial infarction, also known as heart attack |
| NATSIHS | National Aboriginal and Torres Strait Islander Health Survey |
| NATSIS | National Aboriginal and Torres Strait Islander Survey |
| NATSISS | National Aboriginal and Torres Strait Islander Social Survey |
| NRT | Nicotine replacement therapy |
| NSW | New South Wales |
| NT | Northern Territory |
| PAD | Peripheral arterial disease |
| PBS | Pharmaceutical Benefits Scheme |
| PMI | Philip Morris International |
| Qld | Queensland |
| SA | South Australia |
| SIDS | Sudden Infant Death Syndrome |
| SUDI | Sudden Unexpected Death of the Infant |
| TATS study | Talking about the Smokes study |
| THS | Third-hand smoke |
| TIS | Tackling Indigenous Smoking |
| UNDRIP | United Nations Declaration on the Rights of Indigenous Peoples |
| Vic | Victoria |
| WA | Western Australia |
| WHO FCTC | World Health Organization Framework Convention on Tobacco Control |
Appendix 2: Smoking and health conditions
Table 3: Key studies providing latest evidence of association between smoking and health conditions in Aboriginal and Torres Strait Islander populations.
| Health condition | Source | Population studied | Study Design | Findings | Limitations |
| Effects of smoking on the smoker | |||||
| Coronary heart disease (CHD), ischaemic stroke and peripheral arterial disease (PAD) | Luke et al., 2013 [247] | Aboriginal people living in 3 Central Australian communities | Longitudinal
n*=739
|
· A substantial, but not statistically significant, difference in the prevalence of current smoking between those who developed CHD, ischaemic stroke or PAD over the 10-year follow-up period, and those who did not (41.2% vs 30.5%; p = 0.072).
· Current smoking should be included in algorithms for predicting cardiovascular disease risk. |
· Former smokers, smoking duration, and smoking intensity not accounted for in the analysis. |
| Coronary heart disease | Wang and Hoy, 2013 [241] | Aboriginal people living on a remote island, NT | Longitudinal
n=1,115
|
· Prevalence of smoking at baseline was significantly higher among participants who developed CHD after 20 years, compared with those who did not (69.2% vs 55.5%, p=0.003). | · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis.
· CHD may be under-reported in hospital records used as the source of data for the outcome measure. |
| Increased carotid intima-media thickness (IMT, the thickness of the artery wall) a precursor of atherosclerotic disease | McDonald et al., 2004 [242] | Aboriginal people in a remote community | Cross-sectional
n=237 |
· People with carotid IMT had higher odds of being a current smoker (adjusted OR 3.04 95% CI 1.12–8.22, p = 0.03). | · Carotid IMT does not explain all of the risk of cardiovascular events and mortality.
· Former smokers, smoking duration, and smoking intensity not accounted for in the analysis. |
| Increased carotid IMT | Chan et al., 2005 [243] | Indigenous people on North Stradbroke Island, Qld | Cross-sectional
n=119 |
· Thicker carotid IMT was associated with being a current smoker (p=0.04). | |
| Higher levels of fibrinogen in the blood (a risk factor for atherosclerosis) | Maple-Brown et al., 2010 [244] | Urban Indigenous people from Darwin, NT | Cross-sectional
n=915 |
· No association between fibrinogen and being a current
cigarette smoker (compared to former or never smoked combined). |
· High blood fibrinogen does not explain all of the risk of cardiovascular events and mortality.
· Former smokers, smoking duration, and smoking intensity not accounted for in the analysis. |
| Higher levels of fibrinogen in the blood | Wang et al., 2007 [248] | Aboriginal and Torres Strait Islander people from 11 communities in Cape York, Torres Strait and Central Australia | Cross-sectional
n=1,128 |
· No association between fibrinogen and being a current
cigarette smoker (compared to former or never smoked combined). |
|
| Chronic obstructive pulmonary disease (COPD) | Kruavit et al., 2017 [245] | People referred to respiratory specialist outreach team visiting clinics in remote Top End communities, NT | Retrospective cross-sectional
Aboriginal n=352 Non-Indigenous n=92 |
· Current smokers (RR 26.19, 95% CI 10.93–62.77, p<0.001) and ex-smokers (RR 12.56, 95% CI 5.34–29.52, p<0.001) were significantly more likely to have COPD than non-smokers. | · Only included people who were referred to the service.
· Former smokers, smoking duration, and smoking intensity not accounted for in the analysis.
|
| Lung function abnormalities (Post-bronchodilator [non-reversible] airflow limitation and lung capacity) | Schubert et al., 2019 [246] | Aboriginal people referred to respiratory specialist outreach team visiting clinics in remote Top End communities, NT | Retrospective cross-sectional
n=150
|
· There was no difference in lung function between current smokers and former/never smokers. Other factors may contribute in this population (e.g. nutrition, childhood respiratory infections, air pollution). | |
| Cancer | Li, Roder & McDermott, 2018 [97] | Aboriginal and Torres Strait Islander people in Cape York and Torres Strait communities, Qld | Longitudinal study.
n=2,200 |
· The risk of developing a respiratory cancer after 15 years among those who smoked at baseline was nearly four-fold for Aboriginal people (HR 3.9, 95% CI 1.1-14, no p-values reported, n=1389) and for all participants combined (HR 3.7, 95%CI 1.7-8.0).
· Current smoking at baseline was associated with an increased risk of developing any cancer over 15 years (HR 1.6, 95%CI 1.1-2.0). · This risk was borne by Aboriginal participants (HR 2.3, 95%CI 1.3-4.0), rather than by Torres Strait Islander participants, who were at no increased risk from smoking (HR 0.9, 95%CI 0.6-1.5, n=811). · Similarly, results showed no increased risk for this subgroup for respiratory cancers, digestive cancers, or for all other cancers combined. |
· Short follow-up period for detecting cancers.
· Problems with the quality and completeness of hospital data. · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis. |
| Vulvar cancer and vulvar intraepithelial neoplasia (VIN – abnormal growth of cells with the potential to progress to cancer) | McWhirter et al., 2014 [249] | Aboriginal women in Arnhem Land | Case-control study
n=30 cases n=61 controls |
· There was no association between current smoking and vulvar cancer or VIN.
|
· Small sample.
· Problems with the quality and completeness of health clinic records. · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis. · Extremely high prevalence of smoking in the total sample (71%) may have obfuscated the association. |
| Type 2 diabetes | Burke et al., 2007 [250] | Aboriginal people in the Kimberley, WA | Longitudinal study
n=504 |
· People who were current smokers at baseline had twice the diabetes risk of ex- and never-smokers after 14 years (HR 2.15, 95%CI 1.23-3.39, p=0.006). | · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis.
· Death and hospital records used for ascertainment of diabetes. |
| Dementia | Smith et al., 2010 [54] | Aboriginal people aged over 45 years from the Kimberley, WA | Case-control study
n=328 |
· People with dementia had four-fold odds of being current smokers, compared to those without dementia (OR 4.5, 95%CI 1.1 – 18.6). | · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis.
· Brain imaging not used in ascertainment of dementia. |
| Hospitalisation for pelvic inflammatory disease (PID, a condition associated with long term infertility and an increased risk of ectopic pregnancy) | Li & McDermott, 2005 [251] | Aboriginal and Torres Strait Islander women in far North Queensland | Cross-sectional study
n=1,445 |
· Women hospitalised for PID were three times more likely to be current smokers than women without PID (OR 3.1, 95% CI 1.4-9.2, p value not reported). | · Problems with the quality and completeness of hospital records used for ascertainment of PID.
· Cross-sectional design limits causal inference. · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis. |
| Infertility | Kildea and Bowen, 2000 [252] | Aboriginal women in a small remote NT community | Retrospective cross-sectional study
n=342 |
· No association between current smoking and infertility. | · Former smokers, smoking duration, and smoking intensity not accounted for in the analysis.
· Problems with the quality and completeness of health clinic records used for ascertainment of fertility and smoking status · Extremely high prevalence of smoking in the total sample (76%) may have obfuscated the association. |
| Effects of smoking in pregnancy | |||||
| Small for gestational age (SGA), low birthweight and preterm birth | Chan et al., 2001 [253] | All Aboriginal women who had singleton births in SA in 1998-1999 | Retrospective cohort analysis
n=811 |
· Maternal smoking after 20 weeks gestation accounted for 48% of births where the baby was SGA, 25% of low birthweight babies and 20% of preterm births | · Self-reported smoking variable not validated |
| SGA, preterm births and perinatal deaths | Gibberd et al., 2019 [254] | All Aboriginal singleton babies born in Western Australia in 1998-2010 | Retrospective cohort analysis
n=28,119 |
· 28% of SGA, 9% of preterm births and 19% of perinatal deaths could be attributed to maternal smoking at any stage of gestation | |
| Mean birthweight z-score, SGA | Gibberd et al., 2019 [255] | Aboriginal singleton babies born in Western Australia in 1998-2010 | Retrospective cohort analysis with data linkage
n=8,113 |
· Maternal smoking was associated with a reduction in mean birthweight z-score (-0.39, 95% CI -0.45 – -0.34) and an increased risk of SGA (RR 1.89, 1.64-2.17).
· The effect of poor foetal growth of the mother on her own child’s birthweight and risk of SGA was very small in comparison to the effects of smoking in the current pregnancy. |
· Excluded babies whose mothers were born before 1980 or interstate or who did not link to a birth record. |
| Risk factors for SIDS (lower birthweight, younger gestational age at delivery) and maternal blood inflammatory markers | Pringle et al., 2015 [256] | Aboriginal and Torres Strait Islander mothers in NSW | Longitudinal cohort study
n=131 |
· There was a direct relationship between higher levels of maternal serum cotinine levels (a marker of smoke exposure from first- and second-hand smoking) and lower birthweight (correlation coefficient -0.37, p<0.001) and lower gestational age at delivery (-0.199, p=0.023).
· Higher cotinine levels were associated with higher levels of inflammatory markers in the blood of the mother. |
· Small sample
|
| Hospitalisation for respiratory syncytial virus (RSV) infection (bronchiolitis and pneumonia) | Homaira et al., 2016 [257] | Aboriginal and Torres Strait Islander children aged under 2 years in NSW | Retrospective cohort analysis
n=26,523 |
· Children exposed to maternal smoking in pregnancy had a 42% increased risk of hospitalisation for infection with RSV (HR 1.42, 95% CI 1.23 to 1.65).
· Around 17% of admissions for RSV could be attributed to maternal smoking. |
· Problems with the quality and completeness of hospital records used for ascertainment of RSV infection.
· Did not include data on household exposure to smoking, or maternal smoking after pregnancy. |
| Body mass index (BMI) z-score (an indicator of chronic disease risk | Thurber et al., 2015 [258] | Aboriginal and Torres Strait Islander children aged 3 to 9 years (national sample) | Longitudinal cohort study
n=1,264 |
· Children whose mothers smoked during pregnancy had a 0.25 unit increase in body mass index z-score compared to those whose mothers did not smoke. | · Birthweight data obtained via carer recall rather than clinical records for 19% of children. |
| Kidney injury (high urine neutrophils gelatinase-associated lipocalin levels) | Sutherland et al, 2019 [259]
|
Aboriginal and Torres Strait Islander infants born at 24-36 weeks gestation | Cross-sectional
n=60 |
· Kidney injury was associated with maternal smoking.
· [seek full-text for details] |
· Small sample |
| Perinatal death, preterm birth, small for gestational age (SGA), transfer to another hospital | McInerney et al., 2019
[77] |
Singleton babies born to Aboriginal mothers in NSW between 2010 and 2014 | Retrospective cohort study
n=18,154 |
· Babies born to mothers who did not smoke during pregnancy had a substantially lower risk of perinatal death (RR=0.58, 95% CI 0.44 to 0.76), preterm birth (RR=0.58, 95% CI 0.53 to 0.64), SGA (RR=0.35, 95% CI 0.32 to 0.39) and transfer to another hospital (RR=0.76, 95% CI 0.66 to 0.89).
· Around 27% of perinatal deaths, 26% of preterm births and 48% of SGA could be attributed to smoking in pregnancy |
· The effect of smoking intensity and exposure to second-hand smoker were not assessed. |
| Effects of second-hand smoke | |||||
| Re-admission to hospital for respiratory condition | McCallum et al., 2015 [260] | Aboriginal and Torres Strait Islander infants admitted to Royal Darwin Hospital for bronchiolitis | Longitudinal cohort study with 6-month follow-up
n=232 |
· Exposure to household smoke more than doubled the odds of readmission for any respiratory illness within six months (OR 2.6, 95%CI 1.0, 6.3, p=0.04). | · Study excluded infants with chronic lung or cardiac disease and infants who did not require intensive care.
· Exposure to second-hand smoke measured by interview response rather than urine cotinine levels. |
| Acute middle ear infection, otitis media with effusion (glue ear), or eardrum perforation with or without discharge | Jacoby et al., 2008 [261] | Aboriginal children born in Kalgoorlie hospital | Prospective cohort study with 2-year follow-up
n=82 |
· The odds of developing middle ear disease before the age of 2 years was more than trebled for children exposed to indoor and outdoor tobacco smoke (OR 3.54; 95% CI, 1.68–7.47). | · Small sample
· Exposure to second-hand smoke measured by interview response rather than urine cotinine levels. |
Notes:
Studies that only compared outcomes for Aboriginal and Torres Strait Islander peoples with non-Indigenous Australians are not included in this table.
*n=number of participants included in the study
RR – Risk ratio
HR – Hazard ratio
OR – odds ratio
CI – confidence interval
Appendix 3: Literature search strategy
We conducted a literature search in ANU SuperSearch, an all-in-one academic search engine that includes over 900 sources, including the following key databases for this review:
- Applied Social Sciences Indexes and Abstracts (ASSIA)
- Informit Online
- JSTOR
- Medline
- ProQuest
- PubMed
- ScienceDirect
- Scopus
- Taylor and Francis Online
- Web of Science
- Wiley Online Library
Search terms: ((smok* OR tobacco OR cigarette* OR “second-hand smoke” OR nicotine) AND (Aborig* OR “Torres Strait Islander” OR Indigenous OR “First Nation*”) AND Australia).
Filtered to include: articles from 2009-present, peer-review, full text online.
Filtered to exclude: Book/ebook, Book chapter, Book review, conference preceding, magazine article, trade publication article.
We also included relevant articles from the HealthInfoNet EndNote library, and grey literature, focusing on national tobacco policies and programs.
This was not a systematic literature review in that not all articles were synthesized or assessed in the review. Rather, it was a scoping review, whereby the articles collected were used as the basis of the review, with further information sought during the drafting process, where required.
Figure 6: Literature review process
Table 4: Data sources
| Data source | Year | Representative | Method | Sample size | Age range (years) |
| National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) [262] | 2004–05
|
Yes
|
· Nationally representative sample of Aboriginal and Torres Strait Islander households in remote and non-remote areas
· Used a standardised ABS sampling method which has been used across household surveys1 · Developed in conjunction with an advisory group that included people with expertise in Indigenous information, research and health issues. Members worked relevant Aboriginal and Torres Strait Islander Organisations and institutions including health services and peak information bodies, government agencies, or academic research institutions. |
10,439 | ≥ 15 |
| Aboriginal and Torres Strait Islander health survey (ATSIHS) [2, 263, 264] | 2012–13 | Yes | · Information collected from three Aboriginal and Torres Strait Islander surveys: The National Aboriginal and Torres Strait Islander health survey (NATSIHS); the National Aboriginal and Torres Strait Islander nutrition and physical activity survey (NATSINPAS); and the National Aboriginal and Torres Strait Islander health measures survey (NATSIHMS).
· Used a standardised ABS sampling method which has been used across household surveys i. |
~13,300 | ≥ 15 |
| 2018–19 | 10,579 | ≥ 15 | |||
| National Aboriginal and Torres Strait Islander Social Survey (NATSISS) [127, 265, 266] | 2002 | Yes | · Interviews were conducted with Aboriginal and Torres Strait Islander peoples using a standardised ABS sampling method i.
· 2008 – Information on substance use was collected by self-administered forms in non-remote areas and asked by interviewers in remote locations. |
9,400 | ≥ 15 |
| 2008 | Yes | 12,947 | ≥ 15 | ||
| 2014–15
|
Yes
|
11,178
|
≥ 15 | ||
| Talking about the Smokes (TATS study) [267]
|
Baseline 2012–13 Follow-up
2013–14 |
Yes | · Participants were selected through a quota sampling design, based on meaningful clusters. 40 quotas or sites were collected from 35 clusters or Aboriginal community controlled health services (ACCHS), to represent national population distribution (based on 2006 Census) across three remoteness categories major cities, inner and outer regional, remote and very remote. One of the clusters was in the Torres Strait where there are no ACCHS.
· Sampling method was different at each location with the local ACCHS having input into the method used, with the study team aiming to have a sample of 50 smokers, and 25 non-smokers from each of the 40 sites. · Three surveys were used: a survey for community members, an ACCHS staff survey and a policy survey for ACCHS. Community surveys were conducted face-to-face and ACCHS survey were self-reported. · A follow-up survey was completed with half the eligible smokers and ex-smokers. |
2,522 community members
645 ACCHS staff members |
18 – ≥55
|
| National Drug Strategy Household Survey (NDSHS) [56] | 2016 | Yes | · A technical advisory group was set up to support the administration of the survey with experts in tobacco, alcohol, and other drug research and data collection.
· The sample was selected using stratified, multistage random sampling with 15 strata’s broken down by state and then by capital cities within each state excluding the ACT which was one strata. · Sample was based on households, so people who were homeless or institutionalised were not included in the survey. · Participants competed the survey via paper, online or telephone interview. |
23,772 | ≥ 12 |
| National Perinatal data collection (NPDC) [46, 268]
|
Ongoing | Whole of population | · The NPDC has collected data on pregnancy, childbirth and moths since 1991 and is an administrative data set.
· National population-based cross-sectional collection of data on pregnancy and childbirth. Births are reported to the perinatal data collection. · Collected by a midwife or birth attendant on antenatal care, the care provided during labour, and the delivery and care provided after the birth. · Standardised de-identified state-level data is provided to the Australian Institute of Health and Welfare annually to be incorporated into different reports. · Includes all babies born in a hospital, birth centres and community. |
More than 300,000 babies are born every year added onto the register. | N/A |
Note: 1. Households included in ABS household surveys including the NATTSIHS, ATSIHS & NATSISS, were selected using similar sample design based on the most recent census data. Torres Strait Islander population was over sampled to have meaningful data. Residents living in private dwellings over the age of 15 were interviewed by ABS Staff with consent needed to interview persons aged 15–17 years. One person over the age of 18 years was asked to provide demographic and economic information about the household. Data was also collected on children living within the residence by their parents or those responsible for the child. This is a limited population sample as only includes people whose usual place of residence is a private dwelling such as a house, flat or unit at the time of survey. People who live in short stay accommodation such as hotels, hostels, caravan parks, hospitals, prisons or nursing homes are not included in the sample.
References
- Lovett, R., Thurber, K. A., Wright, A., Maddox, R., & Banks, E. (2017). Deadly progress: changes in Australian Aboriginal and Torres Strait Islander adult daily smoking, 2004-2015. Public Health Research & Practice, 27(5). Retrieved from: https://doi.org/10.17061/phrp2751742
- Australian Bureau of Statistics. (2019). National Aboriginal and Torres Strait Islander Health Survey, 2018-19. Canberra: Australian Bureau of Statistics.
- Thomas, D. P. (2009). Smoking prevalence trends in Indigenous Australians, 1994-2004: a typical rather than an exceptional epidemic. International Journal for Equity in Health, 8(37), 1-21.
- Fogarty, W., Lovell, M., Langenberg, J., & Heron, M.-J. (2018). Deficit discourse and strengths-based approaches: changing the narrative of Aboriginal and Torres Strait Islander health and wellbeing. Canberra: National Centre for Indigenous Studies, Australian National University and Lowitja Institute.
- Fforde, C., Bamblett, L., Lovett, R., Gorringe, S., & Fogarty, B. (2013). Discourse, deficit and identity: Aboriginality, the race paradigm and the language of representation in contemporary Australia. Media International Australia, 149, 162-173.
- Axelsson, P., Kukutai, T., & Kippen, R. (2016). The field of Indigenous health and the role of colonisation and history. Journal of Population Research, 33(1), 1-7.
- Sherwood, J. (2013). Colonisation – it’s bad for your health: the context of Aboriginal health. Contemporary Nurse, 46(1), 28-40.
- Paradies, Y. (2016). Colonisation, racism and Indigenous health. Journal of Population Research, 33(1), 83–96.
- Morton Ninomiya, M. E., Hurley, N., & Penashue, J. (2020). A decolonizing method of inquiry: using institutional ethnography to facilitate community-based research and knowledge translation. Critical Public Health, 30(2), 220-231.
- United Nations. (2007). United Nations declaration on the rights of Indigenous peoples. Geneva: United Nations.
- World Health Organization. (2003). World Health Organization Framework Convention on Tobacco Control. Geneva, Switzerland: World Health Organization.
- National Health and Medical Research Council. (2018). Ethical conduct in research with Aboriginal and Torres Strait Islander peoples and communities: guidelines for researchers and stakeholders. Canberra: National Health and Medical Research Council.
- National Health and Medical Research Council. (2018). Keeping research on track II: a companion document to Ethical conduct in research with Aboriginal and Torres Strait Islander peoples and communities: guidelines for researchers and stakeholders. Canberra: National Health and Medical Research Council.
- Johnston, V., & Thomas, D. P. (2008). Smoking behaviours in a remote Australian Indigenous community: the influence of family and other factors. Social Science & Medicine, 67(11), 1708-1716.
- Benowitz, N. L. (2010). Nicotine addiction. New England Journal of Medicine, 362(24), 2295-2303.
- Australian Bureau of Statistics. (2015). National Health Survey: first results, Australia, 2014-15 (ABS Cat. no. 4364.0.55.001). Canberra: Australian Bureau of Statistics.
- Öberg, M., Jaakkola, M. S., Prüss-Üstün, A., Schweizer, C., & Woodward, A. (2010). Second hand smoke: assessing the burden of disease at national and local levels (Environmental burden of disease series no. 18). Geneva, Switzerland: World Health Organization.
- Schick, S., & Glantz, S. A. (2013). Sidestream cigarette smoke toxicity increases with aging and exposure duration. Tobacco Control, 15(6), 424-428.
- Scollo, M. M., & Winstanley, M. H. (2019). Tobacco in Australia: facts and issues. Retrieved July 2019 from https://www.tobaccoinaustralia.org.au/
- Ratsch, A. M., Steadman, K. J., & Bogossian, F. (2010). The pituri story: a review of the historical literature surrounding traditional Australian Aboriginal use of nicotine in Central Australia. Journal of Ethnobiology and Ethnomedicine, 6. Retrieved from: https://doi.org/10.1186/1746-4269-6-26
- Ratsch, A. M., Mason, A., Rive, L., Bogossian, F. E., & Steadman, K. J. (2017). The Pituri Learning Circle: central Australian Aboriginal women’s knowledge and practices around the use of Nicotiana spp. as a chewing tobacco. Rural and Remote Health, 17. Retrieved from: https://doi.org/10.22605/RRH4044
- Ratsch, A., Steadman, K., Ryu, B., & Bogossian, F. (2019). Tobacco and pituri use in pregnancy: a protocol for measuring maternal and perinatal exposure and outcomes in Central Australian Aboriginal women. Methods and Protocols, 2(2). Retrieved from: https://doi.org/10.3390/mps2020047
- Australian Government Department of Health. (2020). About e-cigarettes. Retrieved 29 January 2020 from https://www.health.gov.au/health-topics/smoking-and-tobacco/about-smoking-and-tobacco/about-e-cigarettes
- Australian Bureau of Statistics. (2019). Estimates and projections, Aboriginal and Torres Strait Islander Australians, 2006 to 2031. Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2018). Estimates of Aboriginal and Torres Strait Islander Australians, June 2016. Retrieved 31 August 2018 from https://www.abs.gov.au/ausstats/abs@.nsf/mf/3238.0.55.001
- Australian Bureau of Statistics. (2019). Australian demographic statistics, June 2019. from https://www.abs.gov.au/ausstats/abs%40.nsf/mediareleasesbyCatalogue/CA1999BAEAA1A86ACA25765100098A47?OpenDocument
- Brady, M. (2002). Health Inequalities: Historical and cultural roots of tobacco use among Aboriginal and Torres Strait Islander people. Australian and New Zealand Journal of Public Health, 26(2), 120-124.
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2016). History of tobacco use among Aboriginal peoples and Torres Strait Islanders Tobacco in Australia: facts and issues. Melbourne: Cancer Council Victoria.
- McNiven, I. J. (2008). Inclusions, exclusions and transitions: Torres Strait Islander constructed landscapes over the past 4000 years, northeast Australia. The Holocene, 18(3), 449-462.
- Briggs, D., Lindorff, K., & Ivers, R. (2003). Aboriginal and Torres Strait Islander Australians and tobacco. Tobacco Control, 12(suppl.), ii5-ii8.
- Passey, M. E., Gale, J. T., & Sanson-Fisher, R. W. (2011). “Its almost expected”: rural Australian Aboriginal women’s reflections on smoking initiation and maintenance: a qualitative study. BMC Women’s Health, 11. Retrieved from: https://doi.org/10.1186/1472-6874-11-55
- Waa, A., Robson, B., Gifford, H., Smylie, J., Reading, J., Henderson, J. A., . . . Calma, T. (2019). Foundation for a smoke-free world and healthy Indigenous futures: an oxymoron? Tobacco Control, 29(2), 237-240.
- Brady , M., & Long, J. (2003). Mutual exploitation?: Aboriginal Australian encounters with Europeans, Southeast Asians, and tobacco. In W. Jankowiak & D. Bradburd (Eds.), Drugs, labor and colonial expansion (pp. 31-58). Tucson: University of Arizona Press.
- Stretton, W. G. (1914). Northern Territory of Australia: report of the administrator for the year 1913. Melbourne: Government Printer for the State of Victoria.
- Dawson, A. P., Cargo, M., Stewart, H., Chong, A., & Daniel, M. (2012). ‘I know it’s bad for me and yet I do it’: exploring the factors that perpetuate smoking in Aboriginal health workers – a qualitative study. BMC Health Services Research, 12. Retrieved from: https://doi.org/10.1186/1472-6963-12-102
- Blyton, G. (2010). Smoking Kills: the introduction of tobacco smoking into Aboriginal society with a particular focus on the Hunter Region of Central Eastern New South Wales from 1800 to 1850. International Journal of Critical Indigenous Studies, 3(2), 2-10.
- Ivers, R. G. (2002). Tobacco addiction and the process of colonisation [letter]. Australian and New Zealand Journal of Public Health, 26(3), 280-281.
- Chewings, C. (1936). Back in the stone age: the natives of Central Australia. Sydney: Angus & Robertson.
- Lovett, R., Thurber, K. A., & Maddox, R. (2017). The Aboriginal and Torres Strait Islander smoking epidemic: what stage are we at, and what does it mean? Public Health Research & Practice, 27(4). Retrieved from: https://doi.org/10.17061/phrp2741733
- National Center for Chronic Disease Prevention and Health Promotion United States. (2014). The health consequences of smoking- 50 years of progress: a report of the Surgeon General. Atlanta, United States of America: National Center for Chronic Disease Prevention and Health Promotion United States.
- Australian Institute of Health and Welfare (AIHW). (2016). Tobacco indicators: measuring midpoint progress: reporting under the National Tobacco Strategy 2012-2018. Canberra: Australian Institute of Health and Welfare (AIHW).
- Intergovernmental Committee on Drugs. (2012). National tobacco strategy 2012-2018. Canberra: National Drug Strategy.
- Australian Bureau of Statistics. (2017). Aboriginal and Torres Strait Islander peoples: smoking trends, Australia, 1994 to 2014-15. Retrieved 19 October 2017 from https://www.abs.gov.au/ausstats/abs@.nsf/mf/4737.0?OpenDocument
- Maddox, R., Thurber, K. A., Banks, E., Calma, T., & Lovett, R. (2020 in progress). Deadly news: Further reductions in Aboriginal and Torres Strait Islander smoking, 2004-2018/19.
- Heris, C. L., Eades, S. J., Lyons, L., Chamberlain, C., & Thomas, D. P. (2019). Changes in the age young Aboriginal and Torres Strait Islander people start smoking, 2002–2015. Public Health Research and Practice, Early view(https://doi.org/10.17061/phrp29121906).
- Australian Institute of Health and Welfare. (2019). Australia’s mothers and babies 2017 – in brief (Perinatal statistics series no. 35. Cat. no. PER 100). Canberra: Australian Institute of Health and Welfare.
- Eades, S. J., Sanson-Fisher, R. W., Wenitong, M., Panaretto, K., D’Este, C., Gilligan, C., & Stewart, J. (2012). An intensive smoking intervention for pregnant Aboriginal and Torres Strait Islander women: a randomised controlled trial. Medical Journal of Australia, 197(1), 42-46.
- Bovill, M., Bar-Zeev, Y., Bonevski, B., Gruppetta, M., Oldmeadow, C., Hall, A., . . . ICAN QUIT in Pregnancy Pilot Group. (2020). Aboriginal Wingadhan Birrang (woman’s journey) of smoking cessation during pregnancy as they participate in the ICAN QUIT in pregnancy pilot step-wedge trial. Women and Birth, 33(3), 300-308.
- Australian Bureau of Statistics. (2016). National Aboriginal and Torres Strait Islander Social Survey, 2014-15. Canberra: Australian Bureau of Statistics.
- Gould, G. S., Munn, J., Avuri, S., Hoff, S., Cadet-James, Y., McEwen, A., & Clough, A. R. (2013). “Nobody smokes in the house if there’s a new baby in it”: Aboriginal perspectives on tobacco smoking in pregnancy and in the household in regional NSW Australia. Women and Birth, 26(4), 246–253.
- Knott, V. E., Gilligan, G., Maksimovic, L., Shen, D., & Murphy, M. (2016). Gender determinants of smoking practice in Indigenous communities: an exploratory study. European Journal of Cancer Care, 25(2), 231-241.
- Glover, M., Kira, A., Johnston, V., Walker, N., Brown, N., & Thomas, D. (2015). Australian and New Zealand Indigenous mothers’ report respect for smoking bans in homes. Women and Birth, 28(1), 1-7.
- Thomas, D. (2015). Talking About The Smokes. Medical Journal of Australia, 202 Supplement(10).
- Smith, K., Flicker, L., Dwyer, A., Atkinson, D., Almeida, O. P., Lautenschlager, N. T., & LoGiudice, D. (2010). Factors associated with dementia in Aboriginal Australians. Australian and New Zealand Journal of Psychiatry, 44(10), 888–893.
- Thomas, D. P., Lusis, N., van der Sterren, A. E., & Borland, R. (2019). Electronic cigarette use and understanding among a national sample of Australian Aboriginal and Torres Islander smokers. Nicotine & Tobacco Research, 21(10), 1434-1440.
- Australian Institute of Health and Welfare. (2017). National Drug Strategy Household Survey 2016: detailed findings. Canberra: Australian Institute of Health and Welfare.
- Hartmann-Boyce, J., McRobbie, H., Bullen, C., Begh, R., Stead, L. F., & Hajek, P. (2016). Can electronic cigarettes help people stop smoking, and are they safe to use for this purpose? Cochrane Database of Systematic Reviews, (9). Retrieved from: https://www.cochrane.org/CD010216/TOBACCO_can-electronic-cigarettes-help-people-stop-smoking-and-are-they-safe-use-purpose
- Walker, N., Parag, V., Verbiest, M., Laking, G., Laugesen, M., & Bullen, C. (2020). Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. The Lancet Respiratory Medicine, 8(1), 54-64.
- Cancer Australia. (2018). Statement on e-cigarettes in Australia. Canberra: Cancer Australia.
- World Health Organization. (2017). Statement on electronic nicotine delivery systems and electronic non-nicotine delivery systems (ENDS/ENNDS). Geneva, Switzerland: World Health Organization.
- Australian Institute of Health and Welfare. (2016). Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011 (Australian Burden of Disease Study series no. 6, Cat no. BOD 7). Canberra: Australian Institute of Health and Welfare.
- Filion, K. B., & Luepker, R. V. (2013). Cigarette smoking and cardiovascular disease: lessons from Framingham. Global Heart, 8(1), 35-41.
- Centers for Disease Control and Prevention. (2010). How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. Atlanta, United States of America: Centers for Disease Control and Prevention.
- Xie, X. T., Liu, Q., Wu, J., & Wakui, M. (2009). Impact of cigarette smoking in type 2 diabetes development. Acta Pharmacologica Sinica, 30, 784–787.
- Zhu, P., Pan, X., Sheng, L., Chen, H., & Pan, A. (2017). Cigarette smoking, diabetes, and diabetes complications: Call for urgent action. Current Diabetes Reports, 17(9), 78.
- Pan, A., Wang, Y., Talaei, M., & Hu, F. B. (2015). Relation of smoking with total mortality and cardiovascular events among patients with diabetes mellitus: a meta-analysis and systematic review. Circulation, 132(19), 1795–1804.
- Zhang, K., & Wang, X. (2013). Maternal smoking and increased risk of sudden infant death syndrome: a meta-analysis. Legal Medicine, 15(3), 115-121.
- Rayfield, S., & Plugge, E. (2017). Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity. Journal of Epidemiology and Community Health, 71(2), 162-173.
- Montgomery, S. M., & Ekbom, A. (2002). Smoking during pregnancy and diabetes mellitus in a British longitudinal birth cohort. British Medical Journal, 324, 26-27.
- Jayes, L., Haslam, P. L., Gratziou, C. G., Powell, P., Britton, J., Vardavas, C., . . . De Grada Orive, J. I. (2016). SmokeHaz: systematic reviews and meta-analyses of the effects of smoking on respiratory health. Chest, 150(1), 164-179.
- He, Y., Chen, J., Zhu, L. H., Hua, L. L., & Ke, F. F. (2017). Maternal smoking during pregnancy and ADHD: results from a systematic review and meta-analysis of prospective cohort studies. Journal of Attention Disorders, Early view(https://doi.org/10.1177/1087054717696766).
- Shah, N. R., & Bracken, M. B. (2000). A systematic review and meta-analysis of prospective studies on the association between maternal cigarette smoking and preterm delivery. American Journal of Obstetrics and Gynecology, 182(2), 465-472.
- da Silva Pereira, P., Da Mata, F., Godoy Figueiredo, A. C., Cordeiro de Andrade, K. R., & Pereira, M. G. (2017). Maternal active smoking during pregnancy and low birth weight in the Americas: a systematic review and meta-analysis. Nicotine & Tobacco Research, 19(5), 497–505.
- Marufu, T. C., Ahankari, A., Coleman, T., & Lewis, S. (2015). Maternal smoking and the risk of still birth: systematic review and meta-analysis. BMC Public Health, 15. Retrieved from: https://doi.org/10.1186/s12889-015-1552-5
- Pineles, B. P., Hsu, S., Park, E., & Samet, J. M. (2016). Systematic review and meta-analyses of perinatal death and maternal exposure to tobacco smoke during pregnancy. American Journal of Epidemiology, 184(2), 87–97.
- Xuan, Z., Zhongpeng, Y., Yanjun, G., Jiaqi, D., Yuchi, Z., Bing, S., & Chenghao, L. (2016). Maternal active smoking and risk of oral clefts: a meta-analysis. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 122(6), 680-690.
- McInerney, C., Ibiebele, I., Ford, J. B., Randall, D., Morris, J. M., Meharg, D., . . . Torvaldsen, S. (2019). Benefits of not smoking during pregnancy for Australian Aboriginal and Torres Strait Islander women and their babies: a retrospective cohort study using linked data. BMJ Open, 9(11). Retrieved from: https://doi.org/10.1136/bmjopen-2019-032763
- Moon, R. Y., & Task Force on Sudden Infant Death Syndrome. (2016). SIDS and other sleep-related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics, 138(5). Retrieved from: https://doi.org/10.1542/peds.2016-2940
- Fischer, F., & Kraemer, A. (2015). Meta-analysis of the association between second-hand smoke exposure and ischaemic heart diseases, COPD and stroke. BMC Public Health, 15. Retrieved from: https://doi.org/10.1186/s12889-015-2489-4
- Cao, S., Yang, C., Gan, Y., & Lu, Z. (2015). The health effects of passive smoking: an overview of systematic reviews based on observational epidemiological evidence. PLOS ONE, 10(10). Retrieved from: https://doi.org/10.1371/journal.pone.0139907
- Mahid, S. S., Minor, K. S., Soto, R. E., Hornung, C. A., & Galandiuk, S. (2006). Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clinic Proceedings, 81(11), 1462-1471.
- Okoli, C. T. C., & Kodet, J. (2015). A systematic review of secondhand tobacco smoke exposure and smoking behaviors: smoking status, susceptibility, initiation, dependence, and cessation. Addictive Behaviors, 47, 22-32.
- Northrup, T. F., Jacob, P., Benowitz, N. L., Hoh, E., Quintana, P. J. E., Hovell, M. F., . . . Stotts, A. L. (2016). Thirdhand smoke: state of the science and a call for policy expansion. Public Health Reports, 131(2), 233-238.
- Acuff, L., Fristoe, K., Hamblen, J., Smith, M., & Chen, J. (2016). Third-hand smoke: old smoke, new concerns. Journal of Community Health, 41(3), 680-687.
- Moghbel, N., Ryu, B., Cabot, P. J., Ratsch, A., & Steadman, K. J. (2016). In vitro cytotoxicity of Nicotiana gossei leaves, used in the Australian Aboriginal smokeless tobacco known as pituri or mingkulpa. Toxicology Letters, 254(July 2016), 45-51.
- International Agency for Research on Cancer. (2012). Personal habits and indoor combustions: volume 100 E: a review of human carcinogens. Lyon, France: International Agency for Research on Cancer.
- Inamdar, A. S., Croucher, R. E., Chokhandre, M. K., Mashyakhy, M. H., & Marinho, V. C. C. (2015). Maternal smokeless tobacco use in pregnancy and adverse health outcomes in newborns: a systematic review. Nicotine & Tobacco Research, 17(9), 1058–1066.
- Suliankatchi, R. A., & Sinha, D. N. (2016). The human cost of tobacco chewing among pregnant women in India: a systematic review and meta-analysis. The Journal of Obstetrics and Gynecology of India, 66(Suppl 1), 161-166.
- Liska, S. R. (2013). In utero exposure to Black Bull chewing tobacco and neonatal nicotine withdrawal: a review of the literature. Neonatal Network, 33(1).
- Gould, G. S., Bar Zeev, Y., Tywman, L., Oldmeadow, C., Chiu, S., Clarke, M., & Bonevski, B. (2017). Do clinicians ask pregnant women about exposures to tobacco and cannabis smoking, second-hand-smoke and e-cigarettes? An Australian national cross-sectional survey. International Journal of Environmental Research and Public Health, 14(12). Retrieved from: https://doi.org/10.3390/ijerph14121585
- Cancer Council Australia. (2019). Independent experts back stronger government stance on e-cigarette threat. from https://www.cancer.org.au/news/media-releases/independent-experts-back-stronger-government-stance-on-e-cigarette-threat.html
- The Thoracic Society of Australia and New Zealand, & Lung Foundation Australia. (2017). Inquiry into the use of electronic cigarettes and personal vaporisers in Australia. Sydney: The Thoracic Society of Australia and New Zealand.
- Leventhal, A. M., Strong, D. R., & Kirkpatrick, M. G. (2015). Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. Journal of the American Medical Association, 314(7), 700-707.
- Soneji, S., Barrington-Trimis, J. L., & Wills, T. A. (2017). Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults. JAMA Pediatrics, 171(8), 788-797.
- National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health. (2020). Outbreak of lung injury associated with the use of e-cigarette, or vaping, products. Retrieved 25 February 2020 from https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html
- World Health Organization. (2019). Metrics: Disability-Adjusted Life Year (DALY). from https://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/
- Li, M., Roder, D., & McDermott, R. (2018). Diabetes and smoking as predictors of cancer in Indigenous adults from rural and remote communities of North Queensland – a 15-year follow up study. International Journal of Cancer, 143(5), 1054-1061.
- Australian Institute of Health and Welfare. (2011). Substance use among Aboriginal and Torres Strait Islander people (AIHW Catalogue No IHW 40). Canberra: Australian Institute of Health and Welfare.
- Begg, S., Vos, T., Barker, B., Stevenson, C., Stanley, L., & Lopez, A. (2007). The burden of disease and injury in Australia 2003 (AIHW cat. no. PHE 82). Canberra: Australian Institute of Health and Welfare.
- Whetton, S., Tait, R. J., Scollo, M., Banks E. , Chapman, J., Dey, T., . . . Allsop, S. (2019). Identifying the social costs of tobacco use to Australia in 2015/16. Perth: National Drug Research Institute.
- Unwin, C. E., Thomson, N. J., & Gracey, M. S. (1995). The impact of tobacco smoking and alcohol consumption on Aboriginal mortality in Western Australia. Medical Journal of Australia, 162(9), 475-478.
- Measey, M. A. L., d’Espaignet, E. T., & Cunningham, J. (1998). Adult morbidity and mortality due to tobacco smoking in the Northern Territory 1986–1995. Darwin: Northern Territory Department of Health and Community Services.
- Arnold-Reed, D., D’Arcy, C., Holman, C., Coode, J., & Unwin, E. (1998). Effects of smoking and unsafe alcohol consumption on Aboriginal life expectancy [letter]. Medical Journal of Australia, 168(2), 95.
- Thurber, K., Banks, E., Joshy, G., Calma, T., Eades, S., & Lovett, R. (2019, October 2019). Tobacco smoking and all-cause mortality among 1,464 Aboriginal adults in the 45 and Up Study, New South Wales. Paper presented at the Oceania Tobacco Control Conference, Sydney.
- Wynne-Jones, M., Hillin, A., Byers, D., Stanley, D., Edwige, V., & Brideson, T. (2016). Aboriginal grief and loss: a review of the literature. Australian Indigenous HealthBulletin, 16(3). Retrieved from: http://healthbulletin.org.au/articles/aboriginal-grief-and-loss-a-review-of-the-literature
- Sobott, G., & Munro, J. (2015). An interview with Jenny Munro. from https://gaelesobott.wordpress.com/2015/01/25/an-interview-with-jenny-munro/
- Warburton, J., & Chambers, B. (2007). Older Indigenous Australians: their integral role in culture and community. Australasian Journal on Ageing, 26(1), 3-7.
- Askew, D. A., Guy, J., Lyall, V., Egert, S., Rogers, L., Pokino, L., . . . Schluter, P. J. (2019). A mixed methods exploratory study tackling smoking during pregnancy in an urban Aboriginal and Torres Strait Islander primary health care service. BMC Public Health, 19. Retrieved from: https://doi.org/10.1186/s12889-019-6660-1
- Heath, F., Bor, W., Thompson, J., & Cox, L. (2011). Diversity, disruption, continuity: parenting and social and emotional wellbeing amongst Aboriginal peoples and Torres Strait Islanders. Australian and New Zealand Journal of Family Therapy, 32(4), 300-313.
- Winstanley, M., Freeman, B., Bayly, M., & Scollo, M. (2018). The tobacco industry in Australian society. In E. M. Greenhalgh, M. M. Scollo & M. H. Winstanley (Eds.), Tobacco in Australia: facts and issues. Melbourne: Cancer Council Victoria.
- Euromonitor International. (2019). Tobacco in Australia. from https://www.euromonitor.com/tobacco-in-australia/report
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., & Winstanley, M. H. (2016). The tobacco industry and Indigenous communities. In E. M. Greenhalgh, M. M. Scollo & M. H. Winstanley (Eds.), Tobacco in Australia: facts and issues. Melbourne: Cancer Council Victoria.
- Thomas, D. P., & Bond, L. (2012). The tobacco industry and Aboriginal and Torres Strait Islander people. Medical Journal of Australia, 197(1), 24-26.
- Daube, M., Moodie, R., & McKee, M. (2017). Towards a smoke-free world? Philip Morris International’s new Foundation is not credible. The Lancet, 390(10104), 1722-1724.
- Hutcheon, S., & Bogle, A. (2019). Smoke and mirrors: the nanny state critics behind the vape debate,
- Foundation for a Smoke Free World. (2019). Our vision – Foundation for a Smoke Free World. from https://www.smokefreeworld.org/our-vision/
- British American Tobacco. (2019). Corporate social investment: helping to make a difference. from https://www.bat.com/csi#
- van der Eijk, Y., Bero, L. A., & Malone, R. E. (2018). Philip Morris International-funded ‘Foundation for a Smoke-Free World’: analysing its claims of independence. Tobacco Control, 28(6), 712-718.
- Czyzewski, K. (2011). Colonialism as a broader social determinant of health. International Indigenous Policy Journal, 2(1). Retrieved from: https://ir.lib.uwo.ca/iipj/vol2/iss1/5/
- Griffiths, K., Coleman, C., Lee, V., & Madden, R. (2016). How colonisation determines social justice and Indigenous health – a review of the literature. Journal of Population Research, 33(1), 9–30.
- Heris, C. L., Chamberlain, C., Gubhaju, L., Thomas, D. P., & Eades, S. J. (2019). Factors influencing smoking among Indigenous adolescents aged 10-24 years living in Australia, New Zealand, Canada, and the United States: a systematic review. Nicotine & Tobacco Research, Early view(https://doi.org/10.1093/ntr/ntz219).
- Australian Institute of Health and Welfare. (2018). Aboriginal and Torres Strait Islander Stolen Generations and descendants: numbers, demographic characteristics and selected outcomes. Canberra: Australian Institute of Health and Welfare.
- Tsourtos, G., Ward, P. R., Lawn, S., Winefield, A. H., Hersh, D., & Coveney, J. (2015). Is resilience relevant to smoking abstinence for Indigenous Australians? Health Promotion International, 30(1), 64-76.
- Australian Bureau of Statistics. (2010). The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples, 2010 (ABS Catalogue no 4704.0). Canberra: Australian Bureau of Statistics.
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2019). Prevalence of tobacco use among Aboriginal peoples and Torres Strait Islanders Tobacco in Australia: facts and issues (4 ed.). Melbourne: The Cancer Council.
- Kirk, L., Thurber, K., Welsh, J., Soga, K., Eades, S., Banks, E., & Lovett, R. (2019). Tobacco smoking and sociodemographic factors, health behaviours, and health status among older Indigenous and non-Indigenous adults in New South Wales, Australia, San Francisco, United States of America.
- Australian Bureau of Statistics. (2016). National Aboriginal and Torres Strait Islander Social Survey, 2014-15: Aboriginal and Torres Strait Islander people with a mental health condition. Retrieved 28 April 2016 from http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4714.0~2014-15~Feature%20Article~Aboriginal%20and%20Torres%20Strait%20Islander%20people%20with%20a%20mental%20health%20condition%20(Feature%20Article)~10
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2016). Smoking among Aboriginal and Torres Strait Islander children and teenagers Tobacco in Australia: facts and issues. Melbourne: Cancer Council Victoria.
- Greenhalgh, E. M., Stillman, S., Ford, C., Scollo, M. M., & Winstanley, M. H. (2018). Smoking and mental health Tobacco in Australia: facts & issues. Melbourne: Cancer Council Victoria.
- Priest, N., Paradies, Y., Stewart, P., & Luke, J. (2011). Racism and health among urban Aboriginal young people. BMC Public Health, 11. Retrieved from: https://doi.org/10.1186/1471-2458-11-568
- Cave, L., Cooper, M. N., Zubrick, S. R., & Shepherd, C. C. J. (2019). Caregiver-perceived racial discrimination is associated with diverse mental health outcomes in Aboriginal and Torres Strait Islander children aged 7–12 years. International Journal for Equity in Health, 18. Retrieved from: https://doi.org/10.1186/s12939-019-1045-8
- Paradies, Y. (2006). A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology, 35(4), 888-901.
- Nicholson, A. K., Borland, R., Davey, M. E., Stevens, M., & Thomas, D. P. (2015). Past quit attempts in a national sample of Aboriginal and Torres Strait Islander smokers. Medical Journal of Australia, 202(10 Supplement), S20-S25.
- Thomas, D. P., Lyons, L., & Borland, R. (2019). Predictors and reasons for starting and sustaining quit attempts in a national cohort of Aboriginal and Torres Strait Islander smokers. Drug and Alcohol Review, 38(3), 244-253.
- Thomas, D. P., Briggs, V., Anderson, I. P. S., & Cunningham, J. (2008). The social determinants of being an Indigenous non-smoker. Australian and New Zealand Journal of Public Health, 32(2), 110-116.
- Arjunan, P., Poder, N., Welsh, K., Bellear, L., Heathcote, J., Wright, D., . . . Wen, L. M. (2016). Smoking among Aboriginal adults in Sydney, Australia. Health Promotion Journal of Australia, 27(1), 66-69.
- Maddox, R., Davey, R., Lovett, R., Cochrane, T., van der Sterran, A., & Corbett, J. (2015). The smoke ring: a mixed methods study. The International Journal of Health, Wellness and Society, 5(2), 55-68.
- Thomas, D. P., Panaretto, K. S., Davey, M., Briggs, V., & Borland, R. (2017). The social determinants and starting and sustaining quit attempts in a national sample of Aboriginal and Torres Strait Islander smokers. Australian and New Zealand Journal of Public Health, 41(3), 230-236.
- Bond, C., Brough, M., Spurling, G., & Hayman, N. (2012). ‘It had to be my choice’ Indigenous smoking cessation and negotiations of risk, resistance and resilience. Health, Risk & Society, 14(6), 565-581.
- Australian Bureau of Statistics. (2018). Prisoners in Australia, 2018 (ABS Cat. no. 4517.0). Canberra: Australian Bureau of Statistics.
- Australian Institute of Health and Welfare. (2018). Youth detention population in Australia 2018. Canberra: Australian Institute of Health and Welfare.
- Australian Institute of Health and Welfare. (2019). The health of Australia’s prisoners 2018 (AIHW Cat. no. PHE 246). Canberra: Australian Institute of Health and Welfare.
- Justice Health & Forensic Mental Health Network, & Juvenile Justice NSW. (2017). 2015 Young People in Custody Health Survey: full report. Sydney: NSW Health.
- Australian Bureau of Statistics. (2010). The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples, Oct 2010 (ABS Catalogue no 4704.0). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2011). Adult health: smoking. Retrieved 17 February 2011 from https://www.abs.gov.au/AUSSTATS/abs@.nsf/lookup/4704.0Chapter755Oct+2010
- Nicholson, A. K., Borland, R., Davey, M. E., Stevens, M., & Thomas, D. P. (2015). Predictors of wanting to quit in a national sample of Aboriginal and Torres Strait Islander smokers. Medical Journal of Australia, 202(10 Supplement), S26-S32.
- Thomas, D., Davey, M., van der Sterren, A., Panaretto, K., & Lyons, L. (2020). Mental health and starting or sustaining quit attempts in a national cohort of Aboriginal and Torres Strait Islander smokers.
- Thomas, D. P., Davey, M. E., Panaretto, K. S., & van der Sterren, A. E. (2018). Cannabis use among two national samples of Aboriginal and Torres Strait Islander tobacco smokers. Drug and Alcohol Review, 31(S1), S394-S403.
- Passey, M. E., Sanson-Fisher, R. W., D’Este, C. A., & Stirling, J. M. (2014). Tobacco, alcohol and cannabis use during pregnancy: clustering of risks. Drug and Alcohol Dependence, 134(1), 44–50.
- Dangol, P., Howle, T., & Johnstone, H. (2018). Aboriginal and Torres Strait Islander adolescent and youth health and wellbeing 2018: in brief. Canberra: Australian Institute of Health and Welfare.
- Wood, L., France, K., Hunt, K., Eades, S., & Slack-Smith, L. (2008). Indigenous women and smoking during pregnancy: knowledge, cultural contexts and barriers to cessation. Social Science & Medicine, 66(11), 2378-2389.
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2016). Attitudes to and beliefs about smoking among Aboriginal peoples and Torres Strait Islanders Tobacco in Australia: facts and issues. Melbourne: Cancer Council Victoria.
- DiGiacomo, M., Davidson, P. M., Davison, J., Moore, L., & Abbott, P. (2007). Stressful life events, resources, and access: key considerations in quitting smoking at an Aboriginal Medical Service. Australian and New Zealand Journal of Public Health, 31(2), 174-176.
- Dawson, A. P., Cargo, M., Stewart, H., Chong, A., & Daniel, M. (2012). Aboriginal Health Workers experience multilevel barriers to quitting smoking: a qualitative study. International Journal for Equity in Health, 11(27), 1-21.
- Greenhalgh, E. M., Scollo, M. M., Pearce, M., Scollo, M. M., & Winstanley, M. H. (2016). Smoking and intergenerational poverty Tobacco in Australia: facts & issues. Melbourne: Cancer Council Australia.
- Roddan, M. (2019). Smokers coughing up $17bn,
- Australian Institute of Health and Welfare. (2017). National Drug Strategy Household Survey (NDSHS) 2016 key findings. Retrieved 1 June 2017 from https://www.aihw.gov.au/reports/illicit-use-of-drugs/ndshs-2016-key-findings/contents/summary
- Cosh, S., Hawkins, K., Skaczkowski, G., Copley, D., & Bowden, J. (2015). Tobacco use among urban Aboriginal Australian young people: a qualitative study of reasons for smoking, barriers to cessation and motivators for smoking cessation. Australian Journal of Primary Health, 21(3), 334-341.
- Maddox, R. (2015). The Smoke Ring: are your friends a drag? Social network analysis and tobacco use. University of Canberra, Canberra.
- Walker, R. C., Graham, A., Palmer, S. C., Jagroop, A., & Tipene-Leach, D. C. (2019). Understanding the experiences, perspectives and values of Indigenous women around smoking cessation in pregnancy: systematic review and thematic synthesis of qualitative studies. International Journal for Equity in Health, 18. Retrieved from: https://doi.org/10.1186/s12939-019-0981-7
- Nicholson, A. K., Borland, R., Bennet, P. T., van der Sterren, A. E., Stevens, M., & Thomas, D. P. (2015). Personal attitudes towards smoking in a national sample of Aboriginal and Torres Strait Islander smokers and recent quitters. Medical Journal of Australia, 202(10 Supplement), S51-S56.
- Johnston, V., Westphal, D. W., Earnshzaw, C., & Thomas, D. P. (2012). Starting to smoke: a qualitative study of the experiences of Australian Indigenous youth. BMC Public Health, 12. Retrieved from: https://doi.org/10.1186/1471-2458-12-963
- Wood, L., Greenhalgh, E. M., Vittiglia, A., Hanley-Jones, S., Scollo, M. M., & Winstanley, M. H. (2019). Stages in the uptake of smoking Tobacco in Australia: facts and issues. Melbourne: Cancer Council Victoria.
- Thomas, D. P., Davey, M. E., Briggs, V. L., & Borland, R. (2015). Talking About The Smokes: summary and key findings. Medical Journal of Australia, 202(10 Supplement), S3-S4.
- Nicholson, A. K., Borland, R., Couzos, S., Stevens, M., & Thomas, D. P. (2015). Smoking-related knowledge and health risk beliefs in a national sample of Aboriginal and Torres Strait Islander people. Medical Journal of Australia, 202(10 Suppl), S45-S50.
- Johnston, V., Thomas, D. P., McDonnell, J., & Andrews, R. M. (2011). Maternal smoking and smoking in the household during pregnancy and postpartum: findings from an Indigenous cohort in the Northern Territory. Medical Journal of Australia, 194(10), 556-559.
- Australian Institute of Health and Welfare. (2020). Alcohol, tobacco & other drugs in Australia [web report]. Retrieved 23 April 2020 from https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/introduction
- Passey, M., D’Este, C. A., Stirling, J. M., & Sanson-Fisher, R. W. (2012). Factors associated with antenatal smoking among Aboriginal and Torres Strait Islander women in two jurisdictions. Drug and Alcohol Review, 31(5), 608-616.
- Bovill, M., Bar-Zeev, Y., Gruppetta, M., Clarke, M., Nicholls, K., O’Mara, P., . . . Gould, G. (2019). Giri-nya-la-nha (talk together) to explore acceptability of targeted smoking cessation resources with Australian Aboriginal women. Public Health, 176, 149-158.
- Davey, M. E., Hunt, J. M., Foster, R., Couzos, S., van der Sterren, A. E., Sarin, J., & Thomas, D. P. (2015). Tobacco control policies and activities in Aboriginal community-controlled health services. Medical Journal of Australia, 202(10 Suppl), S63-S66.
- Chapman, S., & Freeman, B. (2008). Markers of the denormalisation of smoking and the tobacco industry. Tobacco Control, 17(1), 25-31.
- Passey, M. E., Sanson-Fisher, R. W., & Stirling, J. M. (2014). Supporting pregnant Aboriginal and Torres Strait Islander women to quit smoking: views of antenatal care providers and pregnant Indigenous women. Maternal and Child Health Journal, 18(10), 2293-2299.
- Nicholson, A. K., Borland, R., van der Sterren, A. E., Bennet, P. T., Stevens, M., & Thomas, D. P. (2015). Social acceptability and desirability of smoking in a national sample of Aboriginal and Torres Strait Islander people. Medical Journal of Australia, 202(10 Supplement), S57-S62.
- Thomas, D. P., Davey, M. E., van der Sterren, A. E., Lyons, L., Hunt, J. M., & Bennet, P. T. (2019). Social networks and quitting in a national cohort of Australian Aboriginal and Torres Strait Islander smokers. Drug and Alcohol Review, 38(1), 82-91.
- Tane, M. P., Hefler, M., & Thomas, D. P. (2020). Do the Yolŋu people of East Arnhem Land experience smoking related stigma associated with local and regional tobacco control strategies?: An Indigenous qualitative study from Australia. Global Public Health, 14(1), 111-120.
- Thomas, D. P., Ferguson, M., Johnston, V., & Brimblecombe, J. (2013). Impact and perceptions of tobacco tax increase in remote Australian Aboriginal communities. Nicotine & Tobacco Research, 15(6), 1099-1106.
- Nicholson, A. K., Borland, R., Sarin, J., Wallace, S., van der Sterren, A. E., Stevens, M., & Thomas, D. P. (2015). Recall of anti-tobacco advertising and information, warning labels and news stories in a national sample of Aboriginal and Torres Strait Islander smokers. Medical Journal of Australia, 202(10 Suppl), S67-S72.
- Nicholson, A., Borland, R., Bennet, P., Davey, M., Sarin, J., Van der Sterren, A., . . . Thomas, D. (2017). The effect of pack warning labels on quitting and related thoughts and behaviours in a national cohort of Aboriginal and Torres Strait Islander smokers. Nicotine & Tobacco Research, 19(10), 1163-1171.
- Maddox, R., Durkin, S., & Lovett, R. (2016). Plain packaging implementation: perceptions of risk and prestige of cigarette brands among Aboriginal and Torres Strait Islander people. Australian and New Zealand Journal of Public Health, 40(3), 221-225.
- Thomas, D. P., Panaretto, K. S., Stevens, M., Bennet, P. T., & Borland, R. (2015). Smoke-free homes and workplaces of a national sample of Aboriginal and Torres Strait Islander people. Medical Journal of Australia, 202(10 Suppl), S33-S38.
- McDaniel, P. A., Smith, E. A., & Malone, R. E. (2016). The tobacco endgame: a qualitative review and synthesis. Tobacco Control, 25(5), 594-604.
- Wilson, N., Thomson, G. W., Edwards, R., & Blakely, T. (2013). Potential advantages and disadvantages of an endgame strategy: a ‘sinking lid’ on tobacco supply. Tobacco Control, 22(1), i18-i21.
- Hayes, L., Wakefield, M. A., & Scollo, M. M. (2014). Public opinion about ending the sale of tobacco in Australia. Tobacco Control, 23(2), 183-184.
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2019). Policies for advancing tobacco control programs among Aboriginal and Torres Strait Islander peoples Tobacco in Australia: facts and issues. Melbourne: Cancer Council Melbourne.
- Australian Government Department of Health and Ageing. (2013). National Aboriginal and Torres Strait Islander Health Plan 2013-2023. Canberra: Australian Government Department of Health and Ageing.
- Australian Government Department of Health. (2017). National drug strategy 2017-2026. Canberra: Australian Government Department of Health.
- Intergovernmental Committee on Drugs. (2015). National Aboriginal and Torres Strait Islander peoples’ drug strategy 2014-2019. Canberra: National Drug Strategy.
- National Preventative Health Taskforce. (2009). Australia: the healthiest country by 2020 – national preventative health strategy – the roadmap for action. Canberra: National Preventative Health Taskforce.
- Council of Australian Governments. (2008). National Healthcare Agreement. Canberrra: Council of Australian Governments.
- Department of the Prime Minister and Cabinet. (2019). Closing the Gap report 2019. Canberra: Department of the Prime Minister and Cabinet.
- Australian Institute of Health and Welfare. (2020). National Indigenous Reform Agreement: PI 03-Rates of current daily smokers, 2020. Retrieved 16 March 2020
- Australian Institute of Health and Welfare. (2020). National Indigenous Reform Agreement: PI 08-Tobacco smoking during pregnancy, 2020. from https://meteor.aihw.gov.au/content/index.phtml/itemId/718486
- Department of the Prime Minister and Cabinet. (2020). Closing the Gap report 2020. Canberra: Department of the Prime Minister and Cabinet.
- Chamberlain, C., Perlen, S., Brennan, S., Rychetnik, L., Thomas, D., Maddox, R., . . . Eades, S. (2017). Evidence for a comprehensive approach to Aboriginal tobacco control to maintain the decline in smoking: an overview of reviews among Indigenous peoples. Systematic Reviews, 6. Retrieved from: https://doi.org/10.1186/s13643-017-0520-9
- Carson, K., Jayasinghe, H., Smith, B., Newchurch, J., Brinn, M., Veale, A., . . . Singh, K. (2014). Smoking cessation and tobacco prevention in Indigenous populations. Evidence Base(3).
- Carson, K. V., Brinn, M. P., Peters, M., Veale, A., Esterman, A. J., & Smith, B. J. (2012). Interventions for smoking cessation in Indigenous populations. Cochrane Database of Systematic Reviews, 2012(1). Retrieved from: https://doi.org/10.1002/14651858.CD009046.pub2
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2016). Tobacco action initiatives targeting Aboriginal peoples and Torres Straits Islanders Tobacco in Australia: facts and issues. Melbourne: Cancer Council Melbourne.
- Minichiello, A., Lefkowitz, A. R. F., Firestone, M., Smylie, J. K., & Schwartz, R. (2016). Effective strategies to reduce commercial tobacco use in Indigenous communities globally: a systematic review. BMC Public Health, 16. Retrieved from: https://doi.org/10.1186/s12889-015-2645-x
- Power, J., Grealy, C., & Rintoul, D. (2009). Tobacco interventions for Indigenous Australians: a review of current evidence. Health Promotion Journal of Australia, 20(3), 186-194.
- Upton, P., Davey, R., Evans, M., Mikhailovich, K., Simpson, L., & Hacklin, D. (2014). Tackling Indigenous Smoking and Healthy Lifestyle Programme review: executive summary. Canberra: Australian Department of Health.
- Upton, P., Davey, R., Evans, M., Mikhailovich, K., Simpson, L., & Hacklin, D. (2014). Tackling Indigenous Smoking and Healthy Lifestyle Programme review: a rapid review of the literature. Canberra: Australian Department of Health.
- National Aboriginal Community Controlled Health Organisation, & Royal Australian College of General Practitioners. (2018). National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people: 3rd edition. East Melbourne: Royal Australian College of General Practitioners.
- Zwar, N., Richmond, R., Borland, R., Stillman, S., Cunningham, M., & Litt, J. (2004). Smoking cessation guidelines for Australian General Practice. Canberra: Department of Health and Ageing.
- Rice, V. H., Heath, L., Livingstone-Banks, J., & Hartmann-Boyce, J. (2017). Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews, (12). Retrieved from: https://doi.org/10.1002/14651858.CD001188.pub5
- Thomas, D. P., Bennet, P. T., Briggs, V. L., Couzos, S., Hunt, J. M., Panaretto, K. S., . . . Borland, R. (2015). Smoking cessation advice and non-pharmacological support in a national sample of Aboriginal and Torres Strait Islander smokers and ex-smokers. Medical Journal of Australia, 202(10 Suppl), S73-S77.
- Aveyard, P., Begh, R., Parsons, A., & West, R. (2012). Brief opportunistic smoking cessation interventions: a systematic review and meta‐analysis to compare advice to quit and offer of assistance. Addiction, 107(6), 1066-1073.
- Mitchell, E., Bandara, P., & Smith, V. (2018). Tackling Indigenous Smoking program: final evaluation report. Canberra: Australian Government Department of Health.
- Johnston, V., & Thomas, D. P. (2010). What works in Indigenous tobacco control? The perceptions of remote Indigenous community members and health staff. Health Promotion Journal of Australia, 21(1), 45-50.
- New South Wales Health. (2010). The NSW SmokeCheck Aboriginal Tobacco Prevention Project 2007-2008: final report. Sydney: New South Wales Health.
- Hearn, S., Nancarrow, H., Rose, M., Massi, L., Wise, M., Conigrave, K., . . . Bauman, A. (2011). Evaluating NSW SmokeCheck: a culturally specific smoking cessation training program for health professionals working in Aboriginal health. Health Promotion Journal of Australia, 22(3), 189-195.
- Queensland Health. (2008). The health of Queenslanders: prevention of chronic disease 2008 (Second report of the Chief Health Officer Queensland). Brisbane: Queensland Health.
- Campbell, S., Bohanna, I., McKeown-Young, D., Esterman, A., Cadet-James, Y., & McDermontt, R. (2014). Evaluation of a community-based tobacco control intervention in five remote north Queensland Indigenous communities. International Journal of Health Promotion and Education, 52(2), 78-79.
- Cosh, S., Maksimovic, L., Ettridge, K., Copley, D., & Bowden, J. (2013). Aboriginal and Torres Strait Islander utilisation of the Quitline service for smoking cessation in South Australia. Australian Journal of Primary Health, 19(2), 113-118.
- Thomas, D. P., Briggs, V. L., Couzos, S., Panaretto, K. S., van der Sterren, A. E., Stevens M, & Borland, R. (2015). Use of nicotine replacement therapy and stop-smoking medicines in a national sample of Aboriginal and Torres Strait Islander smokers and ex-smokers. Medical Journal of Australia, 201(10 Supplement), S78-S84.
- Australian Government Department of Health. (2012). Medicines to help Aboriginal and Torres Strait Islander people stop smoking: a guide for health workers. Canberra: Australian Government Department of Health.
- Australian Government Department of Health. (2019). Listings on the PBS for Aboriginal and Torres Strait Islander people. Retrieved 14 November 2019 from http://www.pbs.gov.au/info/publication/factsheets/shared/pbs-listings-for-aboriginal-and-torres-strait-islander-people
- Gould, G. S., Stevenson, L. C., Cadet-James, Y., & Clough, A. R. (2018). Cultural challenges when developing anti-tobacco messages for Indigenous Australians. Health Promotion International, 33(2), 345–355.
- McNair Ingenuity Research. (2014). Media use amongst Aboriginal and Torres Strait Islander people (pp. 2). Sydney: McNair Ingenuity Research.
- Hefler, M., Kerrigan, V., Freeman, B., Boot, G. R., & Thomas, D. P. (2019). Using Facebook to reduce smoking among Australian Aboriginal and Torres Strait Islander people: a participatory grounded action study. BMC Public Health, 19. Retrieved from: https://doi.org/10.1186/s12889-019-6918-7
- Malseed, C., Nelson, A., Ware, R., Lacey, I., & Lander, K. (2014). Deadly choices community health events: a health promotion initiative for urban Aboriginal and Torres Strait Islander people. Australian Journal of Primary Health, 20(4), 379-383.
- Gould, G. S., McEwen, A., Watters, T., Clough, A. R., & van der Zwan, R. (2013). Should anti-tobacco media messages be culturally targeted for Indigenous populations? A systematic review and narrative synthesis. Tobacco Control, 22(4), e7.
- Australian Indigenous HealthInfoNet. (2019). Tackling Indigenous Smoking. from http://tis-wp.local/
- Australian Government Department of Health. (2019). Tackling Indigenous Smoking. Retrieved 16 April 2019 from https://www.health.gov.au/initiatives-and-programs/tackling-indigenous-smoking?utm_source=health.gov.au&utm_medium=callout-auto-custom&utm_campaign=digital_transformation
- Chamberlain, C., O’Mara-Eves, A., Porter, J., Coleman, T., Perlen, S. M., Thomas, J., & McKenzie, J. E. (2017). Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database of Systematic Reviews, 2017(2). Retrieved from: http://dx.doi.org/10.1002/14651858.CD001055.pub5
- Bar-Zeev, Y., Lim, L. L., Bonevski, B., Gruppetta, M., & Gould, G. S. (2018). Nicotine replacement therapy for smoking cessation in pregnancy. Medical Journal of Australia, 208(1), 46-51.
- van der Sterren, A., & Goreen Narrkwarren Ngrn-toura – Healthy Family Air Project Team 2010. (2010). Goreen Narrkwarren Ngrn-toura – healthy family air: a literature review to inform the VACCHO Smoking amongst Pregnant Aboriginal Women research project. Melbourne: Victorian Aboriginal Community Controlled Health Organisation.
- Dempsey, D., Jacob, P., & Benowitz, N. L. (2002). Accelerated metabolism of nicotine and cotinine in pregnant smokers. The Journal of Pharmacology and Experimental Therapeutics, 301(2), 594-598.
- Gould, G. S., Bovill, M., Pollock, L., Bonevski, B., Gruppetta, M., Atkins, L., . . . Bar-Zeev, Y. (2019). Feasibility and acceptability of Indigenous Counselling and Nicotine (ICAN) QUIT in Pregnancy multicomponent implementation intervention and study design for Australian Indigenous pregnant women: a pilot cluster randomised step-wedge trial. Addictive Behaviors, 90, 176-190.
- Coleman, T., Chamberlain, C., Davey, M. A., Cooper, S. E., & Leonardi-Bee, J. (2015). Pharmacological interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews. Retrieved from: https://doi.org/10.1002/14651858.CD010078.pub2
- Passey, M. E., D’Este, C. A., & Sanson-Fisher, R. W. (2012). Knowledge, attitudes and other factors associated with assessment of tobacco smoking among pregnant Aboriginal women by health care providers: a cross-sectional survey. BMC Public Health, 12. Retrieved from: http://www.biomedcentral.com/content/pdf/1471-2458-12-165.pdf
- Bar-Zeev, Y., Bonevski, B., Bovill, M., Gruppetta, M., Oldmeadow, C., Palazzi, K., . . . Gould, G. S. (2017). The Indigenous Counselling and Nicotine (ICAN) QUIT in Pregnancy Pilot Study protocol: a feasibility step-wedge cluster randomised trial to improve health providers’ management of smoking during pregnancy. BMJ Open, 7. Retrieved from: https://bmjopen.bmj.com/content/7/8/e016095
- Gould, G. S., & McEwen, A. (2012). An intensive smoking intervention for pregnant Aboriginal and Torres Strait Islander women: a randomised controlled trial [letter]. Medical Journal of Australia, 198(1), 23.
- Bar-Zeev, Y., Bovill, M., Bonevski, B., Gruppetta, M., Oldmeadow, C., Palazzi, K., . . . Gould, G. S. (2019). Improving smoking cessation care in pregnancy at Aboriginal Medical Services: ‘ICAN QUIT in Pregnancy’ step-wedge cluster randomised study. BMJ Open, 9(6). Retrieved from: https://doi.org/10.1136/bmjopen-2018-025293
- Passey, M. E., & Stirling, J. M. (2018). Evaluation of ‘Stop Smoking in its Tracks’: an intensive smoking cessation program for pregnant Aboriginal women incorporating contingency-based financial rewards. Public Health Research & Practice, 28(2). Retrieved from: https://doi.org/10.17061/phrp28011804
- Johnston, V., Thomas, D., Westphal, D., & Earnshaw, C. (2013). Starting to smoke: experiences of Indigenous youth. Melbourne: Lowitja Institute.
- Bell, J. (2012). No smokes project: summative evaluation report: findings from qualitative focus groups. Darwin: Menzies School of Health Research.
- Ivers, R. (2011). Anti-tobacco programs for Aboriginal and Torres Strait Islander people 2011. Canberra.
- Dwyer, J., O’Donnell, K., Lavoie, J., Marlina, U., & Sullivan, P. (2009). The overburden report: contracting for Indigenous health services. Darwin: Cooperative Research Centre for Aboriginal Health.
- Marley, J. V., Kitaura, T., Atkinson, D., Metcalf, S., Maguire, G. P., & Gray, D. (2014). Clinical trials in a remote Aboriginal setting: lessons from the BOABS smoking cessation study. BMC Public Health, 14. Retrieved from: https://doi.org/10.1186/1471-2458-14-579
- Lokuge, K., Thurber, K., Calabria, B., Davis, M., McMahon, K., Sartor, L., . . . Banks, E. (2017). Indigenous health program evaluation design and methods in Australia: a systematic review of the evidence. Australian and New Zealand Journal of Public Health, 41(5), 480-482.
- Wang, Z., & Hoy, W. E. (2013). Lifetime risk of developing coronary heart disease in Aboriginal Australians: a cohort study. BMJ Open, 3. Retrieved from: http://dx.doi.org/10.1136/bmjopen-2012-002308
- McDonald, S. P., Maguire, G. P., Duarte, N., Wang, X. L., & Hoy, W. E. (2004). Carotid intima-media thickness, cardiovascular risk factors and albuminuria in a remote Australian Aboriginal community. Atherosclerosis, 177(2), 423-431.
- Chan, L., Shaw, A. G., Busfield, F., Haluska, B., Barnett, A., Kesting, J., . . . Shaw, J. T. (2005). Carotid artery intimal medial thickness, brachial artery flow-mediated vasodilation and cardiovascular risk factors in diabetic and non-diabetic Indigenous Australians. Atherosclerosis, 18(2), 319-326.
- Maple-Brown, L. J., Cunningham, J., Nandi, N., Hodge, A., & O’Dea, K. (2010). Fibrinogen and associated risk factors in a high-risk population: urban Indigenous Australians, the DRUID Study. Cardiovascular Diabetology, 9(69), 1-26.
- Kruavit, A., Fox, M., Pearson, R., & Heraganahally, S. (2017). Chronic respiratory disease in the regional and remote population of the Northern Territory Top End: a perspective from the specialist respiratory outreach service. Australian Journal of Rural Health, 25(5), 275-284.
- Schubert, J., Kruavit, A., Mehra, S., Wasgewatta, S., Chang, A. B., & Heraganahally, S. (2019). Prevalence and nature of lung function abnormalities among Indigenous Australians referred to specialist respiratory outreach clinics in the Northern Territory. Internal Medicine Journal, 49(2), 217-224.
- Luke, J. N., Brown, A. D., Brazionis, L., O’Dea, K., Best, J. D., McDermott, R. A., . . . Rowley, K. G. (2013). Exploring clinical predictors of cardiovascular disease in a central Australian Aboriginal cohort. European Journal of Preventive Cardiology, 20(2), 246-253.
- Wang, Z., Rowley, K., Best, J., McDermott, R., Taylor, M., & O’Dea, K. (2007). Haemostatic factors in Australian Aboriginal and Torres Strait Islander populations. Metabolism, 56(5), 629-635.
- McWhirter, R. E., Thomson, R. J., Marthick, J. R., Rumbold, A. R., Brown, M. A., Taylor-Thomson, D., . . . Dickinson, J. L. (2014). Runs of homozygosity and a cluster of vulvar cancer in young Australian Aboriginal women. Gynecologic Oncology, 133(3), 421–426.
- Burke, V., Zhao, Y., Lee, A. H., Hunter, E., Spargo, R. M., Gracey, M., . . . Puddey, I. B. (2007). Predictors of type 2 diabetes and diabetes-related hospitalisation in an Australian Aboriginal cohort. Diabetes Research and Clinical Practice, 78(3), 360-368.
- Li, M., & McDermott, R. (2015). Smoking, poor nutrition, and sexually transmitted infections associated with pelvic inflammatory disease in remote north Queensland Indigenous communities, 1998-2005. BMC Women’s Health, 15. Retrieved from: https://doi.org/10.1186/s12905-015-0188-z
- Kildea, S., & Bowden, F. J. (2000). Reproductive health, infertility and sexually transmitted infections in Indigenous women in a remote community in the Northern Territory. Australian and New Zealand Journal of Public Health, 24(4), 382-386.
- Chan, A., Keane, R. J., & Robinson, J. S. (2001). The contribution of maternal smoking to preterm birth, small for gestational age and low birthweight among Aboriginal and non-Aboriginal births in South Australia. Medical Journal of Australia, 174(8), 389-393.
- Gibberd, A. J., Simpson, J. M., Jones, J., Williams, R., Stanley, F., & Eades, S. J. (2019). A large proportion of poor birth outcomes among Aboriginal Western Australians are attributable to smoking, alcohol and substance misuse, and assault. BMC Pregnancy and Childbirth, 19. Retrieved from: https://doi.org/10.1186/s12884-019-2252-4
- Gibberd, A. J., Simpson, J. M., McNamara, B. J., & Eades, S. J. (2019). Maternal fetal programming of birthweight among Australian Aboriginal infants: a population-based data linkage study. The Lancet Global Health, 7(4), e523-e532.
- Pringle, K. G., Rae, K., Weatherall, L., Hall, S., Burns, C., Smith, R., . . . Blackwell, C. C. (2015). Effects of maternal inflammation and exposure to cigarette smoke on birth weight and delivery of preterm babies in a cohort of Indigenous Australian women. Frontiers in Immunology, 6. Retrieved from: https://doi.org/10.3389/fimmu.2015.00089
- Homaira, N., Mallitt, K. A., Oei, J. L., Hilder, L., Bajuk, B., Lui, K., . . . Jaffe, A. (2016). Risk factors associated with RSV hospitalisation in the first 2 years of life, among different subgroups of children in NSW: a whole-of-population-based cohort study. BMJ Open, 6(6). Retrieved from: https://doi.org/10.1136/bmjopen-2016-011398
- Thurber, K. A., Dobbins, T., Kirk, M., Dance, P., & Banwell, C. (2015). Early life predictors of increased body mass index among Indigenous Australian children. PLOS ONE, 10(6). Retrieved from: http://dx.doi.org/10.1371/journal.pone.0130039
- Sutherland, M. R., Chatfield, M. D., Davison, B., Vojisavljevic, D., Kent, A. L., Hoy, W. E., . . . Black, M. J. (2019). Renal dysfunction is already evident within the first month of life in Australian Indigenous infants born preterm. Kidney International, 96(5), 1205-1216.
- McCallum, G. B., Morris, P. S., Grimwood, K., Maclennan, C., White, A. V., Chatfield, M. D., . . . Chang, A. B. (2015). Three-weekly doses of azithromycin for indigenous infants hospitalized with bronchiolitis: a multicentre, randomized, placebo-controlled trial. Frontiers in Pediatrics, 3(32), 1-9.
- Jacoby, P. A., Coates, H. L., Arumugaswamy, A., Elsbury, D., Stokes, A., Monck, R., . . . Lehmann, D. (2008). The effect of passive smoking on the risk of otitis media in Aboriginal and non-Aboriginal children in the Kalgoorlie-Boulder region of Western Australia. Medical Journal of Australia, 188(10), 599-603.
- Australian Bureau of Statistics. (2006). National Aboriginal and Torres Strait Islander Health Survey: Australia, 2004-05 (ABS Catalogue no. 4715.0). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2014). Australian Aboriginal and Torres Strait Islander health survey: updated results, 2012-13 (ABS Catalogue no. 4727.0.55.006). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2013). Australian Aboriginal and Torres Strait Islander health survey: first results, Australia, 2012-13 (ABS Catalogue no. 4727.0.55.001). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2009). National Aboriginal and Torres Strait Islander social survey, 2008. Retrieved 11 April 2011 from http://www.abs.gov.au/AUSSTATS/abs@.nsf/allprimarymainfeatures/357509A09C098E90CA257FA200272E0B?opendocument
- Australian Bureau of Statistics. (2004). National Aboriginal and Torres Strait Islander Social Survey, 2002 (ABS Catalogue no. 4714.0). Canberra: Australian Bureau of Statistics.
- Thomas, D. P., Briggs, V. L., Couzos, S., Davey, M. E., Hunt, J. M., Panaretto, K. S., . . . Borland, R. (2015). Research methods of Talking About the Smokes: an international tobacco control policy evaluation project study with Aboriginal and Torres Strait Islander Australians. Medical Journal of Australia, 202(10 Supplement), S5-S12.
- Australian Institute of Health and Welfare. (2017). National Perinatal Data Collection, 2017: quality statement. Retrieved 4 December 2019 from https://meteor.aihw.gov.au/content/index.phtml/itemId/716326