Review of cardiovascular health among Aboriginal and Torres Strait Islander people
ReviewMerone L1, Burns J2, Poynton M2, McDermott, R3. (2019)
1 Apunipima Cape York Health Council, James Cook University
2 Australian Indigenous HealthInfoNet
3 Centre for Chronic Disease Prevention, James Cook University
Corresponding author: Lea Merone, Email: lea@doctors.org.uk
Suggested citation
Merone L, Burns J, Poynton M, McDermott, R. (2019). Review of cardiovascular health among Aboriginal and Torres Strait Islander people. Perth, WA: Australian Indigenous HealthBulletin 19(4).
Contents
Introduction
Key facts
The context of Aboriginal and Torres Strait Islander cardiovascular health
Historical, social and cultural context
Aboriginal and Torres Strait Islander populations
Extent of cardiovascular disease among Aboriginal and Torres Strait Islander people
Specific cardiovascular conditions
Comorbidity
Management of cardiovascular disease
Management of coronary heart disease
Management of stroke
Management of acute rheumatic fever and rheumatic heart disease
Risk and protective factors
Smoking
Physical activity
Nutrition
Overweight and obesity
Alcohol consumption
Social and emotional wellbeing
Future directions
Concluding comments
References
Download PDF (1.5MB)
Introduction
Cardiovascular disease (CVD) is a major health concern for all Australians, but the levels and impacts are much greater for Aboriginal and Torres Strait Islander people compared with non-Indigenous people. CVD is the leading cause of avoidable death, and death overall for Aboriginal and Torres Strait Islander people. However, there has been progress towards better cardiac care for Aboriginal and Torres Strait Islander people in terms of improvement in access to health services and the mortality rate from cardiac conditions is falling [1].
Cardiovascular disease is the term for all diseases and conditions that affect the heart and blood vessels [2]. Specific types of CVD include coronary heart disease (CHD) (or ischaemic heart disease, IHD), cerebrovascular disease (including stroke), hypertension (high blood pressure), and rheumatic heart disease (RHD) [3]. Most types of CVD (excluding RHD) are subject to the same set of modifiable or non-modifiable risk factors [4]. Modifiable behavioural factors for CVD include tobacco use, physical inactivity, poor dietary behaviour and excessive alcohol consumption [4, 5].
Modifiable biomedical factors include hypertension, high blood cholesterol, overweight and obesity. Certain related health conditions, particularly diabetes, depression [6] and chronic kidney disease, can also increase the risk of developing CVD [5]. Non-modifiable risk factors that can influence the risk of CVD include, age, sex, family history of CVD, and ethnicity [4]. Researchers are considering additional risk factors for CVD for Aboriginal and Torres Strait Islander people, including sleep quality and the presence of particular types of blood fats (lipids) [7].
Unlike other types of CVD, RHD occurs when acute rheumatic fever (ARF), an illness that affects the heart, joints, brain and skin, leads to permanent damage to the heart valves [8-10]. ARF, which is rare among non-Indigenous Australians, is caused by an untreated bacterial (group A streptococci or GAS) infection of the throat, and possibly of the skin. It is often repeated bouts of GAS infection that lead to RHD [10]. Reducing ARF and RHD in Aboriginal and Torres Strait Islander communities requires initiatives that address poverty, overcrowded housing and poor sanitation, all of which contribute to the spread of GAS infection [11].
CVD presents a significant burden for Aboriginal and Torres Strait Islander people [12]. CHD was the leading cause of death in the Aboriginal and Torres Strait Islander population in 2018; Aboriginal and Torres Strait Islander people were 2.0 times as likely to die from CHD than non-Indigenous people [13]. Of all specific CVDs, RHD accounts for the biggest difference in death rates between Aboriginal and Torres Strait Islander and non-Indigenous people [10]. The striking difference between Aboriginal and Torres Strait Islander people and non-Indigenous people in CVD mortality is the much greater impact among young and middle-aged Aboriginal and Torres Strait Islander adults [13].
Mortality data for cardiovascular disease are considered to be reliable for the five jurisdictions: New South Wales (NSW); Queensland (Qld); Western Australia (WA); South Australia (SA) and the Northern Territory (NT) [1]. There is some degree of under-identification of Indigenous status in mortality data from death registrations because some deceased Aboriginal and Torres Strait Islander people are not reported as Indigenous by the family, health worker or funeral director. Work is in progress for assessing the quality of Indigenous identification in mortality data sets and developing methods to adjust for under identification [14].
About this review
The purpose of this review is to provide a comprehensive synthesis of key information on cardiovascular health among Aboriginal and Torres Strait Islander people in Australia to:
- inform those involved or who have an interest in Aboriginal and Torres Strait Islander health, in particular cardiovascular health
- provide the evidence for future policy, strategy and program development and delivery.
The review provides general information on the historical, social and cultural context of cardiovascular health, and the environmental and behavioural factors that contribute to cardiovascular disease. It provides information on the extent of cardiovascular disease, including: incidence and prevalence data; hospitalisations and health service utilisation and mortality. It discusses the issues of prevention and management of cardiovascular health, and provides information on relevant policies and strategies that address cardiovascular diseases among Aboriginal and Torres Strait Islander people. It concludes by discussing possible future directions for cardiovascular health in Australia.
This review draws mostly on journal publications, government reports, national data collections and national surveys, the majority of which can be accessed through the HealthInfoNet’s publications database (http://aih-wp.local/key-resources/publications). Information specifically about cardiovascular health is available at: http://aih-wp.local/learn/health-topics/cardiovascular-health.
Edith Cowan University prefers the term ‘Aboriginal and Torres Strait Islander’ rather than ‘Indigenous’ for its publications. However, when referencing information from other sources, authors may use the terms from the original source. As a result, readers may see these terms used interchangeably with the term ‘Indigenous’ in some instances. If they have any concerns they are advised to contact the HealthInfoNet for further information.
Acknowledgements
Special thanks are extended to:
- the anonymous reviewer whose comments assisted finalisation of this review
- staff at the Australian Indigenous HealthInfoNet for their assistance and support including authors of the Overview of Aboriginal and Torres Strait Islander health status as content from the publication has been used in this review
- the Australian Government Department of Health for their ongoing support of the work of the Australian Indigenous HealthInfoNet
- Sara Noonan, Technical Advisor, RHDAustralia, for her feedback about the acute rheumatic fever and rheumatic heart disease content of this review.
Key facts
- CVD is the leading cause of avoidable death, and overall mortality for Aboriginal and Torres Strait Islander people.
- Of all specific CVDs, RHD accounts for the biggest difference in death rates between Aboriginal and Torres Strait Islander people and non-Indigenous people.
- The CHD death rates for Aboriginal and Torres Strait Islander people and non-Indigenous people between 1998 and 2012 declined by 48% and 49% respectively.
- For 2011-15 in NSW, Qld, WA, SA and the NT, the most common condition causing avoidable mortality for Aboriginal and Torres Strait Islander people was coronary heart disease (22%).
- Lifestyle factors can play a preventive role in CVD, however, risk factors such as smoking, alcohol consumption, physical inactivity and poor diet continue to play a major part in CVD morbidity and mortality in Aboriginal and Torres Strait Islander populations.
The context of Aboriginal and Torres Strait Islander cardiovascular health
Historical, social and cultural context
In 1770, the arrival of Captain Cook and subsequent European colonisation led to conflict with Aboriginal and Torres Strait Islander people. Colonisation has been characterised by, dispossession, displacement, relocation, removal of children, forced labour, massacres, racism, loss of culture and oppression [15]. The enduring effects of colonisation have contributed significantly to the disadvantage and ill-health suffered by Aboriginal and Torres Strait Islander people in Australia today. Transgenerational trauma has resulted from previous government and institutional practices, with present generations still suffering the consequences and disadvantages at individual, family and community levels [16].
In order to achieve health equality, it is important to understand how health disparities have occurred. European settlement and displacement adversely affected access to and use of traditional foods for Aboriginal and Torres Strait Islander people [17]. This has had significant knock-on effects including under and over nutrition and a disproportionate burden of nutrition-related diseases such as cardiovascular disease, metabolic syndrome, type 2 diabetes, chronic kidney disease and some cancers. Traditional foods promoted physical, spiritual, emotional and cultural health and prior to colonisation, Aboriginal and Torres Strait Islanders were generally physically fit, strong and lean. In addition to hunter-gatherer activities, some agricultural activities also occurred [18]. As recently as the 20th century, remote groups of Aboriginal people consumed a traditional diet and demonstrated no evidence of the chronic diseases that characterise the modern health-gap. Following settlement, there was decreased access to traditional foods and increased dependence on imported/introduced foods, such as flour, sugar, tea, and tinned meats. This started the transition from traditional ‘bush-tucker’ diets, to the Westernised diet largely consumed throughout Australia today.
People who are socioeconomically disadvantaged are more likely to have greater levels of chronic diseases [19]. Aboriginal and Torres Strait Islander people have significantly higher rates of diseases linked to social position and lifestyle, such as cardiovascular disease, cancer, diabetes and chronic kidney disease [20]. Inequalities in health are inextricably linked with inequalities in society, including socioeconomic disadvantage, poverty and lack of control. The ‘social gradient’ apparent in many disease states and risk factors, demonstrates that the lower the socio-economic class, the worse the health. Deprivation in: early childhood development, education, employment, income and communities, leads to poor health behaviours and outcomes [21]. Therefore, tackling social inequality, particularly in early childhood development, can decrease the prevalence of chronic disease in the Indigenous populations. In recent years to address the disadvantage, there has been a focus on reconciliation [22] and Closing the Gap [23].
A further consideration in Indigenous health disparity is the cultures of Aboriginal and Torres Strait Islander people which are based on the connection between individuals, families, communities and land [24]. Culture forms an important part of the Aboriginal definition of wellbeing, which is holistic and incorporates the social, emotional and cultural wellbeing of the entire community [25]. Accordingly, when considering Indigenous health, the historical, traumatic, social and cultural aspects need to be considered alongside social and physiological determinants.
Aboriginal and Torres Strait Islander populations
In 2019, the projected Aboriginal and Torres Strait Islander population was estimated by the ABS to be 847,190 people (see Table 1) [26]. The Aboriginal and Torres Strait Islander population accounted for 3.3% of Australia’s total population of nearly 25 and a half million (Derived from [26, 27]). The population of Aboriginal and Torres Strait Islander people continues to grow; between 2011 and 2016, according to Census counts, there was a population increase of 18%, from 548,368 people to 649,171 [28]. Increases in the Aboriginal and Torres Strait Islander population have been attributed to a variety of reasons including a decrease in those with unknown Indigenous status and an increase in those identifying themselves and their children as Aboriginal and/or Torres Strait Islander [29]. Of the total population of Indigenous Australians, in 2016, 91% identified as Aboriginal, 5% as Torres Strait Islander and 4% as both Aboriginal and Torres Strait Islander [30].
For 2019, the Aboriginal and Torres Strait Islander population was highest in NSW (281,107 people), followed by Qld (235,962) (Derived from [26, 27]) (see Table 1). The NT has the highest proportion of Aboriginal and Torres Strait Islander people among its population (32%) and Vic the lowest (0.9%).
Table 1 . Estimated Aboriginal and Torres Strait Islander (Indigenous) population, by jurisdiction, Australia, 2019
| Jurisdiction |
Indigenous population (number) |
Proportion of Australian Indigenous population (%) | Proportion of jurisdiction population (%) |
|---|---|---|---|
| NSW | 281,107 | 33 | 3.5 |
| Vic | 62,074 | 7.3 | o.9 |
| Qld | 235,962 | 28 | 4.6 |
| WA | 106,939 | 13 | 4.1 |
| SA | 44,981 | 5.3 | 2.6 |
| Tas | 30,070 | 3.5 | 6.6 |
| ACT | 8,178 | 1.0 | 1.9 |
| NT | 77,605 | 9.2 | 32 |
| Australia | 847,190 | 100 | 3.3 |
Note:
The Australian population includes Jervis Bay Territory, the Cocos (Keeling) Islands, Christmas Island and Norfolk Island.
Source: Derived from ABS, 2019 [26], ABS, 2019 [27]
In 2016, more than one third, 37%, of Aboriginal and Torres Strait Islander people lived in major cities and 19% lived in remote or very remote regions [30]. This is compared with 73% of non-Indigenous people inhabiting major cities, and 1.5% living in remote or very remote regions. The proportion of Aboriginal and Torres Strait Islander people living in rural areas has decreased from 27% in 1996 to 20% in 2016 [28].
The Aboriginal and Torres Strait Islander population is much younger overall than the non-Indigenous population (Derived from [26, 27]). According to ABS estimates for 2019, 33% of Aboriginal and Torres Strait Islander people were aged less than 15 years, compared with 18% of non-Indigenous people. About 4.9% of Aboriginal and Torres Strait Islander people were aged 65 years or over, compared with 16% of non-Indigenous people.
The life expectancy of Aboriginal and Torres Strait Islander people born in 2015-17 is around eight years lower than that of non-Indigenous people [31]. Males could be expected to live to 71.6 years, 8.6 years less than the 80.2 years expected for non-Indigenous males. Females could be expected to live to 75.6 years 7.8 years less than the 83.4 years expected for non-Indigenous females.
Extent of cardiovascular disease among Aboriginal and Torres Strait Islander people
CVD/circulatory disease covers all diseases affecting the heart and blood vessels. Atherosclerosis – the process of ‘furring of the arteries’ due to fatty deposits on the inner walls of blood vessels – is one of the leading causes of CVD. Risk factors for developing CVD include: obesity, smoking, inadequate fruit and vegetable consumption, physical inactivity, raised blood pressure, high cholesterol, depression and diabetes. CVD is the third leading cause of disease burden in all Australians [32].
In 2008-12, CVD was a leading cause of the health and life expectancy gap observed between Aboriginal and Torres Strait Islanders and non-Indigenous people [33, 34].
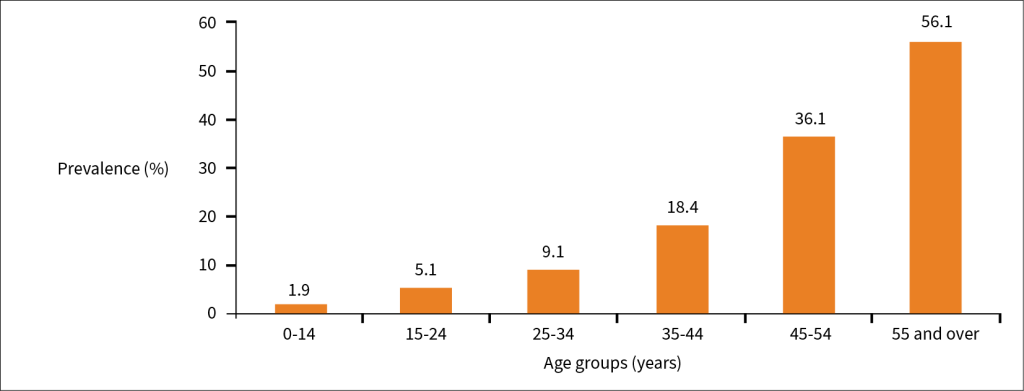
In the 2018-19 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS), 15% of Aboriginal and Torres Strait Islander people (14% of males and 17% of females) self-reported that they had a long-term circulatory system disease; including 5.2% (5.5% of males and 4.9% of females) who reported that they had ‘heart, stroke and vascular disease’ [35]. For those who reported that they had a circulatory system disease, prevalence increased with age, from 1.9% of those aged 0-14 years to 56% in those aged 55 years and older (see Figure 1). Aboriginal and Torres Strait Islander people living in non-remote areas were more likely to report having ‘heart, stroke and vascular disease’ than those living in remote areas (5.4% and 4.9% respectively).
Figure 1. Prevalence (%) of Aboriginal and Torres Strait Islander people reporting diseases of the circulatory system as a long-term health condition, by age group, 2018-19
Note: Prevalence expressed as percentages
Source: ABS, 2019 [35]
More details are available for 2012-13 for specific cardiovascular conditions for Aboriginal and Torres Strait Islander people aged 35+ (see Table 2, some figures may be unreliable and need to be interpreted with caution) [36].
Table 2: Prevalence (%) of self-reported cardiovascular conditions Aboriginal and Torres Strait Islander people aged 35+ by years and sex, 2012-13
| Condition | Prevalence Males % | Prevalence Females % | Prevalence all % |
|---|---|---|---|
| Angina | 3.1 | 3.4 | 6.4 |
| Heart attack and other coronary heart disease | 4.4 | 3.1 | 3.6 |
| Stroke and other CVD | 1.7 | 2.4 | 2.1 |
| Oedema and heart failure | 1.2* | 1.5 | 1.3 |
| Peripheral vascular diseases | 0.4** | 0.6* | 0.5* |
| All | 10.8 | 10.8 | 10.9 |
Notes:
*Interpret with caution, relative error 25-50%
**Unreliable, relative standard error >50%
Source: Nichols, Peterson, Herbert and Allender, 2015 [36]
Hospitalisation
There is some under-identification of Aboriginal and Torres Strait Islander people in the National Hospital Morbidity Database but data for all states and territories are considered to have adequate identification from 2010-11 onwards [37]. An Australian Institute of Health and Welfare (AIHW) study found that the ‘true’ number of hospitalisations nationally was about 9% higher than reported.
In 2017-18, there were 14,945 hospitalisations among Aboriginal and Torres Strait Islander people in Australia for CVD (34 per 1,000) [38] representing 5.4% of all Aboriginal and Torres Strait Islander hospital separations (excluding dialysis) (Derived from [38]).
More details are available for 2015-16, when there were 14,000 hospitalisations among Aboriginal and Torres Strait Islander people for CVD; Aboriginal and Torres Strait Islander people were 1.7 times more likely to be hospitalised for CVD than non-Indigenous people (34 per 1,000 compared with 19 per 1,000 respectively) [39]. The disparity between Aboriginal and Torres Strait Islander and non-Indigenous Australians was greater for females (2 times higher for females: 32 per 1,000 compared with 15 per 1,000) than males (1.5 times: 36 per 1,000 compared with 24 per 1,000).
More details are also available for 2013-14 when there were 11,868 hospital separations in Australia identified as Aboriginal and Torres Strait Islander for CVD as the principal diagnosis (see Table 3) [33]. The rate was 1.8 times higher among Aboriginal and Torres Strait Islander people than for non-Indigenous people (31 per 1,000 and 18 per 1,000 respectively). Coronary heart disease (CHD) was the principal diagnosis for 4,771 of Aboriginal and Torres Strait Islander hospitalisations, representing 40% of CVD hospitalisations with male hospitalisations exceeding female hospitalisations (43% and 37% respectively). The other leading diagnoses for hospitalisation for CVD in Indigenous people included: heart failure and cardiomyopathy (1,730 hospitalisations, 15%), stroke (838 hospitalisations, 7%), peripheral vascular disease (420 hospitalisations, 4%), rheumatic heart fever (RHF) and rheumatic heart disease (RHD) (516 hospitalisations, 4%), and hypertensive heart disease (356 hospitalisations, 3%).
Table 3. Numbers of Aboriginal and Torres Strait Islander hospitalisations for CVD conditions, by sex, 2013-14
| CVD type | Numbers | % of CVD hospitalisations | ||
|---|---|---|---|---|
| Males | Females | Persons | ||
| Coronary heart disease | 2,700 | 2,071 | 4,771 | 40 |
| Heart failure and cardiomyopathy | 868 | 862 | 1,730 | 15 |
| Stroke | 430 | 408 | 838 | 7 |
| Peripheral vascular disease | 257 | 163 | 420 | 4 |
| ARF and RHD | 203 | 313 | 516 | 4 |
| Hypertensive heart disease | 141 | 215 | 356 | 3 |
| Other cardiovascular disease | 1,690 | 1,547 | 3,237 | N/A |
| CVD total | 6,289 | 5,579 | 11,868 | 100 |
| Congenital heart disease | 115 | 116 | 231 | N/A |
Source: AIHW, 2015 [33]
In 2013-15, age-specific hospitalisation rates for CVD rose with age, from 1.4 per 1,000 for those aged 0-4 years to 107 per 1,000 for those aged over 65 years. Although rates were highest for those aged over 65 years, CVD is recognised as having a substantial impact on younger Aboriginal and Torres Strait Islander people, with the age-specific rate for those aged 35-44 years being 21 per 1,000 in 2013-15 [40]. Hospitalisation rates for CVD also increased with remoteness; in 2014-15, crude rates ranged from 12 per 1,000 in major cities to 27 per 1,000 in remote and very remote areas [41].
Rates of hospitalisation for heart-related conditions for Aboriginal and Torres Strait Islander people vary between regions. In 2012-2016, age-standardised rates of hospitalisation for heart attack, angina and heart failure combined were highest in the SA4 region of `Perth – North East’ (20 per 1,000) and `Darwin’ (18 per 1,000), and lowest in `Sydney – Outer West and Blue Mountains’ (5.4 per 1,000) and `Central Coast’ (NSW) (6.6 per 1,000) [42].
In 2013-15, ARF/RHD was responsible for the biggest disparity, rate ratio: 7.2, in hospitalisation rates between Aboriginal and Torres Strait Islander and non-Indigenous people of all specific CVD diagnoses [40].
From 2004-5 to 2014-15 there was a 17% increase in hospitalisations for circulatory diseases in Aboriginal and Torres Strait Islander populations, compared with a 12% decrease in non-Indigenous hospitalisations in NSW, Vic, Qld, WA, SA, and the NT [32].
Mortality
CHD was the leading cause of death in 2018 for Aboriginal and Torres Strait Islander people (390 deaths) in NSW, Qld, WA, SA and the NT accounting for 12% of all deaths with a rate of 117 per 100,000 [13]. The mortality rate due to cerebrovascular disease was 44 per 100,000 (105 deaths).
More details are available for deaths for CVD types for 2011-2015. About a quarter (24%) of all deaths of Aboriginal and Torres Strait Islander people in NSW, Qld, WA, SA and the NT combined were caused by CVD [40]. The age-standardised death rate due to CVD for Aboriginal and Torres Strait Islander people was 271 per 100,000. Of specific CVD types, CHD caused the greatest number of deaths (55% of CVD deaths), followed by other heart disease (17%), cerebrovascular disease (17%), hypertensive diseases (4.6%), RHD (3.4%), and other diseases of the circulatory system (3.3%) (see Table 4).
Table 4: CVD causes of death for Aboriginal and Torres Strait Islander people by sex, in NSW, Qld, WA, SA and the NT, 2011-15
| CVD type |
Males |
Females |
All |
||||
|---|---|---|---|---|---|---|---|
| Number of deaths | Rate per 100,000 | Number of deaths | Rate per 100,000 | Number of deaths | Rate per 100,000 | % of CVD deaths | |
| Coronary heart disease | 1,135 | 183 | 607 | 100 | 1,742 | 138 | 55 |
| Acute myocardial infarction | 406 | 70 | 271 | 47 | 677 | 58 | 22 |
| Other heart disease | 251 | 42 | 271 | 47 | 522 | 45 | 17 |
| Cerebrovascular disease | 225 | 54 | 301 | 60 | 526 | 58 | 17 |
| Stroke | 180 | 42 | 249 | 48 | 429 | 46 | 14 |
| Hypertensive heart disease | 70 | 14 | 75 | 15 | 145 | 15 | 4.6 |
| Rheumatic heart disease | 38 | 4.5 | 70 | 8.1 | 108 | 6.4 | 3.4 |
| Other circulatory diseases | 55 | 11 | 50 | 8.2 | 105 | 9.3 | 3.3 |
| Total CVD deaths | 1,774 | 309 | 1,374 | 238 | 3,148 | 271 | 100 |
Notes:
- Directly age-standardised using the 2001 standard population
2. Data presented for acute myocardial infarction are a subset of data presented for all coronary heart disease, and data presented for stroke are a subset of data presented for all cerebrovascular disease.
Source: Australian Health Ministers’ Advisory Council, 2017 [32]
Between the periods 2009-2013 and 2014-2018, the CHD death rate decreased by 11% from 133 per 100,000 to 118 per 100,000 people [13]. Since 2009, decreases among males and females have occurred at 12% and 11% respectively.
Main causes of avoidable deaths
Potentially avoidable deaths are defined as those in individuals under the age of 75 years from conditions that are preventable or treatable within primary or hospital care [21]. In 2011-15 in NSW, Qld, WA, SA and the NT, the two most common conditions causing avoidable mortality for Aboriginal and Torres Strait Islander people were CVD (22%), and diabetes mellitus (12%) [32]. Avoidable CVD mortality for 2011-15 among Aboriginal and Torres Strait Islander populations in NSW, WA, SA, NT and QLD for coronary heart disease, cerebrovascular disease and rheumatic/valvular heart disease are summarised in Table 5.
Table 5: Avoidable CVD mortality rates by Indigenous status, and Indigenous:non-Indigenous rate ratios, NSW, WA, SA, NT, Qld, 2011-15
| Cause of death | Age-standardised rates per 100,000 population | Rate ratio | |
|---|---|---|---|
|
Aboriginal and Torres Strait Islander |
Non-Indigenous |
||
| Coronary heart disease |
83 |
20 |
4.2 |
| Cerebrovascular disease |
20 |
6.9 |
2.9 |
| Rheumatic/valvular heart disease |
7.6 |
1.3 |
5.7 |
Note:
Rounding may result in inconsistencies in calculated rate ratios.
Source: Australian Health Ministers’ Advisory Council, 2017 [32]
Avoidable mortality for Aboriginal and Torres Strait Islander people decreased by 32% between 1998 and 2015, suggesting improvements in healthcare [32].
Specific cardiovascular conditions
Coronary heart disease
CHD, also known as ischaemic heart disease, is the single biggest cause of mortality in Australia and is the main contributor to overall burden of disease. It occurs when there is narrowing in the blood vessels of the heart [43]. There are two broad types of CHD, acute myocardial infarction heart attack (AMI) and angina [44]. AMI is acute and life-threatening complete occlusion of a blood vessel in the heart, leading to chest pain and death of part of the heart muscle. Angina is a chronic disease characterised by incomplete occlusion of the blood supply leading to periods of temporary insufficiency and chest pain. Heart attacks and unstable angina are considered to be part of a continuum of acute CHD known as acute coronary syndrome (ACS). It causes significant chronic disease, disability, poor life quality and premature mortality, all of which contribute to high costs to the healthcare system.
In the 2018-19 NATSIHS, the proportion of people who reported that they had ‘heart, stroke and vascular disease’ as a long-term condition was 5.2% (5.5% for males and 4.9% for females); there was an increase from 1.1% for people aged 25-34 years to 26% for people aged 55 years and over [35]. The proportions were the same for those living in non-remote and remote areas, both 5%. The proportion of people who reported that they had ‘heart, stroke and vascular disease’ increased from 4.0% in 2012-13 to 5.2% in 2018-19.
CHD is the most common CVD condition among Aboriginal and Torres Strait Islander people and is more prevalent in the Aboriginal and Torres Strait Islander population than in the non-Indigenous population [33]. In the 2012-13 AATSIHS, 15,600 Aboriginal and Torres Strait Islander adults reported that they had CHD, after age-adjustment, they were almost twice as likely to have CHD than non-Indigenous adults (6.3% and 3.2% respectively). CHD prevalence was greater in older age groups; 2.8% of Aboriginal and Torres Strait Islander adults aged 35-44 years had CHD compared with 18% aged 65 years and over. Aboriginal and Torres Strait Islander adults aged 18-34 years were 5 times more likely to have CHD as non-Indigenous adults, this declined to 1.4 times for those aged 65 years and over.
In 2012, the rate of acute coronary events for Aboriginal and Torres Strait Islander people was 995 per 100,000, 2.5 times higher than for non-Indigenous people (399 per 100,000) [33]; this is a decline from 2007 for Aboriginal and Torres Strait Islander people (1,048 per 100,000 and for non-Indigenous people (515 per 100,000). In younger age groups, rates of acute coronary events were higher for Aboriginal and Torres Strait Islander people compared with non-Indigenous people. The rate was 13 times higher for the 25-34 year age group for Aboriginal and Torres Strait Islander people compared with non-Indigenous people (104 per 100,000 and 8 per 100,000 respectively), 7 times higher for the 35-44 year age group (552 per 100,000 and 75 per 100,000 respectively), 3 times higher for 55-64 year age group (1,519 and 474 per 100,000 respectively) and 1.2 times higher for 75 years and over (2,413 and 1,989 per 100,000 respectively).
Studies have shown large differences in CHD event incidence between Aboriginal and Torres Strait Islander people and non-Indigenous matched groups. For example, data linkage for 1998-2006 in Perth, WA, that first event incidence was six times higher in urban Aboriginal people than for the non-Indigenous people and the difference was almost 20-fold in women aged 45-54 years [45].
In 2013-14 there were 4,771 hospitalisations for Aboriginal and Torres Strait Islander people with a principal diagnosis of CHD, with a rate of 13 per 1,000 [33]. Hospitalisation rates for CHD were higher for Aboriginal and Torres Strait Islander males than females (16 per 1,000 and 11 per 1,000 respectively). Rates increased with age for males and females to age group 65-74 years but declined for the age group 75 years and over. Aboriginal and Torres Strait Islander people were hospitalised for CHD at 2.4 times the rate for non-Indigenous people (13 and 6 per 1,000 respectively). Aboriginal and Torres Strait Islander hospitalisation rates for CHD were higher than non-Indigenous rates across all age groups with the greatest gap for the 25-34 year age group (8 times higher) and 35-44 years (7 times higher).
Between 2005-08 and 2014-17, after age-adjustment, the in-hospital mortality rate for Indigenous patients admitted for cardiac conditions fell from 68 to 61 per 100,000 population and for non-Indigenous Australians, it fell from 43 per 100,000 to 30 per 100,000 [1].
During 2014-15 to 2016-17, about 4% (crude rate) of hospitalisations for acute myocardial infarction (AMI) among Aboriginal and Torres Strait Islander people aged 35 years and over ended with death (137 deaths) [1]. The in-hospital death rate after age-adjustment was similar for Aboriginal and Torres Strait Islander people and non-Indigenous people (3% vs 2.8% respectively, rate ratio: 0.9). Between 2005-08 and 2014-17, the in-hospital death rate due to AMI fell among both Aboriginal and Torres Strait Islander adults (from 4% to 3%) and non-Indigenous adults (from 5% to 2.8%).
In 2018 in NSW, Qld, WA, SA and the NT, CHD continued to be the leading cause of death in Aboriginal and Torres Strait Islanders, responsible for the deaths of 390 people [13]. Rates for Aboriginal and Torres Strait Islander people were 2.0 times higher than for non-Indigenous people (117 per 100,000 compared with 59 per 100,000 respectively). There were 256 deaths of Aboriginal and Torres Strait Islander males, rates were 2.1 times higher than for non-Indigenous males (157 per 100,000 and 74 per 100,000 respectively). There were 134 deaths of Aboriginal and Torres Strait Islander females, rates were 1.9 times higher than for non-Indigenous females (84 per 100,000 and 45 per 100,000 respectively).
Age-specific CHD death rates in 2014-2018 increased with age, with rates being highest for those aged 75 years and over [13]. Although rates were highest among older people, CHD is recognised as having a substantial impact on younger Aboriginal and Torres Strait Islander adults; CHD was the leading cause of death for those aged 35-44 years (rate of 49 per 100,000 deaths) and the fourth-leading cause of death for those aged 25-34 years (rate of 12 per 100,000 deaths). CHD death rates in 2014-2018 were highest in the NT (179 per 100,000) and lowest in NSW (87 per 100,000).
Table 6 shows the age-standardised death rates from CHD for 2009-2013 for males and females and by jurisdiction [36, 46].
Table 6: Coronary heart disease deaths and death rates per 100,000, 2009-2013 by Indigenous status, sex and jurisdiction, NSW, NT, Qld, WA, SA
| State/Territory |
Deaths |
Standardised death rate |
Deaths |
Standardised death rate |
|---|---|---|---|---|
| Males | Females | |||
| New South Wales |
296 |
158 |
193 |
101 |
| Northern Territory |
207 |
258 |
90 |
108 |
| Queensland |
306 |
189 |
160 |
104 |
| Western Australia |
195 |
238 |
113 |
126 |
| South Australia |
60 |
139 |
32 |
71 |
Source: Heart foundation, 2015 [36], ABS 2015 [46]
The CHD death rates for Aboriginal and Torres Strait Islander people between 1998 and 2012 declined by 48%, which was similar to the decline for non-Indigenous people (49%) [33]. The decline for Aboriginal and Torres Strait Islander females (59%) was greater than for Aboriginal and Torres Strait Islander males (38%).
In the Perth Aboriginal Atherosclerosis Risk Study, a cohort was assessed at baseline (1998/1999) and 913 urban-living Aboriginal people were followed up to 2006 [45]. A comparison group of 3,582 non-Aboriginal people, sex-matched and post code-matched, were selected from the Perth electoral roll. From electronic record linkage, prior CHD and first CHD events from both groups were recorded and the rates of first CHD events (hospital admission or CHD deaths per 1,000 person years) and the incidence rates were calculated. It was found that CHD events occurred at a much younger age in the Aboriginal population and age and sex-specific CHD rates in the urban Aboriginal people far exceeded those of the general population and were equally excessive among men and women.
A study that included 1,115 Aboriginal people from a remote tribal group, who were free from CHD at baseline, 1992 to 1995, and who were followed up for 20 years [47]. New CHD incident cases were identified from hospital and death records. It was found that the lifetime risk of developing CHD for Aboriginal and Torres Strait Islander men and women was one in two. There were 185 people who developed CHD; the average age at which the first CHD event occurred was 48 years for men and 49 years for women. The risk of developing CHD increased with age until 60 years and then decreased with age. Lifetime cumulative risk without adjusting for competing risk was 70.7% for men and 63.8% for women. After adjusting for the presence of competing risk of death from non-CVD causes, the lifetime risk was 52.6% for men and 49.2% for women.
Cerebrovascular Disease
Cerebrovascular disease includes all disorders that cause parts of the brain to become ischaemic – have reduced blood flow – usually due to haemorrhage (bleeding) or narrowing/blockage of the blood vessels in the brain [48]. Stroke is the commonest term used for cerebrovascular diseases and refers to either blockage or bleeding resulting in reduced blood flow to the brain tissue. Symptoms can include muscle weakness, slurred speech, loss of vision, dizziness and confusion. Symptoms that resolve are termed a transient ischaemic attack. Strokes may cause a range of disability or even death.
Modifiable risk factors for cerebrovascular disease include [48]:
- hypertension
- smoking
- diabetes
- high cholesterol
- obesity
- poor diet and physical inactivity
- atrial fibrillation
- alcohol excess.
Epidemiological data surrounding stroke in Aboriginal and Torres Strait Islander populations are sparse. Information on strokes as self-reported by non-Indigenous and Indigenous people is available from the 2016 National Eye Health Survey (NEHS) [49, 50]. It was found that the crude prevalence of stroke among Indigenous people aged 40 years and over was 8.8%. After age-adjustment, the prevalence was 13%, indicating Indigenous people were 3 times more likely to have reported stroke than non-Indigenous people [50].
A study documented stroke prevalence in Aboriginal and Torres Strait Islander people in WA for the period 2007-2011 using a weighted average of annual prevalence and histories of 11 comorbidities identified by using a 20-year look back period [51]. The study found that prevalence using linked data was four times higher than for non-Indigenous adults for those aged 25-84 years and there was a higher prevalence in a younger cohort of patients. There was a high prevalence of both risk factors and comorbidities, suggesting primary prevention may be fundamental in reducing stroke incidence in Aboriginal and Torres Strait Islander populations.
The pooled results from two South Australian population-based studies (2009-11) and found that the age-standardised incidence of stroke for Aboriginal people was almost double that of the non-Indigenous population although the sample size was small [52].
In 2004-5, an estimated 1,400 Aboriginal and Torres Strait Islander people (0.3% of the population) had experienced cerebrovascular disease (stroke would be expected to be the most common condition) [53]. Prevalence was similar for males and females. The estimated prevalence of stroke was 1.7 times higher for Aboriginal and Torres Strait Islander people than for non-Indigenous people.
In 2013-14, there were 838 hospitalisations identified as Indigenous with a principal diagnosis of stroke at a rate of 2.7 per 1,000 [33]. The stroke hospitalisation rates identified as Indigenous were higher for males than for females (3.0 and 2.5 per 1,000 respectively). Rates were higher for older age groups for both males and females; for the age group 75 years and over, the hospitalisation rate for stroke was 1.8 times higher than for the 65-74 years age group. Hospitalisation rates identified as Indigenous for stroke were twice the rate of non-Indigenous hospitalisations and rates were higher across all age groups.
A study in the NT, 1992-2013, they found Aboriginal patients had 71% more hospital bed-days and 7.4% fewer procedures than non-Indigenous patients. Aboriginal patients were 34% more likely to die from stroke than non-Indigenous patients [54].
In 2018, for Aboriginal and Torres Strait Islander people in NSW, Qld, WA, SA and the NT, the mortality rate due to cerebrovascular disease was 44 per 100,000 (105 deaths), 1.3 times higher than for non-Indigenous people, 34 per 100,000 [13]. Cerebrovascular disease was the eighth-leading cause of deaths of Aboriginal and Torres Strait Islander people. Age-specific death rates for cerebrovascular disease for males (43 per 100,000) were similar to those for females (45 per 100,000). Age-adjusted cerebrovascular death rates for Aboriginal and Torres Strait Islander people in 2014-2018 were highest in WA (59 per 100,000) and lowest in NSW (32 per 100,000).
For 2014-2018, the rate ratio was particularly high for the age group 65-74 years (see Table 7) [13].
Table 7. Cerebrovascular disease mortality by Indigenous status and age groups over 65 years, rates per 100,000 and rate ratios in NSW, Qld, WA, SA and the NT, 2014-2018.
| Age group
(years) |
Indigenous |
Non-Indigenous |
Rate ratio |
|---|---|---|---|
|
Males |
|||
| 65-74 |
109 |
58 |
1.9 |
| 75+ |
n/a |
n/a |
n/a |
|
Females |
|||
| 65-74 |
76 |
39 |
1.9 |
| 75+ |
571 |
610 |
0.9 |
|
Persons |
|||
| 65-74 |
92 |
49 |
1.9 |
| 75+ |
510 |
556 |
0.9 |
Source: Australian Institute of Health and Welfare, 2019 [13]
Hypertension
Hypertension, also known as high blood pressure, is a leading risk factor for stroke, CHD, kidney disease, blindness and peripheral vascular disease (leading to leg ulcers). Hypertension is highly prevalent in the Australian population; many people have undiagnosed hypertension including Aboriginal and Torres Strait islanders [55].
Blood pressure
Blood pressure is categorised as optimal, normal, high-normal, grade 1 hypertension (mild), grade 2 hypertension (moderate), grade 3 hypertension (severe) and isolated systolic hypertension [55].
| Diagnostic category for adults | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| Optimal | <120 | <80 |
| Normal | 120-129 | 80-84 |
| High-normal | 130-139 | 85-89 |
| Grade 1 (mild) hypertension | 140-159 | 90-99 |
| Grade 2 (moderate) hypertension | 160-179 | 100-109 |
| Grade 3 (severe) hypertension | 180+ | 110+ |
| Isolated systolic hypertension | >140 | <90 |
High-normal blood pressure is also known as ‘pre-hypertension’. This is associated with a greater likelihood of having a myocardial infarction (heart attack) and coronary artery disease compared with someone with normal blood pressure [55].
Hypertension is one of the most important modifiable disease factors for Aboriginal and Torres Strait Islander people. Risk factors for developing hypertension include: physical inactivity, poor diet, obesity, excess alcohol consumption and increasing age [32]. Nationally in the AATSHIS 2012-2013, participants who were obese were twice as likely as those who were not obese to have high blood pressure (37% and 18% respectively) [32].
In the 2018-19 NATSIHS, 8.3% of Aboriginal and Torres Strait Islander people (8.2% for males and 8.4% for females) reported that they had hypertension [35]. This was an increase from 5% in 2012-13, driven mainly by the proportion of people with hypertension doubling from 4% to 8% in non-remote areas. The proportion was higher in remote areas (10%) than in non-remote areas (8%). The proportion of people who reported having hypertension increased with age from 3% of people aged 25-34 years to 38% of people aged 55 years and over. Voluntary blood pressure measurements were taken at the time of the interview for adults 18 years and over and it was found that 23% of participants had a high blood pressure reading; this was similar for those living in non-remote areas (23%) and remote areas (22%). The proportion of people with a high reading was higher than in 2012-13 (20%) and higher for males (25%) than females (21%). A high reading doesn’t necessarily mean that a person has high blood pressure, but it can indicate that a person may have undiagnosed or untreated hypertension. For those aged 25-34 years, the proportion with a high reading (16%) was around five times higher than the proportion with hypertension (3%). By 55 years and over, the proportion with a high reading (37%) and reported hypertension was about the same.
The National key performance indicators for Aboriginal and Torres Strait Islander primary health care results to June 2018 reported that as a chronic disease management indicator less than half, 41%, of clients with type 2 diabetes had a blood pressure result at or below the accepted target level of 130/80 mmHg [56].
A study examined health service data from a community screening for the Young Persons Check in 11 remote communities in north Qld between March 2009 and April 2011 [57]. The study examined the prevalence of pre-hypertension, hypertension and other cardiovascular risk factors for 1,883 Aboriginal and Torres Strait Islander people aged 15-24 years. The prevalence of hypertension was 34% (grade 1: 18% and grade 2: 3.3%). In terms of risk factors, the prevalence of elevated waist circumference was 48%, overweight or obesity, 46%, elevated triglcerides, 18%, decreased HDL, 55% and proteinuria, 24%.
A study examined the prevalence of hypertension among 657 Aboriginal and Torres Strait Islander children aged 2-17 years (median age 6.3 years) attending four urban Aboriginal Community Controlled Health Organisations (ACCHOs) from 2008 to 2011 [58]. The prevalence of hypertension was 16% and for pre-hypertension it was 12%. One of the strongest predictors of hypertension was caregiver BP (0.15 increase in systolic z-score per 10 mmHg of caregiver BP; child BMI z-score was significantly related to diastolic (0.08 increase (0.01-0.15) per mg/m BMI increase).
Hypertension in childhood is highly predictive of hypertension in adulthood and contributes to the development of the metabolic syndrome – characterised by central obesity, high cholesterol, high blood pressure and insulin resistance [59]. However, the evidence of childhood hypertension and future CVD events is currently lacking and further investigation is required.
In 2013-14, there were 356 (141 for females and 215 for males) hospitalisations among Aboriginal and Torres Strait Islander people for hypertensive disease accounting for 3% of CVD hospitalisations [33].
Information for 2013-15 hospitalisations for hypertension showed that there was an increase with age (see Table 8); the rates were consistently higher for Aboriginal and Torres Strait Islander people than for non-Indigenous people for all age groups and the rate ratio peaked at 45-54 years [32].
Table 8: Age-specific hospitalisation rates per 1,000 people and rate ratios for the principal diagnosis of hypertension, by Indigenous status and by age group over 5 years, 2013-15
| 5-14 years | 15-24 years | 25-34 years | 35-44 years | 45-54 years | 55-64 years | 65+ years | |
|---|---|---|---|---|---|---|---|
| Indigenous | 0.1 | 0.1 | 0.3 | 0.6 | 1.4 | 1.7 | 2.8 |
| Non-Indigenous | 0 | 0 | 0.1 | 0.2 | 0.3 | 0.5 | 1.9 |
| Rate ratio | 1.9 | 2.2 | 4.2 | 3.8 | 4.5 | 3.4 | 1.4 |
Note: Rounding may result in inconsistencies in calculated rate ratios
Source: Australian Institute of Health and Welfare, 2017 [40]
In 2011-15, hypertensive disease as an underlying cause of CVD was responsible for 145 deaths of Aboriginal and Torres Strait Islander people (70 males and 75 females), 4.6% of CVD deaths, in NSW, Qld, WA, SA and the NT [32].
In 2011, hypertension was responsible for 5% of the total burden of disease in Aboriginal and Torres Strait Islander people and 8% of the health gap between Indigenous and non-Indigenous people.
Acute rheumatic fever and rheumatic heart disease
Acute rheumatic fever (ARF) and rheumatic heart disease, although sometimes seen in the non-Indigenous population, are predominantly observed in Aboriginal and Torres Strait Islander populations [10]. While rates of ARF and RHD throughout Australia have declined overall, they remain major contributors to childhood and adult cardiovascular disease throughout the NT and central Australia [10, 60]. Recurrent ARF increases the risk of progression to RHD, heart failure and premature mortality.
Acute rheumatic fever and rheumatic heart disease
Acute rheumatic fever (ARF): is an autoimmune response to group A streptococcus infection [61]. Group A streptococcus infection may cause throat or skin infections, however the autoimmune response to this in ARF causes joint pain, fevers and requires hospitalisation. Approximately 0.3-3% of those with streptococcus Strep A throat infection are genetically susceptible to developing ARF [60]. Following ARF, and if the heart was involved, rheumatic heart disease (RHD) can occur which can cause lasting damage [10]. Stretching or scarring of the heart valves results in disruption to the blood flow and heart surgery may be needed [62]. Untreated, RHD can result in heart failure, arrhythmias, stroke, endocarditis (inflammation of the inner lining of the heart) and complications during pregnancy and labour. Symptoms of RHD are subtle and may not be noticed for years.
The National Rheumatic Heart Disease Data Collection includes information about diagnoses of rheumatic heart disease (RHD) by jurisdiction [10]. Jurisdictional data for the incidence of ARF and the prevalence of RHD are currently only available from RHD registers for Qld, WA, SA and the NT [63]. It is not possible to directly compare data from these registers, because they were developed at different times, and disease notification varies between the jurisdictions . In NSW, ARF in people of any age and RHD in people aged <35 years were added to the list of notifiable conditions in 2015, and a register for people with ARF/RHD has been established [64].
|
NT |
QLD |
WA |
SA |
NSW |
VIC, TAS, ACT |
|
|---|---|---|---|---|---|---|
|
RHD Control Program |
1997 |
2009 |
2009 |
2010 |
2015 |
– |
|
ARF/RHD Register |
1997 |
2006 |
2009 |
2012 |
2016 |
– |
Acute rheumatic fever
In 2013-2017, there were 1,776 diagnoses (85 per 100,000) for ARF among Aboriginal and Torres Strait Islander Australians, accounting for 94% of all diagnoses and with a rate of more than 250 times the rate for non-Indigenous Australians [10]. The rate for Aboriginal and Torres Strait Islander females (1,006 diagnoses, 96 per 100,000) was higher than for males (770 diagnoses, 74 per 100,000) overall, however for children, ARF rates were higher in males (see Table 9). Rates were highest for the age group 5-14 years (602 diagnoses, 195 per 100,000). Over half (53%, 954 diagnoses) of all ARF diagnoses were from the NT; the regions with the highest notifications were Rural Darwin (249 diagnoses, 387 per 100,000) and East Arnhem (212 diagnoses, 366 per 100,000). The Kimberley in WA also had high rates (180 diagnoses, 200 per 100,000). Of note, there is a lack of robust data from other remote Indigenous populations [65]. The rate of ARF has generally increased over time in each jurisdiction, apart from for WA where there was no clear pattern [10]. In 2017, for the NT, there were 268 diagnoses, more than twice the number in 2013 (127) and in Qld, the number of diagnoses almost tripled from 43 to 124.
Table 9. Acute rheumatic fever diagnoses number and rates per 100,000 among Aboriginal and Torres Strait Islanders by sex and age, 2013-2017
| Age group (years) |
Male number |
Male rate |
Female number |
Female rate |
Total number |
Total rate |
|---|---|---|---|---|---|---|
| 0-4 |
32 |
26 |
30 |
25 |
62 |
25 |
| 5-14 |
478 |
203 |
424 |
186 |
602 |
195 |
| 15-24 |
151 |
71 |
274 |
134 |
425 |
102 |
| 25-44 |
104 |
38 |
256 |
91 |
360 |
65 |
| 45+ |
5 |
2.6 |
22 |
10 |
27 |
6.7 |
| Total |
770 |
74 |
1,006 |
96 |
1,776 |
85 |
Source: AIHW, 2019 [10]
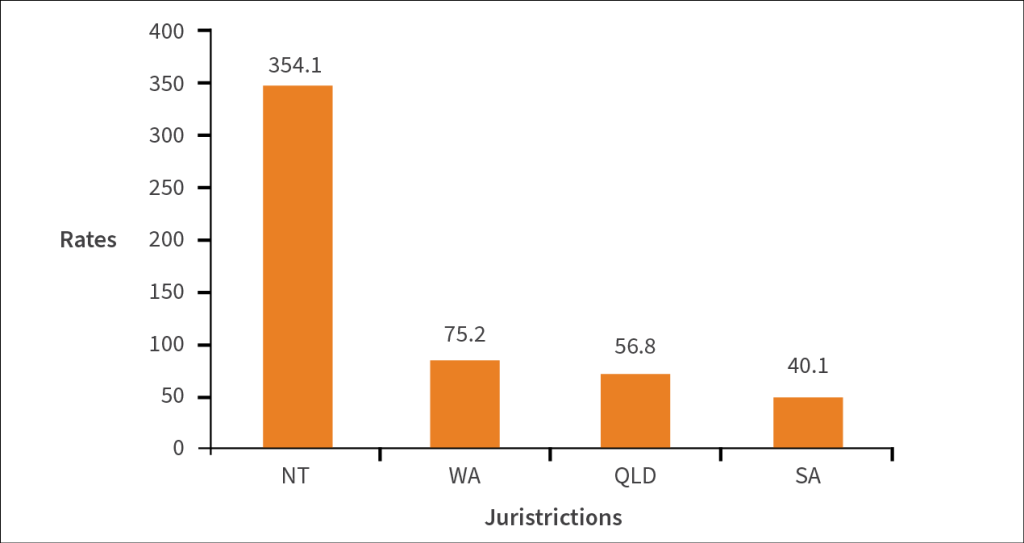
ARF rates for Aboriginal and Torres Strait Islander people in the NT, Qld, WA and SA in 2017 are summarised below (Figure 2) [10].
Figure 2: Acute rheumatic fever rates per 100,000 population for Aboriginal and Torres Strait Islander people in the NT, WA, Qld and SA, 2017
Source: AIHW, 2019 [10]
For NSW, for October 2015-December 2017, there were 19 ARF diagnoses for Aboriginal and Torres Strait Islander people [10].
For 2013-2017, the incidence of ARF for Aboriginal and Torres Strait Islander people in Qld, WA, SA and the NT rose from 63 per 100,000 to 111 per 100,000 [1]. Although the reasons are unclear, it is possible that this could be due to better reporting and registration of ARF.
In 2016-17 in Qld, WA, SA and the NT, 26% of ARF episodes (241 of 920) among Aboriginal and Torres Strait Islander people were recurrences compared with 17% of ARF episodes (11 of 65) among non-Indigenous Australians [63].
For 2013-2017, there were 19 deaths (16 in the NT) of Aboriginal and Torres Strait Islander people who had ARF (not RHD), although these people could have died from any cause [10].
Rheumatic heart disease
For 2013-2017, there were 1,043 new RHD diagnoses among Aboriginal and Torres Strait Islander Australians in NT, Qld, WA and SA, a rate of 50 per 100,000 (see Table 10) [10]. The rate was about 125 times the rate for non-Indigenous people (0.4 per 100,000). The rate for females was about twice the rate for males generally and females had higher rates compared with males in all age groups apart from those aged 0-4 years. For young Indigenous women with RHD, there can be substantial risks from valvular heart diseases during pregnancy and labour [66]. Nearly 60% of new RHD cases were for those aged less than 25 years old at diagnosis [10].
Table 10: Number and rate per 100,000 of new RHD diagnoses among Aboriginal and Torres Strait Islander people in NT, Qld, WA and SA, by age (years) and sex, 2013-2017
|
Male |
Female |
Total |
||||
|---|---|---|---|---|---|---|
| Age group
(years) |
Number |
Rate |
Number |
Rate |
Number |
Rate |
| 0-4 |
8 |
6.4 |
7 |
5.9 |
15 |
6.1 |
| 5-14 |
164 |
70 |
195 |
86 |
359 |
78 |
| 15-24 |
71 |
33 |
167 |
82 |
238 |
57 |
| 25-44 |
79 |
29 |
218 |
77 |
297 |
53 |
| 45 and over |
36 |
19 |
98 |
46 |
134 |
33 |
| Total |
358 |
34 |
685 |
65 |
1,043 |
50 |
Note: Rates per 100,000
Source: AIHW, 2019 [10]
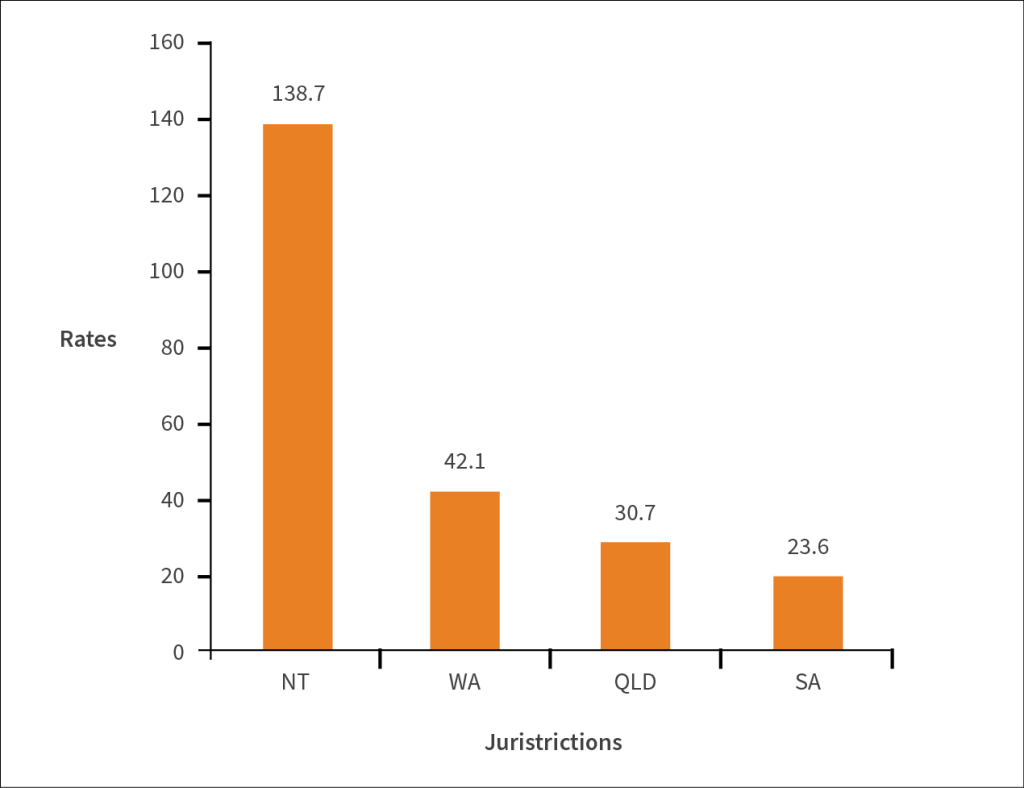
For 2013-2017, the region with the highest rate of new RHD diagnoses was East Arnhem (104 diagnoses, 179 per 100,000) followed by Northwest Qld (64 diagnoses, 145 per 100,000) [10]. For 2017, the highest number and rate of new RHD diagnoses were in the NT (see Figure 3). As at 31 December 2017, for Aboriginal and Torres Strait Islander people, there were 3,690 living RHD cases with the NT having the highest number (see Table 11). In 2013-2017, among all new RHD diagnoses identified as Indigenous, about 4 in 5 (838 diagnoses) did not have a previous ARF episode recorded on the registers [61]. One reason why ARF cases have not been notified to a register is diagnosis before a resister began.
Figure 3: Rate of new diagnoses of RHD per 100,000 Aboriginal and Torres Strait Islander people by selected jurisdictions, 2017
Source AIHW, 2019 [10]
Table 11: Number of Aboriginal and Torres Strait Islander and non-Indigenous people living with RHD in NT, QLD, WA, SA, as at 31 December 2017
| Jurisdiction |
Number of Indigenous persons |
Number of non-Indigenous people |
|---|---|---|
| NT |
1,846 |
108 |
| Qld |
1,161 |
331 |
| WA |
522 |
32 |
| SA |
161 |
20 |
Source: AIHW, 2019 [10]
In NSW for October 2015–December 2017, there were 14 RHD diagnoses (4.0 per 100,000) among Aboriginal and Torres Strait Islander people compared with 30 RHD diagnoses (0.4 per 100,000) among non-Indigenous people [10].
A screening study of high-risk Aboriginal and Torres Strait Islander children aged 5-15 years in northern and central Australia, between 2008 and 2010, showed a definite RHD prevalence of 8.6 per 1,000 and a borderline RHD prevalence of 17 per 1,000 [65]. Prevalence of both definite and borderline RHD was shown to increase with age and peaked at 47 per 1,000 in the 12 year old age group. Over 50% of the definite cases detected were new diagnoses.
A study in the NT of residents in 1997-2010 demonstrated that ARF incidence for Indigenous people was highest in the 5-14 year age-group (males: 162 per 100,000; females 228 per 100,000) [67]. The ARF recurrence rate declined by 9% per year after diagnosis. Following first diagnosis of ARF, 61% of those with ARF developed RHD within a decade and of those, almost 30% progressed to heart failure within 5 years.
Hospitalisation
For 2013-2017, 322 Aboriginal and Torres Strait Islander people underwent 350 surgery events for RHD (the majority had one surgery while 21 people had 2 surgical events and 2 people had 4 surgical events) [10]. About half of the surgery cases were from the NT (176 surgical events), and one third (112 surgical events) were from Qld.
Hospitalisations for ARF/RHD among Aboriginal and Torres Strait Islander people were about seven times higher after age-adjustment than those for non-Indigenous people for 2013-14 to 2014-15 [32]. Hospitalisation rates among Aboriginal and Torres Strait Islander people were highest in the NT and lowest in NSW and Vic (3.7 versus 0.2 per 1,000 persons respectively). In 2013-15, rates were highest in Aboriginal and Torres Strait Islander children aged 10-14 years (see Table 12), however in the non-Indigenous population, rates increased with age and peaked in those over 65 years.
Table 12: Hospitalisation numbers and rates per 1,000 for ARF or RHD for Aboriginal and Torres Strait Islander people by age group, Australia, 2013-15
| Age group Years |
Number | Rate of hospitalisation per 1,000 population: Aboriginal and Torres Strait Islander | Rate ratio: Indigenous: non-Indigenous |
|---|---|---|---|
| 0-4 |
19 |
0.1 |
54.2 |
| 5-9 |
155 |
0.9 |
85.0 |
| 10-14 |
258 |
1.6 |
64.5 |
| 15-19 |
116 |
0.8 |
46.7 |
| 20-24 |
78 |
0.6 |
56.2 |
| 25-34 |
159 |
0.8 |
39.8 |
| 35-44 |
114 |
0.7 |
20.7 |
| 45-54 |
76 |
0.6 |
7.0 |
| 55-64 |
54 |
0.6 |
4.0 |
| 65+ |
33 |
0.6 |
1.3 |
Note: Rate ratio is the Indigenous rate divided by the non-Indigenous rate
Source: Australian Health Ministers’ Advisory Council, 2017 [32]
Deaths
For 2013-2017, there were 221 deaths of Aboriginal and Torres Strait Islander people who had RHD, although they may have died from any cause [10]. Most deaths occurred in the NT.
For 2011-15, Aboriginal and Torres Strait people in NSW, Qld, WA, SA and the NT were 4.7 times more likely to die from RHD than non-Indigenous people (6.4 per 100,000 compared with 1.4 per 100,000, after age-adjustment) [32]. There were 108 deaths from RHD (representing 3.4% of all circulatory disease deaths for Indigenous people): 38 males (representing 2.1% of all circulatory disease deaths for Indigenous males) and 70 females (representing 5.1% of all circulatory disease deaths for Indigenous females) [32]. Numbers of RHD deaths for age groups, were: 0-4 years: 4, 5-14 years: 4, 15-24 years: 7, 25-34 years: 9, 35-44 years: 14, 45-54 years: 25, 55-64 years: 24, 65-74 years: 17 and 75+ years: 7.
A data linkage study in the NT (register entries 1997-2013 for ARF or RHD) suggested that mortality among people with RHD was 6.6 times higher for Indigenous patients than for non-Indigenous patients and that over a quarter (28%) of this difference was due to concurrent chronic kidney disease and alcohol misuse [32, 68].
In the Burden of Disease Study 2011, the contribution of RHD to CVD burden for Aboriginal and Torres Strait Islander people was 5.1% [12]. RHD burden is dominated by its high mortality burden; 84% of total RHD burden. The overall burden from CVD for rheumatic heart disease was greater for females (61%) than males (39%).
Congenital heart disease
Congenital heart disease
Congenital heart diseases are present at birth; they include holes between pumping chambers of the heart, valves that don’t open or close properly and narrowing of major blood vessels of the aorta and pulmonary artery [69]. Causes of congenital heart disease are multifactorial and can arise through genetic (e.g. Down syndrome) and environmental factors. Congenital heart diseases affect over 2,400 Australian babies each year and many require complex, specialised care. There have been recent improvements in treatment and care leading to extended survival and more active lives for people with congenital heart disease.
In 2016-17, there were 249 hospitalisations of Aboriginal and Torres Strait Islander people with congenital heart disease (rate: 22 per 100,000).
A study investigated survival for Aboriginal and Torres Strait Islander and non-Indigenous children with congenital heart disease who were born in WA from 1980 to 2010. [70]. This study demonstrated an increased risk of mortality for Aboriginal children with congenital heart diseases.
Congenital heart disease is a leading cause of death among infants in Australia [69]. In 2017, 46% of deaths due to congenital heart disease were for those aged 1 year or under. For 2015-2017, congenital heart disease was the cause of death for 29 Aboriginal and Torres Strait Islander people (12 males and 17 females) in NSW, Qld, WA, SA and the NT (rate: 1.1 per 100,000).
Comorbidity
If one or more conditions co-occur with a primary disease, it is known as comorbidity, for example, CVD often occurs concurrently with diabetes and chronic kidney disease (CKD) [33]. CVD, diabetes and CKD have complex causes and share a number of health risk factors, their interactions can worsen health outcomes [33, 71, 72]. Aboriginal and Torres Strait Islander people often have multiple behavioural and biomedical risk factors for a number of chronic diseases [19, 33]. Comorbidity is also linked with higher mortality and this contributes to the life expectancy gap observed between Aboriginal and Torres Strait Islanders and non-Indigenous people.
In the 2012-13 AATSIHS, 35% of Aboriginal and Torres Strait Islander adults had CVD, diabetes or CKD [33]. Of all Indigenous adults with CVD, diabetes or CKD, 38% had 2 or more conditions together, 11% had all 3 conditions together. The prevalence of comorbidity increased with age. Participants who reported that they had diabetes were 2.2 times more likely than other participants to have high blood pressure (51% and 23% respectively) as were those who reported having kidney disease (57% and 26% respectively) [32].
A study estimated that based on biomedical data provided from the 2012-13 AIATSIS, that more than a quarter of Aboriginal and Torres Strait Islander people aged 35-74 years were at high risk of a CVD event in the next 5 years (9.6% with prior CVD and 15.7% at high risk of a primary event) [73]. More than 80% of those at high primary risk were identified by clinical criteria, mainly diabetes and 58% of those at high primary risk were not receiving recommended lipid-lowering therapy.
In 2013-14, there were 65,707 hospitalisations, excluding dialysis, for Aboriginal and Torres Strait Islander adults aged 25 years and over where CVD, diabetes (three quarters, 76% included diabetes) or CKD were present as principal diagnosis and/or additional diagnosis; 63% had only 1 disease recorded [33]. There were 11,702 hospitalisations for CVD only and 1,531 were for CKD only, the remaining 24,506 (37%) of hospitalisations recorded 2 or 3 of the diseases: 11%, CVD and diabetes together; 3%, CVD and CKD; 5%, CVD and diabetes; and 18%, all 3 diseases. The proportion of Indigenous hospitalisations with all 3 diseases (18%) was higher than for non-Indigenous hospitalisations (7%).
A review of the literature about coronary artery bypass grafting (CABG) in Aboriginal and Torres Strait Islander Australians for the management of CHD found that high rates of left ventricular dysfunction were documented, potentially reflecting barriers to medical care or the influence of high rates of diabetes in the Indigenous population
(diabetic patients have been shown to have reduced ventricular function compared with non-diabetics) [74]. Younger patients with higher rates of preventable risk factors constituted the Indigenous CABG population and Indigenous females were over-represented. It was concluded that excess morbidity and mortality in the long-term following CABG appears to be largely contributed to by higher rates of ventricular dysfunction and comorbidities.
It is common for 2 or more comorbid conditions to contribute to a death and CVD, diabetes and CKD are often listed concurrently on death certificates [33]. They are classed as either the underlying cause of death, the immediate cause of death, an intervening cause, or condition(s) that contributed to the death but was not related to the disease or condition causing death. In 2010-2012, there were 4,149 deaths identified as Aboriginal and Torres Strait Islander in NSW, Qld, WA, SA and NT, where CVD, diabetes or CKD were recorded as either an underlying or an associated cause of death, comprising 58% of total Indigenous deaths. CVD, diabetes and CKD were more commonly listed together on Indigenous death certificates, 23% had any 2 conditions compared with 14% of non-Indigenous deaths. Of all Indigenous deaths with CVD, diabetes or CKD listed, 16% had CVD and diabetes listed together compared with 11% of non-Indigenous deaths and 11% of Indigenous deaths had all 3 conditions listed compared with 3% of non-Indigenous deaths.
Management of cardiovascular disease
Aboriginal and Torres Strait Islander people often do not receive the same level of health care as non-Indigenous people for a variety of reasons. Biases, both conscious and unconscious within the health system occur globally, and consequentially [75]. Racism, both institutional, interpersonal and perceived (internalised) affect attitude towards treatment. Aboriginal and Torres Strait Islander knowledge and beliefs can be challenged by the Westernised biomedical model of care, impacting on how Aboriginal and Torres Strait Islander people interact with the healthcare system on a daily basis [76]. Disparities in care must be addressed in order to close the gap and provide culturally safe clinical care.
Access to health care is a key issue for Aboriginal and Torres Strait Islander patients. Disadvantages in treatment are compounded by remoteness and lack of access to appropriate care, cultural barriers and individual and collective experiences of healthcare [77]. In a survey of Aboriginal and Torres Strait Islander people, the lack of access to Aboriginal Health Workers (AHWs) was of particular concern [78]. Also, a lack of understanding of the role of AHWs is a barrier to shared care. A study in the NT noted that the relationship with health staff was important for compliance [79]. Post-discharge management has also been found to be suboptimal for Aboriginal and Torres Strait Islander people owing largely to inadequate discharge planning and poor communication between the hospital and the primary care giver [77].
Many systemic issues have been found that contribute to the poorer outcomes for CHD in Aboriginal and Torres Strait Islander populations. These include: mistrust/fear, institutional racism, cultural misunderstandings, transport and accessibility issues, economic constraints, waiting times and poor health literacy [80].
In a study of the perspectives of health professionals about barriers and enablers for access to health care for Aboriginal people, the most common challenges reported were a lack of time, the availability of culturally appropriate resources and the disconnection between Western medical and Aboriginal views of health [81]. Community awareness may help reduce some barriers, particularly those pertaining to poor health literacy [82].
The primary care sector plays a fundamental role in primary (and secondary) prevention of CVD. Primary prevention involves modifying risk factors for CVD and is a key strategy to reduce health inequality for Aboriginal and Torres Strait Islander people [82]. Aboriginal Community Controlled Health Organisations (ACCHOs) can help reduce barriers by providing AHWs and offering a range of programs. Aboriginal and Torres Strait Islander people are eligible for a comprehensive annual health assessment that covers a wide variety of risk factors related to cardiac disease and other chronic diseases [1]. In 2017-18, there were 236,000 health checks (Medicare MBS item 715) provided to 230,000 Aboriginal and Torres Strait Islander people (minimum time between checks is 9 months); this is more than three times the number of checks than for 2010-11 [83]. Computerised alerts for screening can help with prevention and follow-up [82].
To calculate risk for CHD, the standard absolute risk calculation utilised in Australia is the Framingham Risk Score, however it is deemed too conservative for this high-risk population of Aboriginal and Torres Strait Islander people [84]. Consequentially, two alternative, recalibrated risk scores have been proposed, one contained within the Central Australian Rural Practitioners Association (CARPA) manual [85] and another devised by Hua et al. (2017) and Tran-Duy et al. (2019) [86, 87]. There is little information regarding the utilisation of these scoring systems in primary care when working with Aboriginal and Torres Strait Islander patients. Current scoring systems do not account for additional economic, social, cultural and physical risk factors [88].
Secondary prevention strategies are designed to prevent further decline in the condition of those already diagnosed with CVD [82]. Relative risk reductions in mortality and CVD events are noted with modifying certain behavioural risk factors outlined in Table 13 [82].
Table 13: Decreases in relative risk associated with secondary prevention
| % Relative risk reduction | Secondary prevention modification |
|---|---|
| 67% | People aged <65 years who have never smoked |
| 40% | People aged >65 years who have never smoked |
| 22% | Treatment with ACE inhibitor (medication) |
| 20% | Treatment with Beta blocker (medication) |
| 20% | Increased physical activity |
| 20% | Controlled cholesterol levels |
| 19% | Treated with aspirin |
| 14% | Controlled blood pressure |
Source: Reath et al., 2010 [82]
Rehabilitation is an important part of secondary prevention for both CHD and stroke, with the overall aim of giving people the confidence, motivation and ability to engage in lifestyle changes [89]. Cardiac rehabilitation involves the co-ordinated utilisation of medical, social, educational and psychological measures to allow patients the opportunity to regain the highest possible function following a cardiac event [78]. It is a mainstay of secondary prevention of further events. However, engagement of Aboriginal and Torres Strait Islander patients in cardiac rehabilitation is known to be low [90].
A study in Queensland found uptake for rehabilitation by Aboriginal and Torres Strait Islander cardiac patients was low [78]. Engagement was poor due to lack of knowledge about rehabilitation, low income and having a large extended family. It is possible that owing to issues with availability of AHWs, there was not the support required to enable Aboriginal and Torres Strait Islander patients to engage with rehabilitation programs.
Generally across Australia, few eligible Aboriginal and Torres Strait Islander patients attend cardiac rehabilitation [91]. Furthermore, failure to refer to rehabilitation services is another barrier for Aboriginal and Torres Strait Islander and non-Indigenous people alike when accessing secondary prevention, and more is required to embed the referral process into standard care [90]. In WA, a study found that there is a need for services to better meet the needs of Aboriginal and Torres Strait Islander people with CVD and in particular, with culturally appropriate cardiac rehabilitation, good systematic data collection across services, benchmarks that enable regular monitoring and upskilling of staff to ensure that they are aware of cardiac rehabilitation guidelines and promote uptake [90].
The National Health and Medical Research Council (NHMRC) (2005) published a guide to strengthen cardiac rehabilitation in Aboriginal and Torres Strait Islander populations [92]. Key points for successful engagement included:
- cultural competency and collaboration with Aboriginal and Torres Strait Islander patients
- having a process for identifying Aboriginal and Torres Strait Islander patients
- involvement of Aboriginal Health Workers wherever possible
- acknowledging the importance of family and kinship relationships
- developing flexible approaches to information sharing
- talking about rehabilitation early in the diagnostic and management process
- utilising Aboriginal and Torres Strait Islander ‘buddys’ or ‘mentors’
- exploring existing networks in the community that may be of use
- engaging with communities
- providing culturally respectful discharge plans.
Barriers to rehabilitation for Aboriginal and Torres Strait Islander patients have been identified and include: cultural misunderstanding, lack of continuity of care, community norms and behaviours converse to medical advice, perceptions of hospitals as ‘places where our people go to die’, weak links between mainstream healthcare, extended family responsibilities, lack of community support, cultural appropriateness of the program (or lack thereof), disempowering health messages in the media and lack of flexibility in hospital-based rehabilitation programs [92].
Much work is still required for all requiring cardiac rehabilitation, but particularly for Aboriginal and Torres Strait Islanders who once again face several barriers to care that must be surmounted. There have been reports that there are effective alternatives to hospital-based rehabilitation that may be of benefit to those living remotely, including: brief interventions (for low-risk patients only), telehealth interventions with tele-monitoring, community and home-based cardiac rehabilitation and complementary therapies [93].
Access to care from a geographical and transportation stand-point is a real consideration when caring for Aboriginal and Torres Strait Islander people, particularly those in remote settings. Aboriginal and Torres Strait Islander people face decreased access to medications, delayed access to acute care and lower rates of investigation and intervention [82].
A literature review on cardiac rehabilitation in rural and remote areas found that there were five themes that influenced cardiac rehabilitation: referral; health services pathways and planning; cultural and geographic, necessitating alternative and flexible programs; professional roles and influence; knowing, valuing and psychosocial factors; and financial costs – personal and health services [94]. The study found weak systems with low referral rates and poor access to cardiac rehabilitation in rural and remote areas. There were low levels of involvement of Aboriginal and Torres Strait Islander people and a lack of cultural understanding by non-Indigenous staff.
Management of coronary heart disease
To diagnose or treat CHD, there are a number of procedures, coronary angiography for diagnosis and surgical procedures for revascularisation such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) [33].
In 2015-16, Aboriginal and Torres Strait Islander people with a suspected or confirmed cardiac condition were less likely than non-Indigenous people to be reviewed by a specialist after a cardiac related procedure; for those aged under 65 years, 76% compared with 92% respectively and for those over 65 years, 93% compared with 97% respectively [63].
During 2014-15 to 2016-17, there were 1,068 hospitalisations for Aboriginal and Torres Strait Islander adults for ST-Elevation myocardial infarction (STEMI), (4% of all hospitalised STEMI events) [1]. After age-adjustment, 64% of hospitalised STEMI events among Aboriginal and Torres Strait Islander adults were treated by PCI compared with 79% of such events among non-Indigenous adults (rate ratio: 0.8). Between 2004-05 and 2016-17, after age-adjustment, the proportion of hospitalised STEMI events treated by PCI among Aboriginal and Torres Strait Islander adults rose from 26% to 73% and from 53% to 81% for non-Indigenous adults.
During 2014-15 to 2016-17, there were 5,751 hospitalisations for acute coronary syndrome (ACS) among Aboriginal and Torres Strait Islander adults aged 18 years and over, of which 51% (crude rate) included diagnostic angiography (27% PCI; 4% CABG) and 53% included at least 1 diagnostic angiography or definitive revascularisation procedure [1]. After age-adjustment, the proportion of hospitalised ACS events among Aboriginal and Torres Strait Islander adults receiving a diagnostic angiography and/or definitive revascularisation procedure was 55% compared with 67% for non-Indigenous adults (rate ratio: 0.8). Between 2004-05 and 2016-17, after age adjustment, the proportion of hospitalisations for ACS events among Aboriginal and Torres Strait Islander adults that included either a diagnostic angiography or a definitive revascularisation procedure rose from 32% to 58%, compared with a rise from 45% to 67% among non-Indigenous adults.
In an examination of emergency admissions in WA for CHD it was found that after adjusting for age and sex, Aboriginal and Torres Strait Islander patients were 23% less likely than non-Indigenous people to receive coronary angiography [95]. Following adjustment for comorbidities and private health insurance, the gap decreased to 9%. Much of the disparity was owing to the higher burden of comorbidity in the Aboriginal and Torres Strait Islander patient group, there was little difference in the rates of angiography between Aboriginal and Torres Strait Islanders and non-Indigenous patients in younger patients, however, in older patients aged 55 years and over there was a significant discrepancy (rate ratio: 0.88).
In the Perth Aboriginal Atherosclerosis Risk Study and WA hospital morbidity data for 1980-2006 there was little difference in coronary artery re-vascularisation procedures (CARP) for CVD between age and sex matched Aboriginal and Torres Strait Islander and non-Indigenous patients [96]. Aboriginal people were more likely to have CABG than PCI.
A retrospective review of case notes from patients admitted to two tertiary hospitals in Adelaide for December 2007 to December 2009 and found that Aboriginal and Torres Strait Islander patients with acute coronary syndromes were typically younger and presented later in the disease process than non- Indigenous patients [97]. Aboriginal and Torres Strait Islander patients were 54% less likely to undergo angiography than non-Indigenous patients, however after adjustment for age, sex and propensity score, this difference disappeared. Aboriginal and Torres Strait Islander patients were 20% more likely to receive recommended medications compared with non-Indigenous patients.
In an examination of emergency ACS admissions to hospitals in SA between 2007 and 2012, analysis suggested that Aboriginal and Torres Strait Islander patients, after age-adjustment, were less likely than non-Indigenous patients to receive coronary angiography [98]. Possible reasons included patient-related factors and their preferences and the appropriateness of the intervention. Angiography was more likely if family members or Aboriginal liaison officers were present.
Aboriginal and Torres Strait Islanders with cardiac events may delay presentation to hospital owing to: lack of understanding of the severity of the illness (low health literacy), conflicting priorities such as family responsibility, cultural beliefs, fear of medical institutions, lack of accessible transport and communication issues and failure of triage to appreciate the severity of illness [99].
It has been found in a study that Aboriginal and Torres Strait Islander people have a unique subset of comorbid conditions which predispose them to cardiovascular disease and subsequently high incidence of major adverse cardiac events (MACE) post intervention [100]. Data were assessed on PCI and CABG cases among Aboriginal and Torres Strait Islander patients, 2006-2007, at The Townsville Hospital and MACE outcomes were assessed at 30 days, 1, 5 and 10 years:
Of 66 patients who underwent PCI:
- 1 had a MACE event at 30 days
- 4 had a MACE event at 1 year
- 19 had a MACE event at 5 years
- 32 had a MACE event at 10 years
Of 66 patients who underwent CABG
- 1 had a MACE event at 30 days
- 5 had a MACE event at 1 year
- 8 had a MACE event at 5 years
- 32 had a MACE event at 10 years
One of the aims of The Heart Foundation’s Lighthouse Hospital Project is to reduce the incidence and impact of discharge against medical advice for Aboriginal and Torres Strait Islander people admitted to hospital with a cardiac condition [101].
Management of stroke
Quality of care is an important aspect for decreasing the risk of disability or mortality following a stroke [102]. Similar to CHD, there are reports that Aboriginal and Torres Strait Islander patients who have suffered a stroke have received lower quality care and have had less favourable outcomes than non-Indigenous people [103-105]. Aboriginal and Torres Strait Islander people have a greater prevalence of stroke risk factors, are more likely to suffer an intracranial haemorrhage, less likely to receive timely health assessments and less likely to be treated in a stroke unit when compared with non-Indigenous people [105]. In the Australian National Stroke Audit of services in 2009, it was found that Aboriginal and Torres Strait Islander stroke patients aged between 18 and 64 years had a three-fold risk of dying or permanent disability compared with non-Indigenous patients.
A study that examined stroke data from the Australian National Stroke Audit in 2009 to compare the stroke care between Aboriginal and Torres Strait Islander and non-Indigenous people [103]. Aboriginal and Torres Strait Islander people admitted with stroke tended to be younger, with greater prevalence of risk factors and degrees of comorbidity. Recommended care processes were not as strictly adhered to when caring for Aboriginal and Torres Strait Islander patients, and they were less likely to be treated on a stroke unit despite evidence for the benefits of this. There were also more likely to be delays in care and assessment of Aboriginal and Torres Strait Islander stroke patients and no Aboriginal and/or Torres Strait Islander patient received intravenous thrombolysis, an important acute treatment for ischaemic stroke.
An historical cohort study of 43 Indigenous and 167 non-Indigenous patients admitted to Tamworth Rural Referral Hospital between January 2010 and January 2015 with an ischaemic cerebrovascular accident found that Indigenous patients were significantly less likely to have investigations completed, including carotid imaging and echocardiography [106]. Discharge follow-up was significantly lower for the Indigenous population than the non-Indigenous population. Overall, Indigenous stroke patients were 15.8 years younger than non-Indigenous patients and were more likely to have stroke risk factors including smoking, diabetes mellitus and a past history of CVA (cerebrovascular accident (stroke)) or TIA (transient ischaemic attack).
In a 1992-2013 study looking at the care pathways and cost-effectiveness of stroke in Indigenous and non-Indigenous adults in the NT, Aboriginal and Torres Strait Islander patients were shown to have fewer stroke-specific investigations such as imaging, but more non-specific investigations than non-Indigenous patients [54].
A study in Queensland found that there was a need for an inclusive coordinated and culturally responsive approach to Aboriginal and Torres Strait Islander stroke care that values the role of the client, their family and community [107]. The Aboriginal and Torres Strait Islander liaison officer was described as having a pivotal role in a multidisciplinary team. There was a need for resources specific to language, literacy and cultural needs of Aboriginal and Torres Strait Islander stroke survivors and advocacy for the availability and use of Aboriginal and Torres Strait Islander language interpreters. It was also found that Aboriginal and Torres Strait Islander stroke survivors had limited opportunity to fulfil their rehabilitation potential after hospital discharge.
Research about brain injury found that the absence of Aboriginal people in rehabilitation services has often led non-Aboriginal practitioners assuming that they don’t want therapy [108]. However, based on interviews with Aboriginal people in WA who have had a brain injury (due to a stroke, traumatic injury or fall), it was found that they want information about brain injury and more practical support for their rehabilitation.
There is a gap between Aboriginal and Torres Strait Islander and non-Indigenous people in terms of referral and uptake of stroke rehabilitation programs. The South Australian Heart and Stroke Plan 2017-2021 (SAHMRI) report notes that in 2013 and 2014, 28% of Aboriginal and Torres Strait Islander received referral to rehabilitation services as inpatients, compared with 34% of non-Indigenous patients [109]. Additionally, pre-discharge education is often poor and there are difficulties accessing stroke rehabilitation specialists in some areas.
Management of acute rheumatic fever and rheumatic heart disease
RHD is common in low- and middle-income countries and predominantly found in socioeconomically disadvantaged populations in high-income countries [10]. Both ARF and RHD are strongly linked to poor living conditions, such as overcrowding, poor access to clean drinking water, inadequate sanitation and sewage facilities, and poor access to healthcare [9]. Household overcrowding is a known contributor to increased risk of group A streptococcus infection [61]. In 2016, the highest proportion of overcrowding among Indigenous Australians was in the Nhulunbuy region, East Arnhem Land, NT, with 42% of surveyed households being classified as severely overcrowded. About 71% of all ARF cases are managed in regions with the highest rates of overcrowding including all NT regions; the Kimberley, W.A. and Torres Strait and Cape York, Qld.
Adherence is a persistent theme within chronic disease management in Aboriginal and Torres Strait Islander health, and is affected by: socioeconomic factors, geographical location, access to health services, and medication adverse effects [110]. Barriers to the control of ARF and RHD in Australia include: high health staff turnover, lack of awareness of ARF and RHD among health staff, and remoteness of the patient population [60].
Primary prevention of ARF and RHD focuses on preventing the ARF that leads to the RHD and can be divided into ‘primordial prevention’ and ‘primary prevention’ [9]. Primordial prevention focuses on the broad socioeconomic risk factors that lead to ARF, through measures that target the environment or social behaviours and alleviate poverty [9]. Changing environmental conditions can decrease carriage and transmission of group A streptococcus [9, 111]. This requires political commitment to address the underlying inequalities that underpin much of the health and life expectancy gap [89].
Primary prevention targets populations at elevated risk of group A streptococcus infection including Aboriginal and Torres Strait Islander people [9]. Accurate diagnosis and treatment of group A streptococcus infections can prevent ARF and subsequent RHD [112] with care being taken to diagnose skin infections which can be easily missed [113]. Antibiotic therapy is the mainstay of treatment for group A streptococcus infections, delivered as swiftly as possible and often via single intramuscular injection. Social recommendations include practising good hygiene and not sharing a bed when possible [114].
Following an episode of ARF, the chances of recurrence are high [10]. Secondary prevention of ARF and RHD involves avoiding recurrences of ARF and progression to RHD and is proven to be the best option in terms of efficacy and cost-effectiveness [110]. Onset of ARF is typically within 1-4 weeks of the start of infection [114]. Treatment of ARF is recommended alongside symptom management, using antibiotics, non-steroidal anti-inflammatories and anticonvulsants in the event of Syndenham’s Chorea (a clinical manifestation of ARF) [114].
The duration of secondary prevention is lengthy; a minimum of 10 years or until aged 21 years old – whichever is later – for those with no or mild RHD, until age 35 years for those with moderate RHD and until age 40 years for those with severe RHD [114]. Shortages of medication occur regularly and this creates difficulties with secondary prevention. The number of recurrences of ARF reflects inadequate secondary prophylaxis delivery [8].
In 2017, of Indigenous people who received secondary prophylaxis of benzathine penicillin G [10]:
- 394 people (15%) received 100% or more of their prescribed doses
- 548 people (21%) received 80% to 99% of their prescribed doses
- 964 people (37%) received 50% to 79% of their prescribed doses
- 724 people (28%) received less than 50% of their prescribed doses.
Indigenous people in the 15-24 year age group generally had lower adherence to secondary prophylaxis than other age groups, almost one third of this age group received less than half of their prescribed doses [10]. Almost half of those aged 5-14 years and more than half of those aged 45 years and over received at least 80% of their prescribed doses.
For those with established RHD, best practice recommendations include secondary prevention, anti-coagulation (if there is atrial fibrillation or valve replacement), diligent oral health care and regular cardiology follow-up [9]. Tertiary prevention focuses on medical management of RHD to prevent complications. A vaccine against group A streptococcus is in development [115, 116]. Clinical trials of prototypes are funded and underway [117].
A co-ordinated control program is the most effective approach to management of ARF and RHD and improving adherence to prophylaxis and secondary prevention measures [118]. Control programs: identify those at risk, support delivery of long-term prophylaxis, increase education among the workforce, provide education and self-management advice to patients, promote primary prevention and use information from disease monitoring to improve control program activities.
Audits of ARF/RHD records (2007-2009) for Aboriginal and Torres Strait Islander people in Far North Qld and WA demonstrated that only 55% had been reviewed by a specialist and only 61% had undergone echocardiography within recommended timeframes [119].
RHD may progress or regress over time and may present at varying levels of severity. A NT study of Aboriginal and Torres Strait Islander patients aged between 5 and 14 years, diagnosed with RHD in the period 1999-2012 found that of 96 patients with severe RHD at diagnosis, 50% proceeded to valve surgery by 2 years and 10% died within 6 years [120]. For those with moderate RHD, there was a similar chance of regression or progression over time. Those with mild RHD at diagnosis were the most stable with 64% remaining mild after 10 years however, 11% progressed to severe RHD and half of those required surgery.
Delivery of secondary prophylaxis in the NT is not adequate to prevent ARF. In response to this, a study tested a model of care to improve delivery of secondary prevention prophylaxis in ARF/RHD using multiple interventions such as activities to improve delivery of antibiotics and continuous quality-improvement feedback on adherence [110] [121].
That said, prophylaxis delivery has improved since 2014, when there was implementation of a recall system to avoid delays with injections [121].
In an ARF/RHD clinical audit using the ABCD (Audit and Best practice for Chronic Disease) ARF/RHD audit tool, data were collected for 2009 and 2014 from 63 Aboriginal centres
[122]. It was found that timely injections and patient education were important areas for improvement.
Owing to the length of treatment, there is strong need for culturally sensitive and appropriate engagement with patients to ensure long term follow-up [114]. A review that examined what self-management means in terms of ARF and RHD management for Aboriginal and Torres Strait Islander people identified five priority areas required for self-management to work [123] :
- improved clinical interaction/communication
- shared decision making
- knowledge transfer
- strengthened partnerships
- health services reform.
A community initiative in a remote Aboriginal community to work towards the elimination of RHD was based in ‘both-way learning’ with the aim to co-design, implement and evaluate community-based participatory action research (CBPAR) [124]. Activities related to understanding and addressing RHD social determinants were delivered through an accredited course and theory-driven evaluation linking CBPAR to empowerment was applied. The findings included the importance of valuing traditional knowledges and ways of learning, empowerment through critical thinking and community ownership of knowledge about RHD and research.
Collective action to address RHD is necessary [66]. RHDAustralia was established in 2009 to support the control of RHD. Separate RHD control programs have also been established in the NT, Qld, SA and WA, where each have priorities in terms of provision of service [118].
The National Health and Medical Research Council funded END RHD centre for research excellence (NHMRC END RHD CRE) is delivering a strategy to end RHD using a set of cost-effective interventions [66]. Six national bodies have formed the END RHD coalition: the Australian Medical Association (AMA), the National Heart Foundation of Australia, the National Aboriginal Community Controlled Health Organisation (NACCHO), RHDAustralia, Aboriginal Medical Services Alliance Northern Territory and END RHD CRE. The current target is to eliminate RHD in Australia by 2031 [125]. For improved monitoring and to assess prevention and treatment strategies, the END RHD in Australia: Study of Epidemiology (ERASE) Project aims to provide a comprehensive database of ARF and RHD cases in Australia and provides a baseline to assess improvements [126].
ARF recurrence is a key performance indicator (KPI) in ARF monitoring and prevention [127].
Key Performance Indicators (KPIs) for ARF/RHD include:
- ARF incidence by episode type
- ARF recurrences
- ARF and/or RHD deaths
- RHD point prevalence
- RHD incidence
- Secondary prophylaxis
- Priority levels of ARF and RHD cases (by age group)
- Echocardiograms performed – within designated timeframes – for priority levels 1 and 2
- Waiting times for RHD surgery
- Surgical procedures by type and patient age
- Mortality within 1 year of surgery by age category.
Risk and protective factors
There are many modifiable risk-factors for developing CVD and their interactions are complex as they reflect the impacts of historical, cultural and socioeconomic trauma and disadvantage [89]. The leading biochemical and behaviour factors are: smoking, physical inactivity, nutrition, alcohol consumption, overweight and obesity, depression, social and emotional wellbeing and comorbidity.
CHD events occur earlier in Aboriginal and Torres Strait Islander people than non-Indigenous contemporaries [45]. Studies that have demonstrated higher CHD incidence in Aboriginal and Torres Strait Islander people have also noted a greater likelihood of socio-economic disadvantage, whereas comparable non-Indigenous populations are more likely to be evenly distributed across the quartiles. Social and economic factors account for slightly more than one third of the ‘good health’ gap between Aboriginal and Torres Strait Islander people and non-Indigenous people when considering chronic disease [19]. Health risk factors such as high blood pressure, and risky alcohol consumption explain another 19%. It has been estimated that 11% of the total health gap can be attributed to the overlap, or interactions between social determinants and health risk factors [21].
CHD is largely preventable with a healthy, active lifestyle [128]. The strongest prevention methods include: smoking cessation, low/no alcohol consumption, a diet rich in fruit and vegetables and low in saturated fats, red meats and processed foods, and regular physical activity. Additionally, control of blood pressure and blood lipids with medications such as anti-hypertensives and statins can also decrease risk when prescribed appropriately [128].
Smoking
Tobacco use has a number of health impacts, including increasing the risk of chronic disease, such as CVD [32]. Components of cigarette smoke, particularly nicotine and carbon monoxide are involved in causing inflammation, changes in the lining of the blood vessels, dysregulation of blood sugar and changes in blood lipids (fats); all of which are integral causes of atherosclerosis and CVD [129, 130]. Cigarette smoking strongly and independently of other risk factors, increases the risk of developing CVD, even low-tar cigarettes significantly increase risk for smokers compared with non-smokers.
A prospective study of Australians aged ≥ 45 years from 2006 to 2009 with linked data to 2015 found that tobacco smoking cases damage across the entire cardiovascular system [131]. Smokers had at least double the risk of developing most significant types of CVD including AMI, cerebrovascular disease and heart failure and over five times the risk of developing peripheral arterial disease compared with people who had never smoked. Environmental tobacco smoke (passive smoking) is also of concern to health, with children particularly susceptible. Passive smoking in an environment with a smoker increases CVD risk by 30% [129].
Australia has one of the lowest prevalences of smoking globally [132]. However, prevalence is higher for Aboriginal and Torres Strait Islander people than non-Indigenous people. Smoking behaviour in Aboriginal and Torres Strait islander people is linked with the history of colonisation. Tobacco was historically offered as payment and included in rations on mission stations [133]. Smoking is strongly associated with social disadvantage, those with the most social disadvantage are more likely to smoke than those with the least; Aboriginal and Torres Strait Islander people are more likely to have lower educational achievement, lower income and be unemployed [130]. High levels of psychological distress, poor self-assessed health status and experience of one or more life stressors in the recent months have been associated with higher rates of smoking [134].
In the 2018-19 NATSIHS, there were 41% of Aboriginal and Torres Strait Islander people aged 15 years and over who were current smokers – 37% smoked every day and 3% smoked but not every day [35]. Of those who smoked daily (average 12 cigarettes per day), the proportions were similar for males (39%) and females (36%). The proportion of people who smoked daily was higher for people living in remote areas (49%) than in non-remote areas (35%). The proportion was lowest, almost 10%, for people aged 15-17 years compared with around 40% in all other age groups (see Table 14). The proportion of Aboriginal and Torres Strait Islander people aged 15 years and over who smoked daily decreased from 49% in 2004-05, to 41% in 2012-13 and to 37% in 2018-19, however, the proportion in remote areas did not change significantly. More than 22% of people aged 15 years and over were ex-smokers with rates higher in non-remote areas (24%) than in remote areas (15%).
Table 14. Daily smoking proportion (%) by sex and age group (years) 2018-19
| 15-17 | 18-24 | 25-34 | 35-44 | 45-54 | 55+ | |
|---|---|---|---|---|---|---|
| Males | 12 | 35 | 47 | 49 | 44 | 35 |
| Females | 8 | 36 | 41 | 45 | 41 | 32 |
| All | 10 | 36 | 44 | 47 | 42 | 33 |
Source: ABS, 2019 [35]
In 2018-19, the proportion of Aboriginal and Torres Strait Islander people aged 15 years and over who had never smoked was 37% (36% of males and 39% of females) (see Figure 4 for specific age groups), the proportion was higher in non-remote areas (40%) than in remote areas (29%) [35]. Since 2012-13, the proportion of young people who had never smoked increased from 77% to 85% for those aged 15-17 years and from 43% to 50% for those aged 18-24 years. There was no change in the overall proportion between 2012-13 and 2018-19 (both 37%).
Figure 4: Proportion (%) of Aboriginal and Torres Strait Islanders who have never smoked by age group, 2018-19
Source: ABS 2019 [35]
In 2014-2015, 57% of Aboriginal and Torres Strait Islander children aged 0-14 years lived in households with a daily smoker (a decline from 63% in 2008) [135]. For those children living with a daily smoker, 13% were living in households where people smoked indoors.
The National key performance indicators for Aboriginal and Torres Strait Islander primary health care reported that at June 2018, 52% of clients were current smokers [56].
High rates of smoking have been reported for Aboriginal and Torres Strait Islander mothers; however since 2009 the proportion of Aboriginal and Torres Strait Islander mothers who reported smoking during pregnancy has decreased from 52% in 2009 to 44% in 2017 [136]. Of those who smoked, the proportion of Indigenous mothers who quit smoking during pregnancy was 12%, based on mothers who reported smoking in the first 20 weeks of pregnancy and not smoking after 20 weeks of pregnancy.
In 2014-15, approximately 69% of Aboriginal and Torres Strait Islander smokers had attempted to quit in the previous 12 months and females were more likely to attempt to quit or ‘cut-down’ than males (72% versus 67%) [32]. Those aged 25-34 years were most likely to attempt quitting [32]. Reasons given for attempting to quit were: health, cost, fitness, pressure from family and medical advice [32]. The graphic warnings on cigarette packages have been shown to be a useful deterrent for Aboriginal and Torres Strait Islander smokers [137].
A 2012-13 survey of 2,522 Aboriginal and Torres Strait Islander people, of whom 1,643 were current cigarette smokers, demonstrated that most were aware of the major risks of smoking, such as lung cancer, CVD and low birthweight [138]. Smokers who responded ‘agree’ or ‘strongly agree’ to the statement “Smoking is not very risky when you think about all the things that people do”, were assessed as holding risk-minimising beliefs. Those who responded ‘very worried’ to the question “How worried are you that smoking will damage your health in the future?” were assessed as having health worry. Of current smokers, 44% held risk-minimising beliefs and 36% had health worry. Those aware of the risks of smoking were more likely to have attempted to quit. There was also a high level of knowledge regarding the risks of passive smoking for children.
Aboriginal and Torres Strait Islander people are significantly more likely to be hospitalised owing to smoking-related illnesses [139]. In 2004-5, 30% of current and 37% of former smokers reported having treatment for CVD [140].
In 2015, tobacco use was the leading risk factor that contributed to disease burden and deaths accounting for 9.3% of disease burden in Australia [141]. In 2011, tobacco use remained the leading cause of the burden of disease and injury among Aboriginal and Torres Strait Islander people, responsible for 12% of the total burden of disease [12]. It contributed around 40% of the disease burden to CVD, cancer and respiratory diseases. Tobacco use was also the risk factor contributing the most (23%) to the health gap between Aboriginal and Torres Strait Islander and non-Indigenous people. This disease burden is greater than any other risk-factor, including alcohol and illicit drugs combined [139].
The National Tobacco Strategy 2012-2018 outlines nine priority areas to tackle smoking rates in Aboriginal and Torres Strait Islander people [142]:
- Protect public policy from tobacco industry influence
- Strengthen mass media campaigns to:
- motivate smokers to quit
- discourage non-smokers to take up smoking
- reframe social smoking norms
- Continue to make tobacco products less affordable
- Build on partnerships to reduce smoking in Aboriginal and Torres Strait Islander people
- Increase efforts to reduce smoking in populations with a high prevalence
- Eliminate advertising and promotion of tobacco products
- Further regulation of tobacco contents and products
- Fewer exceptions to smoke-free places
- Greater access to support services for quitting tobacco.
The Tackling Indigenous Smoking (TIS) program (http://tacklingsmoking.org.au/about-the-tis-program) aims to improve the health of Aboriginal and Torres Strait Islander people by reducing the prevalence of tobacco use through population health promotion activities. The program has a number of parts:
- regional tobacco control grants (RTCGs) to organisations
- a National Best Practice Unit for Tackling Indigenous Smoking (NBPU TIS)
- a National Coordinator for Tackling Indigenous Smoking
- enhancements to Quitline services
- Quitskills training
- a focus on priority groups (including pregnant women and smokers in remote areas)
- an evaluation of the overall program (process and impact).
Physical activity
The concept of physical activity may be perceived differently by Aboriginal and Torres Strait Islander people compared with non-Indigenous people. As with many other lifestyle factors, the physical activity levels of Aboriginal and Torres Strait Islander people have been adversely affected by colonisation; prevention from accessing land, moving people into missions or towns and forcing a reliance on food-handouts, have decreased physical activity significantly, which combined with poor nutrition, have increased disease burden in this population [143].
The traditional lifestyle of Aboriginal and Torres Strait Islanders was highly active, consisting of hunting, gathering and walking [143]. These activities helped to build an important social structure; Westernised methods of exercising as an individual may be viewed as selfish or inappropriate. Prior to colonisation, sport was an important part of Aboriginal and Torres Strait Islander life, and currently traditional sports are undergoing a revival under consultation with Elders who remember the rules and the National Aboriginal Sporting Chance Academy. Traditional games are inclusive rather than competitive and have the added benefit of showing the strength and survival of Aboriginal culture.
Physical activity is important for maintaining good overall health and wellbeing [144]. Low levels of activity, including high levels of sedentary behaviour are risk factors for a range of health conditions as well as being a strong contributor to obesity. Australia’s physical activity and sedentary behaviour guidelines for adults recommend a combination of moderate and vigorous physical activity on most, preferably all, days of the week to improve health and reduce the risk of chronic disease and other conditions. However, doing some physical activity is better than doing none and the health benefits of being physically active are continuous, starting with any activity above zero [145]. Regular physical activity reduces the risk of many health problems including CVD [144]. For those with existing cardiac disease, it is recommended that they should consult their doctor for an individualised physical activity plan [146].
Physical inactivity is an important risk factor in the development of CVD, especially for CHD, stroke and heart failure [71]. Physical activity reduces the impact of other CVD risk factors such as overweight/obesity, hypertension, stress, cholesterol and type 2 diabetes mellitus. In addition to lack of physical activity, extended time sitting is also associated with increased mortality [147]. In 2011, physical inactivity accounted for 5.5% of the total burden of disease for Aboriginal and Torres Strait Islanders and 8.2% of the health gap [32]. It is the fourth leading risk factor for the Aboriginal and Torres Strait Islander population (following smoking, alcohol and overweight/obesity). Approximately 44% of the CHD disease burden is related to physical inactivity [32].
In the 2018-19 NATSIHS, 11% (13% of males and 9.7% of females) of Aboriginal and Torres Strait Islander people over the age of 15 years in non-remote areas met the 2014 physical activity guidelines and 89% did not meet the guidelines [35]. More than 22% (20% of males and 23% of females) had done no physical activity in the past week.
In the 2012-13 AATSIHS, people who participated in the survey’s pedometer study recorded an average of 6,963 steps per day; 17% met the recommended threshold of 10,000 steps or more [148]. In remote areas, 55% of adults exceeded the recommended 30 minutes of physical activity [148]. The most common type of physical activity for adults was ‘walking to places’ (71%). Around one-in-ten (11%) participated in cultural activities, including hunting and gathering bush foods or going fishing.
In 2012-13, on average, Aboriginal and Torres Strait Islander adults engaged in around one third the amount of physical activity as children aged 5-17 years (39 minutes per day including 21 minutes on walking for transport) [148]. Aboriginal and Torres Strait Islander children aged 5-17 years living in non-remote areas spent an average of two hours per day participating in physical activity (exceeding the recommendation of one hour per day); this was 25 minutes more than non-Indigenous children. Around half (48%) of Aboriginal and Torres Strait Islander children met the recommended amount of physical activity, compared with 35% of non-Indigenous children. For Aboriginal and Torres Strait Islander children aged five years and over in remote areas, 82% did more than 60 minutes of physical activity on the day prior to the interview. Other than walking (82%), the two most common activities were running (53%) and playing football or soccer (33%). Aboriginal and Torres Strait Islander children aged 2-4 years living in non-remote areas spent an average of 6.6 hours per day participating in physical activity and spent more time outdoors than non-Indigenous children in the same age group (3.5 hours compared with 2.8 hours) [148]. Aboriginal and Torres Strait Islander children aged 2-4 years spent an average of 1.5 hours per day on sedentary screen-based activities such as watching TV, DVDs or playing electronic games.
A study in NSW found that Aboriginal and Torres Strait Islanders most likely to engage in the recommended physical activity levels are typically in the younger age bracket [149].
A notable barrier to physical activity for Aboriginal and Torres Strait Islander people is systematic racism and limited participation resulting in fewer athletic role models for young Aboriginal and Torres Strait Islander people [150]. However, physical activity can be a vital part of youth development for Aboriginal and Torres Strait Islander young people; encouraging empowerment and understanding of traditional culture and values. Additionally, a study found in a physical activity and nutrition program for women that aspects such as lack of transport and family commitments are also significant barriers for Aboriginal and Torres Strait Islander people engaging in physical activity [151].
Neighbourhoods and social environments are known to influence participation in physical activity. Aboriginal and Torres Strait Islander people – particularly those living in remote communities – are 10% less likely than non-Indigenous people to meet physical activity recommendations [149]. The neighbourhood and built environment directly impact on the ability to be physically active; enabling or disenabling walking, cycling and team sports. Neighbourhood environments with lower crime rates and better social support are most conducive to achieving the recommended physical activity levels.
Nutrition
The diet of Aboriginal and Torres Strait Islander people has changed since the time of colonisation, from traditional diets that were high in protein, fibre, polyunsaturated fat and complex carbohydrates to a more highly refined carbohydrate diet, with added sugars, saturated fat, sodium and low levels of fibre [152]. Traditional foods remain an important part of the diet for many people, strongly linked to identity, culture and country. The nutritional status of Aboriginal and Torres Strait Islander people is influenced by many factors such as socioeconomic disadvantage, and geographical, environmental and social factors [153]. Poor nutrition is an important factor contributing to CVD and related to other risk factors such as overweight and obesity [153, 154]. Good nutrition is one of the most vital aspects for preventing chronic diseases [12]. An AIHW report stated that there is little difference between the food and nutrient intakes and health outcomes of Aboriginal and Torres Strait Islander people and non-Indigenous Australians [155]. Approximately 72% of CVD deaths are attributable to poor diet [156].
The 2011 Australian Burden of Disease study considered the contribution of 29 selected risk factors to the burden of disease, of which 13 risk factors were dietary [12]. When combined, the joint effect of all dietary risks contributed 9.7% to the total burden of disease for Aboriginal and Torres Strait Islander people. The contribution of dietary risk factors to the burden of disease was particularly notable in the 65 years and over age-group, with a diet low in fruit contributing 4% to the burden for Aboriginal and Torres Strait Islander males and 3% for Aboriginal and Torres Strait Islander females.
The Australian dietary guidelines recommend that adults eat fruit and plenty of vegetables every day, selected from a wide variety of types and colours [154]. Current dietary guidelines emphasise an abundance of fresh vegetables with fresh fruits, whole grains, protein, nuts/seeds and vegetable oils (preferably non-refined/extra virgin olive oil)
[154, 156]. The guidelines also recommend including reduced fat varieties of milk, yoghurts and cheeses, and limiting the intake of added sugar and salt and the consumption of ‘discretionary’ foods and drinks [154]. Recent years have shifted the focus from quantity to quality of food, with a focus on whole foods and reduction of processed food, saturated fats and refined carbohydrates
CVD prevention can be promoted by a variety of diets, including: a whole food plant based diet [158], the Mediterranean diet, a low-fat diet, a low-carbohydrate diet and the DASH (Dietary Approaches to Stop Hypertension) diet [159]. All of these diets overlap with one another yet all show promise for reducing CVD burden. A resounding similarity between all is a focus on eating large quantities and varieties of fresh fruit and vegetables and few saturated fats, processed foods and refined sugars. Consumption of anti-inflammatory foods to reduce risk of type 2 diabetes, the metabolic syndrome and subsequent CVD is also favourable, including foods high in polyphenolic compounds such as tea, berries and citrus fruits [160].
Across Australia, adherence to dietary guidelines is poor in both Aboriginal and Torres Strait Islanders and non-Indigenous populations, with under-consumption of whole-food fruits, vegetables and whole grains and over consumption of processed foods, saturated fats, salt and refined sugar [154]. The social reasons for this are complex and include food security aspects such as availability of fresh food and affordability, which is more challenging in remote locations [161], poor health literacy, social factors and conflicting dietary advice [154]. The recommended kilojoule intake per day in Australia, for the average adult, is approximately 8,700 kJ. Aboriginal and Torres Strait Islander males consume, on average, 9,175 kJ and females consume on average 7,261 kJ [162].
In the 2018-19 NATSIHS, 39% of Aboriginal and Torres Strait Islander people aged 15 years (44% of females and 35% of males) and over met the guidelines for the recommended number of serves of fruit per day [35]. The proportion was lower than in 2012-13 (43%). The proportion was about the same for people living in non-remote areas (39%) and remote areas (42%). The proportion of Aboriginal and Torres Strait Islander people aged 15 years and over who had consumed the recommended number of serves of fruit per day declined for those living in remote areas from 49% in 2012-13 to 42% in 2018-19. For children, 69% of those aged 2- 14 years met the 2013 dietary guidelines for the recommended number of serves of fruit per day.
In 2018-19, 4% of Aboriginal and Torres Strait Islander people aged 15 years and over (6% of females and 2% of males) met the 2013 dietary guidelines for the recommended number of serves of vegetables per day [35]. The proportions were the same for those living in non-remote and remote areas (both 4%). The proportion was the same as in 2012-13 (both 4%). For children, 7% of those aged 2-14 years met the guidelines for the recommended number of serves of vegetables per day.
In the 2012-13 NATSINPAS for vegetable intake, it was reported that Aboriginal and Torres Strait Islander children (2-18 years) averaged 1.4 serves of vegetables a day and adults (aged 19 years and over) averaged 2.1 serves per day [163]. The food group consumed by most Aboriginal and Torres Strait Islanders was the cereals and grains group, including breads [162]. Approximately 87% of Aboriginal and Torres Strait Islander people reported consuming cereal products in the week prior to survey. Out of all meat products, processed meats were the most commonly consumed, followed by red meats such as beef and pork. Those living remotely derived a greater number of calories from meat than those living in more urbanised areas.
In the 2012-13 NATSINPAS, discretionary foods (foods low in nutritional value but high in salt, sugar and saturated fats) were consumed by a large proportion of Aboriginal and Torres Strait Islander people in the 24 hours prior to the survey, including confectionary (25%), snack foods (20%) and alcoholic beverages (11%) [164]. On average, Aboriginal and Torres Strait Islander people consumed 41% of their total daily energy in the form of discretionary foods; including 8.8% of daily energy as cereal-based products (such as cakes, biscuits and pastries), and 6.9% of daily energy as non-alcoholic beverages (such as soft drinks) [162]. Similar proportions of females and males consumed all discretionary foods except for alcoholic beverages for which twice as many males as females reported consuming (15% and 7.7% respectively) [164]. People in non-remote areas were more likely to consume all discretionary foods types than those in remote areas, except for non-alcoholic beverages (99% of people in both non-remote and remote locations).
Refined sugar consumption is high among Aboriginal and Torres Strait Islander people; with an average consumption in those aged 2 years and older of 18 teaspoons of sugar per day (75g) [17]. The WHO recommends that both adults and children consume less than 10% of daily dietary energy from free sugars [165]. According to the 2012-13 NATSINPAS, Aboriginal and Torres Strait Islander people consumed 111 grams (g) of total sugars per day on average [157]. Males consumed more totals sugars on average than females (121 g compared with 101 g) especially in the 14-18 years age-group (147 g compared with 102 g). The variation in sugar consumption across age and sex was mostly due to the consumption of free sugars as the amount of intrinsic and milk sugars consumed remained relatively constant across all age and sex groups. The majority of free sugars consumed were from discretionary foods and beverages.
In the 2018-19 NATSIHS, 24% of Aboriginal and Torres Strait Islander people aged 15 years and over reported that they usually consumed sugar sweetened drinks every day and 6% consumed diet drinks; 71% (75% of males and 67% of females) usually consumed sugar sweetened drinks or diet drinks at least once per week [35]. For children aged 2-14 years, 20% usually consumed sugar sweetened drinks daily and 2% consumed diet drinks daily; 63% usually consumed sugar sweetened drinks or diet drinks at least once a week. The proportion of people who usually consumed sugar sweetened or diet drinks was higher for people living in remote areas (77%) than for non-remote areas (69%). The proportion was lowest for those aged 45-54 years (63%) and 55 years and over (49%), compared with 80% for people aged less than 45 years.
Infant nutrition is of vital importance, setting good dietary habits for life. Inadequate nutrition in pregnancy is associated with growth retardation in babies [32]. Within Aboriginal and Torres Strait Islander communities, infant malnourishment, underweight and failure to thrive remain significant problems which can continue to affect health for the duration of life [17]. Breastfeeding is known to incur several health benefits for the infant superior to formula milk, including decreased chronic disease risk. In 2012-13, 83% of Aboriginal and Torres Strait Islander infants had been breastfed, versus 93% of non-Indigenous children. Aboriginal and Torres Strait Islander infants however, were less likely than non-Indigenous infants to have been breastfed for one year or more (12% versus 21% respectively) [17].
Food security is one of the largest barriers for Aboriginal and Torres Strait Islander people to meeting recommended dietary guidelines and those living in rural or remote areas are particularly vulnerable for reasons such as poverty, over-crowding of houses, low-income and lack of access to nutritious, affordable food. Food-security is recognised as a fundamental human right and within Australia there is not enough being done to ensure food-security for Aboriginal and Torres Strait Islander people [161].
The 2012-13 NATSINPAS addressed the issue of food security by asking respondents if they had run out of food and couldn’t afford to buy more in the last 12 months [166]. This had been a problem for 22% of respondents; 7% of respondents had run out and gone without food, while 15% had run out but not gone without food. People in remote areas were more likely to run out of food than people in non-remote areas (31% and 20% respectively) and slightly more likely to go without (9.2% and 6.4% respectively). A study conducted in urban settings identified that food insecurity is intermittent, occurring especially when large household bills are due for payment [167].
Healthy food items in remote settings are often priced highly, providing a further barrier to accessible healthy eating. A study conducted in a remote North Queensland Aboriginal and Torres Strait islander community investigated the use of food vouchers for fruit and vegetables to promote healthy eating behaviours [168]. Whilst several barriers to implementation and success were noted such as poor infrastructure for promotion, frequent store closures and poor staffing, it was shown that populations subgroups, such as mothers with children, were particularly receptive to the program. This demonstrates the value of consumer subsidy schemes, particularly in settings with socioeconomic disadvantage
It has been estimated that 80,000 Aboriginal and Torres Strait Islander people live in remote communities with poor access to fresh, nutritional food [161]. Improving nutrition among Aboriginal and Torres Strait Islanders will involve addressing food security and the underlying social injustice.
Overweight and obesity
There is a strong association between excess body weight and a variety of conditions including atherosclerosis, hypertension, raised blood cholesterol, cardiovascular disease and type 2 diabetes mellitus [169]. Obesity affects the heart via altered blood cholesterol, hypertension, insulin resistance and inflammation [170].
Overweight and obesity are complex issues, caused by interlinked factors including genetics and epigenetics, metabolism, behaviours, socio-economic status, culture and environment [171].
Evidence shows that those living in poverty or living with food insecurity are more likely to purchase and consume food that gives the most calories for the least monetary cost; often the most processed and energy dense foods [32]. Financial stress in the long-term is a predictor of obesity as low-income is associated with food insecurity and poor food-choices [32]. Those living with food insecurity often simultaneously suffer overweight and obesity. Obesity is strongly linked to other determinants of health and socioeconomic factors. It is also linked with social and emotional wellbeing and comorbidity.
Obesity is a major contributor to the morbidity and mortality gap between Aboriginal and Torres Strait Islander people and non-Indigenous people and the problems often begin in childhood. Childhood is a critical period for problems related to social inequalities to present. Both underweight and overweight are more common in Aboriginal and Torres Strait Islander children than in non-Indigenous children [32].
The most common measure for classifying a person’s weight status is body mass index (BMI) (BMI: weight in kilograms divided by height in metres squared) or by measuring their waist circumference (WC) [172]. Being overweight (BMI 25 to 29) or obese (BMI of 30 or more) [172], increase a person’s risk for CVD [173] A high BMI can be a result of many factors, alone or in combination, such as poor nutrition, physical inactivity, socioeconomic disadvantage, genetic predisposition, increased age and alcohol use [154, 174]. Abdominal obesity, a risk factor for the development of metabolic syndrome, can be measured by WC alone (greater than 94 cm for males and greater than 80 cm for females), or waist-hip ratio (WHR) (greater than or equal to 0.90 for males and 0.85 for females) [175]. Obesity and abdominal obesity, as measured by BMI and WC, have been shown to be risk factors for hypertension [176] including for Aboriginal and Torres Strait Islander people [177]. However, optimal BMI and WC cut-offs are still uncertain for Aboriginal and Torres Strait Islander people (due to differences in body shape and other physiological factors) when calculating cardiovascular risk [178-180]. In the 2018-19 NATSIHS, 71% of people (81% of females and 60% of males) aged 18 years and over had a measured waist circumference that put them at increased risk of developing chronic disease; the highest proportion was for people aged 55 years and over (86%) [35].
In the 2018-19 NATSIHS, 71% of Aboriginal and Torres Strait Islander people aged 15 years and over were overweight (29%) or obese (43%), 25% were normal weight and 4% were underweight [35]. The proportion for obesity was higher for females (45%) than the proportion for males (40%) but there were no significant differences for males and females for overweight, normal weight and underweight (see Table 15). The proportion for overweight/obese was higher for people living in non-remote areas (73%) than for those living in remote areas (64%). There was an increase with age for overweight/obese proportions from 42% for 15-17 years to 80% for people aged 35-44 years and over. More than half (54%) of children aged 2-14 years were in the normal weight range, 24% were overweight, 13% were obese and 9% were underweight. There was an increase in the proportion of children who were overweight or obese from 30% in 2012-13 to 37% in 2018-19.
Table 15: Proportion (%) of overweight/obesity in Aboriginal and Torres Strait Islanders by sex and age (years), 2018-19
| Age |
Underweight |
Normal |
Overweight |
Obese |
|---|---|---|---|---|
|
Males |
||||
| 15-17 |
3.1 |
53 |
27 |
18 |
| 18-24 |
10 |
34 |
26 |
31 |
| 25-34 |
1.4 |
27 |
33 |
40 |
| 35-44 |
1.5 |
17 |
35 |
46 |
| 45-54 |
2.4 |
19 |
30 |
50 |
| 55+ |
2.0 |
15 |
32 |
52 |
| All men 15+ |
3.2 |
26 |
31 |
40 |
|
Females |
||||
| 15-17 |
14 |
46 |
22 |
18 |
| 18-24 |
5.9 |
34 |
27 |
33 |
| 25-34 |
4.3 |
23 |
23 |
49 |
| 35-44 |
1.4 |
18 |
29 |
52 |
| 45-54 |
2.5 |
15 |
30 |
54 |
| 55+ |
2.9 |
16 |
30 |
51 |
| All women 15+ |
4.5 |
24 |
27 |
45 |
Source: ABS 2019 [35]
According to the 2018-19 NATSIHS, based on BMI information, around 40% of Aboriginal and Torres Strait Islander children aged 2-14 years were either overweight (27%) or obese (13%), 53% were in the normal weight range, and 7% were underweight [35]. More girls aged 2-14 years were overweight or obese than boys (34% and 40% respectively).
Physical activity and overweight and obesity are linked; in 2012-13, those who did not meet the guidelines for physical activity were more likely to be obese (44%) than those who did (36%) [32].
In 2017, the national key performance indicators for Aboriginal and Torres Strait Islander primary health care services reported that, of regular clients attending services aged 25 years and over, 71% were either overweight or obese (27% were overweight and 44% were obese) in the previous two years [181]. More females were overweight or obese than males across all age groups. However, the percentage of regular clients classified as obese rose with age for both males and females up until around 64 years, then fell slightly thereafter. Overall, more than half of the organisations (114 of 214) reported 73% of their clients, 25 years and above, to be overweight or obese.
Alcohol consumption
The historical context should be considered when observing patterns of Aboriginal and Torres Strait Islander alcohol consumption [182]. Alongside issues highlighted above, with trauma, racism, significant social disadvantage and marginalisation, historically alcohol was a ‘cornerstone’ of colonialism and was often used with Aboriginal and Torres Strait Islander people in exchange for labour or sex. As its use became commonplace, many Aboriginal and Torres Strait Islanders sought solace and enjoyment in alcohol and the consequences have been far-reaching. Restrictions subsequently placed on Aboriginal and Torres Strait Islander alcohol consumption have resulted in riskier patterns of drinking, including ‘binge’ drinking when alcohol can be obtained [182]. Binge-drinking is associated with high risks of developing CVD [183]. The 2011 Burden of Disease study estimated that harm from alcohol accounts for 8% of the total burden of disease and injury for Aboriginal and Torres Strait Islander people [12].
Trauma is linked to post-traumatic stress disorder, and in Aboriginal and Torres Strait Islander people this has been linked with high-risk alcohol consumption [184]. Excess alcohol consumption has adverse impacts on Aboriginal and Torres Strait Islander communities. In 2014-15, 19% of Aboriginal and Torres Strait Islander people aged 15 years and older reported that alcohol was a family stressor and this problem appears exacerbated by remoteness [32]. Evidence suggests that Aboriginal and Torres Strait Islander people have better health outcomes when there are adequately resourced and culturally safe alcohol and other drug (AOD) services provided by community controlled organisations [185, 186].
There is ongoing debate on whether there is: a ‘safe’ level of alcohol consumption; if some alcohol consumption helps prevent CVD; and whether all levels of alcohol consumption contribute to the development of CVD. Systematic reviews show that alcohol in moderation can reduce the risk of vascular disease, but is also correlated with increased mortality particularly in younger adults, consequentially, care should be taken when advising on ‘safe’ alcohol consumption levels [187]. Other research also shows that alcohol can have adverse effects on blood cholesterol and could increase the risk of CVD [188].
The current guidelines from the 2009 NHMRC seek to estimate the overall risk of alcohol-related harm over a person’s lifetime [189]:
- Guideline 1 states that to reduce the risk of alcohol-related harm over a lifetime, no more than two standard drinks should be consumed on any day.
- Guideline 2 states that to reduce the risk of injury on a single occasion of drinking, no more than four standard drinks should be consumed.
- Guideline 3 recommends that the safest option is not drinking alcohol for those aged under 15 years and delaying alcohol use for as long as possible for those aged 15 to 17 years.
- Guideline 4 recommends that the safest option for pregnant and breastfeeding women is not to drink alcohol.
The Draft Australian guidelines to reduce health risks from drinking alcohol were released for consultation in December 2019 and recommend not drinking more than 10 standard drinks per week [190]. The guidelines also recommend that those younger than 18 years don’t drink at all, and that women who are pregnant or planning to have a baby avoid alcohol.
Alcohol consumption in Aboriginal and Torres Strait Islander people is proving detrimental to the health of the population, however, Aboriginal and Torres Strait Islander people are less likely to drink alcohol than non-Indigenous people, but those who do drink are more likely to at levels that cause harm [32, 191].
In the 2018-19 NATSIHS, 26% of Aboriginal and Torres Strait Islander people aged 18 years and over reported that they did not drink alcohol in the previous 12 months or had never consumed alcohol (15% had not consumed alcohol in the previous 12 months and 11% had never consumed alcohol); females were more likely (31%) to have not consumed alcohol in the previous 12 months or to have never consumed alcohol than males (19%). Aboriginal and Torres Strait Islander people living in remote areas were more likely (37%) to have not consumed alcohol in the previous 12 months or had never consumed alcohol than those living in non-remote areas (23%). The proportion that did not drink alcohol in the previous 12 months or had never consumed alcohol was higher in 2018-19 (26%) than in 2012-13 (23%).
In 2018-19, more than half (54%) of Aboriginal and Torres Strait Islander people aged 18 years and over had exceeded the single occasion guideline (more than four standard drinks on one occasion in the last 12 months) with males more likely (65%) to exceed the guideline than females (43%) [35]. The proportion was lower for people aged 55 years and over (34%) than for any other age group; the proportion for males in this age group (47%) was higher than for females (23%). The proportions were about the same for people living in non-remote areas (54%) and remote areas (53%). The proportion of people who had exceeded the single occasion guideline was lower than in 2012-13 (57%). For those aged over 18 years who had exceeded the lifetime risk, 20% had consumed more than two standard drinks per day on average (about the same as for 2012-13 (20%)); about the same for those living in non-remote areas (21%) and remote areas (17%). The proportion of people who had exceeded the lifetime risk guideline was three times higher for males (30%) than for females (10%).
Social and emotional wellbeing
For Aboriginal and Torres Strait Islander people, the term ‘social and emotional wellbeing’ is used to encompass the social, cultural, spiritual and emotional wellbeing of an individual or community [32]. Differentiated from mental health, Aboriginal and Torres Strait Islander people take a holistic view of health and believe the term ‘mental health’ focuses too much on problems and not enough on factors such as culture that can also impact on social and emotional wellbeing [192]. Factors that appear to impact adversely on Aboriginal and Torres Strait Islander social and emotional wellbeing include: socioeconomic disadvantage, loss of culture, breakdown of traditional family and kinship structures, fear and lack of education, historical factors, racism and loss [192, 193]. The impacts of these factors both directly on individuals and as a result of intergenerational trauma owing to loss of land, incarceration and forcible separation of families, have strongly and adversely affected Aboriginal and Torres Strait Islander health [32]. Indeed, Aboriginal and Torres Strait Islander people report higher levels of emotional distress, self-harm and suicide than any other Australians.
Cardiovascular health is intrinsically linked with social and emotional wellbeing. Studies have demonstrated that strong negative emotions such as fear, anger, stress, anxiety or depression can precipitate heart disease, particularly CHD [194]. Sudden, profound emotional distress has been observed to precipitate heart failure in those previously free from heart disease.
Additionally, there is an 80% chance of developing CVD in adults diagnosed with depression with or without prior cardiac conditions [195]. Conversely, positive emotions, optimism, social support, and life satisfaction appear to be protective against CVD, associated with healthy immune systems and lower levels of inflammation. Additionally, those who experience positive emotions are more likely to engage in healthy behaviours such as a good diet and exercise [196].
The relationship between emotional wellbeing and CVD is complex and it is believed that depression accelerates the onset of atherosclerosis and additionally exacerbates or promotes risk factors such as hypertension, obesity, altered blood cholesterol and diabetes [195]. One of the most significant ways in which depression impacts the cardiovascular system is via lifestyle; depression increases the risk of unhealthy lifestyle behaviours such as smoking, alcohol intake, poor diet, sedentary lifestyles and decreased compliance with medications. Social support is fundamental in combating depression and associated CVD. The absence of social or marital support in the presence of depression and CVD is a poor prognostic indicator and may be predictive of adverse outcomes [197].
In the 2018-19 NATSIHS, 24% of Aboriginal and Torres Strait Islander people aged two years and over reported having a mental or behavioural condition: proportions were about the same for males (23%) and females (25%) [35]. The proportion was three times higher for people living in non-remote areas (28%) than in remote areas 10%. Anxiety was the most common (17%) mental or behavioural condition: proportions were higher for females 21% than males (12%). Depression was the second most common (13%): proportions were higher for females (16%) than for males (10%).
In 2018-19, 31% of Aboriginal and Torres Strait Islander people aged 18 years and over reported that they had experienced high or very high levels of psychological distress: the proportion for females (35%) was higher than for males (26%) [35]. Proportions were about the same for those living in non-remote areas (31%) and remote areas (28%).
In the 2014-15 National Aboriginal and Torres Strait Islander Social Survey, 33% of Aboriginal and Torres Strait Islander people aged over 15 years reported high or very high levels of psychological distress [135]. After age-adjustment, Aboriginal and Torres Strait Islanders were 2.6 times more likely than non-Indigenous people to suffer high levels of psychological distress. The most common sources of life stress were reported to be: death of a family member/close friend, unemployment, serious illness and mental illness.
Future directions
National policies and strategies have been developed to improve the health of Aboriginal and Torres Strait Islander people. The Aboriginal and Torres Strait Islander Health Plan 2013-2023 overarches these, linking commonwealth frameworks with an aim to identify areas of focus and reduce racism and inequality, providing health services to Aboriginal and Torres Strait Islander people that are effective, high-quality, appropriate and affordable [198]. Theintention of the Implementation for the Aboriginal and Torres Strait Islander Health Plan 2013-2023 is to progress strategies and actions that improve outcomes for Aboriginal and Torres Strait Islander people .
Below is a selection of some of policies and strategies across Australia currently; this list is by no means exhaustive.
National Strategic Framework for Chronic Conditions
This framework follows the 2005 National Chronic Disease Strategy and the National Service Improvement Frameworks as the largest Australian policy for tackling chronic disease; including CVD [199]. The strategy has three core objectives which are very similar to those outlined in specific CVD strategies at a state-wide level;
- Prevention
- partnerships for health
- health promotion/risk reduction
- timely and appropriate disease detection and intervention.
- Efficient, effective, appropriate care to those with chronic conditions to optimise life quality
- active engagement
- continuity of care
- accessible health services
- information sharing
- supportive systems.
- Target priority populations
- Aboriginal and Torres Strait Islander people
- action and empowerment.
This strategy is not specific to Aboriginal and Torres Strait Islander people but highlights them as a priority group and builds on the closing the gap approach, recognising the importance of the social and cultural determinants of health. This over-arching strategy can assist with management of CVD in Aboriginal and Torres Strait Islanders owing to the focus on improving all health-outcomes for Aboriginal and Torres Strait Islander people, however there is a need for further funding to achieve strategic implementation [200].
Rheumatic Fever Strategy, 2009 Onwards (RFS)
It is proven that the best way to improve adherence to secondary prevention programs, is via register-based strategies [110]. The RFS focuses on secondary prevention via state-based registers and control programs to improve detection, management and monitoring and national co-ordination to develop education and training materials [127]. The RFS National Partnership Agreement began in 2009 with the purpose of building infrastructure and capacity for secondary prevention (prophylaxis) against ARF and RHD. Each participating state/ territory has a control plan and register for ARF and RHD. Evaluation of the strategy in 2017 demonstrated several key achievements including:
- improved ARF and RHD monitoring and surveillance
- increased ARF and RHD awareness
- increased registration of patients
- increased prescribing of prophylaxis
- a developed data-collection system
- improved ARF and RHD incidence and prevalence rates.
However, it was noted that work was required within states/territories to refine their programs and tackle areas of challenge such as staff retention, improvements in detection rates in primary care, strategies to reduce the discomfort of injections and introduction of primordial and primary prevention strategies [127]. Future opportunities for the strategy include:
- a stronger role for primary care in diagnosis, management and surveillance of ARF and RHD
- development of clinical education for detection and management of ARF and RHD
- improved strategies to engage and educate patients and carers
- use of My Health Record to benefit patients who travel across services
- introducing primordial and primary prevention strategies
- vaccine development for group A streptococcus.
In 2018, it was announced that with a new round of Commonwealth funding, the Rheumatic Fever Strategy and RHD Australia were shifting direction with a new mission statement and strategy, currently in development, however, once again implementation and success will likely be funding dependent.
The Australian Government provides funding under the Rheumatic Fever Strategy to support RHD control programs in Qld, WA, SA and the NT [10].
These programs:
- identify people with or at risk of ARF and RHD
- promote primary prevention of ARF
- support the delivery of long-term secondary prevention treatment
- increase awareness of ARF and RHD among health professionals, and provide education about these diseases to health professionals, patients and their families and communities
- maintain disease registers for people diagnosed with ARF or RHD, and use this information to monitor health outcomes and improve control program
Cardiac Health Strategies
Many of the states/territories have their own individual strategy to tackle heart disease in Aboriginal and Torres Strait Islanders (Table 16), with some focussing on improvement in prevention and diagnosis and others on rehabilitation.
Table 16: A summary overview of heart disease strategies for Aboriginal and Torres Strait Islanders by State/Territory
| State/Territory | Goals/Targets | Priorities/ Action Areas |
|---|---|---|
| Qld Queensland Aboriginal and Torres Strait Islander cardiac health strategy 2014-2017. [201] |
Reduce the gap in mortality from CVD.
Improve health literacy and support self-management. Reduce rates of progression in RHD. Improve cardiac health care to reduce costs on health system. |
Early CVD risk assessment and management.
Timely diagnosis of heart disease/failure. Guideline based therapy for acute coronary syndrome. Optimisation of health status and ongoing preventative care. Strengthen diagnosis, management and follow-up of ARF and RHD.
|
| NT Cardiac rehabilitation and secondary prevention: a framework for the Northern Territory. [202]Note: this policy is not specific to Aboriginal and Torres Strait Islander people |
Provide direction for a multidisciplinary approach to cardiac rehabilitation.
Facilitate systems to provide timely access to secondary prevention services. Facilitate communication across all stakeholders of rehabilitation. Facilitate development of educational resources. |
Phase 1: Hospitalisation:
Phase 2: Discharge until physical, psychological and emotional stabilisation:
Phase 3: Ongoing completion of outpatient phase:
|
| SA South Australian Aboriginal heart and stroke plan 2017-2021. [109] |
Reduce age-standardised mortality rate from CVD.
Increase identification and management of those with high CVD risk. Reduce re-admission rate following CVD event. |
Governance and systems co-ordination.
Sustainable funding. Sustainable workforce development. Transport and accommodation support. Information and communications technology solutions. Monitoring and evaluation. |
| NSW Better cardiac care for Aboriginal and Torres Strait Islander people. [203] | Reduce mortality and morbidity from cardiac diseases.
Increase access to services. Improve management of risk factors. Improve co-ordination of care |
Early CVD risk assessment and management.
Timely diagnosis of heart disease/failure. Guideline based therapy for Acute Coronary Syndrome. Optimisation of health status and ongoing preventative care. Strengthen diagnosis, notification and follow up of ARF and RHD. |
| Vic Heart health: improved services and better outcomes for Victorians. [204] Note: this policy is not specific to Aboriginal and Torres Strait Islander people |
Improved care and better outcomes for Victorians with or at risk of CVD. | Promote healthy living and improve detection of those at risk of CVD.
Improved access to time-critical cardiac care. Improve services for people with heart disease. Strengthen system performance. |
Heart Foundation of Australia
The Heart Foundation of Australia made a submission of recommendations for the 2018-19 Budget to tackle heart disease within Australia and to save lives and money (see Table 17) [101].
Table 17: Recommendations from the Heart Foundation of Australia for tackling CVD
| Recommendation | Rationale |
|---|---|
| Develop a National heart and stroke action plan. | Develop a heart and stroke action plan to address key gaps in the current approach to cardiovascular disease prevention and care. It would support recommendations in the National Strategic Framework for Chronic Conditions [199] and aligns with the Government’s long-term health plan. |
| Build a comprehensive approach to prevention | Develop a coordinated approach to physical activity and healthy nutrition and decrease in smoking. |
| Detect and manage those at risk. | Inclusion of an integrated health check and ongoing management of patients at risk will aid development of a new, quality-focussed Practice Incentive Program. Combining risk assessment into integrative health checks will help ensure relevant risk assessment is performed in primary care. This will help improve detection of those at risk of CVD and improve management of that risk. |
| Renew absolute risk management guidelines | The absolute risk management guidelines developed by the National Vascular Disease Prevention Alliance are now due for review. Funding should be provided to ensure this takes place as soon as practicable. |
| Support women and heart disease campaign | Support women and heart disease campaign, $4M over 3 years to save lives and reduce suffering caused by a lack of awareness of the need for women to have their heart health checked. |
| A long-term commitment to end rheumatic heart disease | Make a long term commitment to end rheumatic heart disease as a major public health issue confronting Aboriginal and Torres Strait Islander people |
| Boost uptake of life-saving cardiac rehabilitation | Boost uptake of life-saving cardiac rehabilitation $1M every two years. Fund a biennial national audit of cardiac rehabilitation to improve uptake of this life-saving service for people who have had a coronary event, especially those living in regional, rural and remote communities. |
| Ensure funding for CVD research reflects the burden the disease imposes on the community | Ensure disbursements for disease specific research form the National Health and Medical Research Council and the Medical Research fund are commensurate with the burden these diseases impose on the community. Support the National Health Measurement Survey via the Medical Research Future Fund. |
Source: Heart Foundation, 2017 [101]
The Heart Foundation of Australia also recommended a health levy on sugary drinks ($400 M per year) and a reform of alcohol tax could raise $3.3 Bn per year and reduce excessive consumption and harm while providing a source of revenue for preventative health and research [101]. In its report Fighting for Australian hearts the Foundation identified priorities were:
- Helping Australian families make heart healthy choices
- Reducing preventable heart attacks by supporting vulnerable communities
- Getting the care you deserve and making the best recovery possible
- Research [205].
Concluding comments
While statistics surrounding CVD have generally improved, there is still much work to be done as CVD is largely preventable. The reasons for disadvantage in cardiovascular health for Aboriginal and Torres Strait Islander people are complex and lie in the impacts of historical colonisation, and subsequent intergenerational trauma, marginalisation, ongoing institutional racism and poverty. Lower socioeconomic status increases high risk behaviours for CVD such as smoking, risky alcohol intake, poor diet and physical inactivity. All of these factors impact Aboriginal and Torres Strait Islander people disproportionately. There are indications that diet for many is getting slightly worse with few people eating sufficient vegetables and the prevalence of overweight and obesity is increasing [35]. There are however, good signs that less young people are taking up smoking.
The complexity of the underlying social disadvantage means there is no ‘easy-fix’ to these problems and any primary prevention strategies implemented and decreases in social/behavioural risk factors, are likely to take considerable time before they are translated into measurable differences in CVD morbidity and mortality. There is urgent need for development and implementation of a funded nation-wide program to tackle CVD in Aboriginal and Torres Strait Islander populations. In the short-term however, management of CVD can be greatly improved for this population, who suffer increased waiting time for medical attention and a lack of rehabilitation services, often related to geographical remoteness. It is encouraging that more Aboriginal and Torres Strait Islander people are going for health checks. The checks are important because although CVD mostly affects people from middle to old age, CVD can occur at younger ages than in the non-Indigenous population so spotting early warning signs is vital.
The Council of Australian Governments places a focus on Closing the gap to achieve equality in health and life expectancy for Aboriginal and Torres Strait Islander people [23, 206]. The specified targets of this scheme to close the health and life expectancy gap between Aboriginal and Torres Strait Islander people and non-Indigenous people in Australia, remain a challenge [207]. CVD is a significant contributor to this gap, affecting proportionally more Aboriginal and Torres Strait Islanders at a younger age and resulting in higher morbidity and mortality. Many of the Close the Gap targets were not on track by 2018 [23] including:
- to halve the gap in child mortality rates by 2018
- to close the gap in life expectancy by 2031.
Four of the seven targets expired in 2018 so the Australian Government has worked with Aboriginal and Torres Strait Islander people to develop the Closing the Gap Refresh [23]. In 2018, COAG released the COAG statement on the Closing the Gap Refresh [208], this is a draft of the strengths-based framework that recognises the importance of genuine partnership between the governments and Aboriginal and Torres Strait Islander people and outlined refreshed targets. The refresh represents a fundamental recalibration of the aspirations of not only the targets but also, and perhaps more significantly, how these targets will be met. The Prime Minister in his Closing the Gap report has signalled a whole of government commitment to some principles that he believes will shift the narrative in profoundly important ways [23]. The principles are not new in the sense that they have been called for by Aboriginal leaders for some time, for example in the Redfern Statement [209] and the Uluru Statement from the Heart [210]. They include a commitment to strengths based approaches, authentic partnerships, co-design, community led solutions, a strong evidenced based approach, whole of government (including states and territories) approaches and clearly articulated accountabilities.
In respect to many of the stated areas of improvement, such as reducing smoking, providing improved access to specialist services in remote areas, achieving greater rates of secondary prevention for RHD and reducing adverse outcomes in coronary care and stroke, are still a considerable distance from their targets.
While incidence of CVD (including stroke and CHD) among Indigenous people has declined over several decades, reflecting a decline in the general population, the ‘gap’ remains due to a combination of higher risk factors, comorbidities (such as diabetes) and persistently poorer access to good quality primary and hospital care. This is especially true of Aboriginal and Torres Strait Islander people in remote and regional areas and a large burden of CVD is attributed to RHD. Access to good quality affordable food, secure and appropriate housing, health services which are more focussed on holistic care (along the Aboriginal Community Controlled Service model) and genuine partnership with communities in policy, planning and service delivery should be the focus of future programs to improve the CVD health of Aboriginal and Torres Strait Islander people.
References
- Australian Institute of Health and Welfare. (2019). Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: fourth national report 2018–19. Canberra: Australian Institute of Health and Welfare.
- Australian Institute of Health and Welfare. (2019). Cardiovascular disease. Retrieved 30 Aug 2019 from https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/cardiovascular-health-compendium/contents/what-is-cardiovascular-disease
- World Health Organization. (2019). ICD-11 for mortality and morbidity statistics: diseases of the circulatory system. from https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f426429380
- World Heart Federation. (2017). Cardiovascular risk factors. Retrieved 30 May 2017 from https://www.world-heart-federation.org/resources/risk-factors/
- Australian Institute of Health and Welfare. (2015). Cardiovascular disease, diabetes and chronic kidney disease – Australian facts: risk factors (AIHW Catalogue no CDK 004, cardiovascular, diabetes and chronic kidney disease series no 4). Canberra: Australian Institute of Health and Welfare.
- Dhar, A. K., & Barton, D. A. (2016). Depression and the link with cardiovascular disease. Frontiers in Psychiatry, 7. Retrieved from: https://doi.org/10.3389/fpsyt.2016.00033
- Rémond, M. G. W., Stewart, S., Carrington, M. J., Marwick, T. H., Kingwell, B. A., Meikle, P., . . . Maguire, G. P. (2017). Better Indigenous Risk stratification for Cardiac Health study (BIRCH) protocol: rationale and design of a cross-sectional and prospective cohort study to identify novel cardiovascular risk indicators in Aboriginal Australian and Torres Strait Islander adults. BMC Cardiovascular Disorders, 17. Retrieved from: https://doi.org/10.1186/s12872-017-0662-7
- Australian Institute of Health and Welfare. (2013). Rheumatic heart disease and acute rheumatic fever in Australia: 1996-2012 (AIHW Catalogue no CVD 60, cardiovascular disease series no 36). Canberra: Australian Institute of Health and Welfare.
- Rheumatic Heart Disease Australia, National Heart Foundation of Australia, & Cardiac Society of Australia and New Zealand. (2012). The Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease: 2nd edition. Darwin: Menzies School of Health Research.
- Australian Institute of Health and Welfare. (2019). Acute rheumatic fever and rheumatic heart disease in Australia. Retrieved 11 October 2019 from https://www.aihw.gov.au/reports/indigenous-australians/acute-rheumatic-fever-rheumatic-heart-disease/contents/summary
- Maguire, G. P., Carapetis, J. R., Walsh, W. F., & Brown, A. D. H. (2012). The future of acute rheumatic fever and rheumatic heart disease in Australia [editorial]. Medical Journal of Australia, 197(3), 133-134.
- Australian Institute of Health and Welfare. (2016). Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011 (Australian Burden of Disease Study series no. 6, Cat no. BOD 7). Canberra: Australian Institute of Health and Welfare.
- Australian Bureau of Statistics. (2019). Causes of Death, Australia, 2018. Canberra: Australian Bureau of Statistics.
- Australian Institute of Health and Welfare. (2019). Improving Indigenous identification in mortality estimates (Cat. no. IHW 215). Canberra: Australian Institute of Health and Welfare.
- Dudgeon, P., Wright, M., Paradies, Y., Garvey, D., & Walker, I. (2014). Aboriginal social, cultural and historical contexts. In P. Dudgeon, H. Milroy & R. Walker (Eds.), Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice (2nd ed., pp. 3-24). Canberra: Department of The Prime Minister and Cabinet.
- Atkinson, J., Nelson, J., Brooks, R., Atkinson, C., & Ryan, K. (2014). Addressing individual and community transgenerational trauma. In P. Dudgeon, H. Milroy & R. Walker (Eds.), Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice (2nd edition ed., pp. 289-306 (chapter 217)). Canberra: Department of The Prime Minister and Cabinet.
- Lee, A., & Ride, K. (2018). Review of nutrition among Aboriginal and Torres Strait Islander people. Australian Indigenous HealthBulletin, 18(1). Retrieved from: http://healthbulletin.org.au/articles/review-of-nutrition-among-aboriginal-and-torres-strait-islander-people/
- Pascoe, B. (2018). Dark emu: Aboriginal Australia and the birth of agriculture. Broome, WA: Magabala Books.
- Australian Institute of Health and Welfare. (2019). Indicators of socioeconomic inequalities in cardiovascular disease, diabetes and chronic kidney disease (Cat. no. CDK 12). Canberra: Australian Institute of Health and Welfare.
- Marmot, M. (2011). Social determinants and the health of Indigenous Australians. Aboriginal and Islander Health Worker Journal, 35(3), 21-22.
- Australian Institute of Health and Welfare. (2018). Australia’s health 2018 (Australia’s health series no. 16, Cat. no: AUS 221). Canberra: Australian Institute of Health and Welfare.
- Reconciliation Australia. (2019). Australian reconciliation barometer 2018. Canberra: Reconciliation Australia.
- Department of the Prime Minister and Cabinet. (2019). Closing the Gap report 2019. Canberra: Department of the Prime Minister and Cabinet.
- Gee, G., Dudgeon, P., Schultz, C., Hart, A., & Kelly, K. (2014). Aboriginal and Torres Strait Islander social and emotional wellbeing. In P. Dudgeon, H. Milroy & R. Walker (Eds.), Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice (2nd ed., pp. 55-68). Canberra: Department of The Prime Minister and Cabinet.
- National Aboriginal Health Strategy Working Party. (1989). A national Aboriginal health strategy. Canberra: Department of Aboriginal Affairs.
- Australian Bureau of Statistics. (2019). Estimates and projections, Aboriginal and Torres Strait Islander Australians, 2006 to 2031. Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2019). Australian demographic statistics, June 2019. from https://www.abs.gov.au/ausstats/abs%40.nsf/mediareleasesbyCatalogue/CA1999BAEAA1A86ACA25765100098A47?OpenDocument
- Australian Bureau of Statistics. (2017). Census of population and housing: reflecting Australia – stories from the Census, 2016: Aboriginal and Torres Strait Islander population. Retrieved 28 June 2017 from https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2071.02016?OpenDocument
- Australian Bureau of Statistics. (2013). Understanding the increase in Aboriginal and Torres Strait Islander counts, 2006-2011 (ABS Cat. no. 2077.0). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2018). Estimates of Aboriginal and Torres Strait Islander Australians, June 2016. Retrieved 31 August 2018 from https://www.abs.gov.au/ausstats/abs@.nsf/mf/3238.0.55.001
- Australian Bureau of Statistics. (2018). Life tables for Aboriginal and Torres Strait Islander Australians, 2015-2017 (ABS Cat. no. 3302.0.55.003). Canberra: Australian Bureau of Statistics.
- Australian Health Ministers’ Advisory Council. (2017). Aboriginal and Torres Strait Islander Health Performance Framework: 2017 report. Canberra: Department of the Prime Minster and Cabinet.
- Australian Institute of Health and Welfare. (2015). Cardiovascular disease, diabetes and chronic kidney disease- Australian facts: Aboriginal and Torres Strait Islander people. Canberra: Australian Institute of Health and Welfare.
- Al-Yaman, F. (2017). The Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people, 2011. Public Health Research & Practice, 27(4). Retrieved from: https://doi.org/10.17061/phrp2741732
- Australian Bureau of Statistics. (2019). National Aboriginal and Torres Strait Islander Health Survey, 2018-19. Canberra: Australian Bureau of Statistics.
- Nichols, M., Peterson, K., Herbert, J., & Allender, S. (2015). Australian heart disease statistics 2015: overweight, obesity and cardiovascular disease- past, present and future. Melbourne: Heart Foundation.
- Australian Institute of Health and Welfare. (2013). Indigenous identification in hospital separations data: quality report (AIHW Catalogue No IHW 90). Canberra: Australian Institute of Health and Welfare.
- Australian Institute of Health and Welfare. (2019). Admitted patient care 2017-18 (AIHW Cat. no: HSE 225). Canberra: Australian Institute of Health and Welfare.
- Australian Institute of Health and Welfare. (2018). Cardiovascular disease snapshot. Retrieved 24 July 2018 from https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/cardiovascular-health-compendium/contents/hospital-care-for-cardiovascular-disease
- Australian Institute of Health and Welfare. (2017). Aboriginal and Torres Strait Islander Health Performance Framework. Retrieved 30 May 2017 from https://www.aihw.gov.au/reports/indigenous-health-welfare/health-performance-framework/contents/overview
- Steering Committee for the Review of Government Service Provision. (2016). Overcoming Indigenous disadvantage: key indicators 2016 report. Canberra: Productivity Commission.
- National Heart Foundation of Australia. (2016). Australian Heart Maps. Retrieved 2016 from http://www.heartfoundation.org.au/for-professionals/australian-heart-maps
- National Heart Foundation. (2018). What is coronary heart disease? Retrieved 2018 from https://www.heartfoundation.org.au/your-heart/heart-conditions/what-is-coronary-heart-disease
- Australian Institute of Health and Welfare. (2014). Trends in coronary heart disease mortality: age groups and populations (AIHW Catalogue no CVD 79). Canberra: Australian Institute of Health and Welfare.
- Bradshaw, P. J., Alfonso, H. S., Finn, J., Owen, J., & Thompson, P. L. (2010). A comparison of coronary heart disease event rates among urban Australian Aboriginal people and a matched non-Aboriginal population. Journal of Epidemiology and Community Health, 65(4), 315-319.
- Australian Bureau of Statistics. (2015). Causes of death, Australia, 2013 (ABS Catalogue no 3303.0). Canberra: Australian Bureau of Statistics.
- Wang, Z., & Hoy, W. E. (2013). Lifetime risk of developing coronary heart disease in Aboriginal Australians: a cohort study. BMJ Open, 3. Retrieved from: http://dx.doi.org/10.1136/bmjopen-2012-002308
- American Association of Neurological Surgeons. (2018). Cerebrovascular disease. Retrieved 2019 from https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Cerebrovascular-Disease
- Foreman, J., Keel, S., Xie, J., van Wijngaarden, P., Crowston, J., Taylor, H. R., & Dirani, M. (2016). The National Eye Health Survey 2016 report. Melbourne: Vision 2020 Australia.
- Keel, S., Foreman, J., Xie, J., Taylor, H. R., & Dirani, M. (2017). The prevalence of self-reported stroke in the Australian National Eye Health Survey. Journal of Stroke and Cerebrovascular Diseases, 26(7), 1433-1439.
- Katzenellenbogen, J. M., Knuiman, M. W., Sanfilippo, F. M., Hobbs, M. S., & Thompson, S. C. (2014). Prevalence of stroke and coexistent conditions: disparities between Indigenous and nonIndigenous Western Australians. International Journal of Stroke, 9(Supplement A100), 61-68.
- Balabanski, A. H., Newbury, J., Leyden, J. M., Arima, H., Anderson, C. S., Castle, S., . . . Kleinig, T. J. (2018). Excess stroke incidence in young Aboriginal people in South Australia: pooled results from two population-based studies. International Journal of Stroke, 13(8), 811-814.
- Australian Institute of Health and Welfare. (2013). Stroke and its management in Australia: an update (AIHW Catalogue no CVD 61, cardiovascular disease series no 37). Canberra: Australian Institute of Health and Welfare.
- Zhao, Y., Guthridge, S., Falhammar, H., Flavell, H., & Cadilhac, D. A. (2017). Cost-effectiveness of stroke care in Aboriginal and non-Aboriginal patients: an observational cohort study in the Northern Territory of Australia. BMJ Open, 7(10). Retrieved from: https://doi.org/10.1136/bmjopen-2016-015033
- National Heart Foundation of Australia. (2016). Guideline for the diagnosis and management of hypertension in adults. Canberra: National Heart Foundation of Australia.
- Australian Institute of Health and Welfare. (2019). National key performance indicators for Aboriginal and Torres Strait Islander primary health care: results to June 2018. Retrieved 8 July 2019 from https://www.aihw.gov.au/reports/indigenous-australians/nkpis-indigenous-australians-health-care-2018/contents/indigenous-primary-health-care-organisations
- Esler, D., Raulli, A., Pratt, R., & Fagan, P. (2016). Hypertension: high prevalence and a positive association with obesity among Aboriginal and Torres Strait Islander youth in far north Queensland. Australian and New Zealand Journal of Public Health, 40(S1), S65-S69.
- Larkins, N., Teixeira-Pinto, A., Banks, E., Gunasekera, H., Cass, A., Kearnes, J., & Craig, J. C. (2017). Blood pressure among Australian Aboriginal children. Journal of Hypertension, 35(9), 1801-1807.
- Rao, G. (2016). Diagnosis, epidemiology, and management of hypertension in children. Pediatrics, 138(2). Retrieved from: https://doi.org/10.1542/peds.2015-3616
- Parnaby, M. G., & Carapetis, J. R. (2010). Rheumatic fever in Indigenous Australian children. Journal of Paediatrics and Child Health, 46(9), 527-533.
- Australian Institute of Health and Welfare. (2019). Acute rheumatic fever and rheumatic heart disease in Australia: in brief. Canberra: Australian Institute of Health and Welfare.
- Rheumatic Heart Disease Australia. (2019). What is rheumatic heart disease? from https://www.rhdaustralia.org.au/what-rheumatic-heart-disease
- Australian Institute of Health and Welfare. (2018). Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: third national report 2017. Canberra: Australian Institute of Health and Welfare.
- Chronic Care for Aboriginal People. (2017). Acute rheumatic fever and rheumatic heart disease in NSW: framework. Sydney: Agency for Clinical Innovation.
- Roberts, K., Maguire, G., Brown, A., Atkinson, D., Reményi, B., Wheaton, G., . . . Carapetis, J. R. (2014). Echocardiographic screening for rheumatic heart disease in high and low risk Australian children. Circulation, 129(19), 1953-1961.
- Wyber, R., Katzenellenbogen, J. M., Pearson, G., & Gannon, M. (2017). The rationale for action to end new cases of rheumatic heart disease in Australia. Medical Journal of Australia, 207(8), 322-323.
- Lawrence, J. G., Carapetis, J. R., Griffiths, K., Edwards, K., & Condon, J. R. (2013). Acute rheumatic fever and rheumatic heart disease: incidence and progression in the Northern Territory of Australia 1997-2010. Circulation, 128(5), 492-501.
- He, V. Y., Condon, J. R., Ralph, A. P., Zhao, Y., Roberts, K., de Dassel, J. L., . . . Carapetis, J. R. (2016). Long term outcomes from acute rheumatic fever and rheumatic heart disease: a data-linkage and survival analysis approach. Circulation, 134(3), 222-232.
- Australian Institute of Health and Welfare. (2019). Congenital heart disease in Australia (Cat. no. CDK 14). Canberra: Australian Institute of Health and Welfare.
- Nembhard, W. N., Bourke, J., Leonard, H., Eckersley, L., Li, J., & Bower, C. (2016). Twenty-five-year survival for Aboriginal and caucasian children with congenital heart defects in Western Australia, 1980 to 2010. Birth Defects Research Part A: Clinical and Molecular Teratology, 106(12), 1016-1031.
- Penm, E. (2008). Cardiovascular disease and its associated risk factors in Aboriginal and Torres Strait Islander peoples 2004-05 (Cardiovascular disease series no. 29. Cat. no. CVD 41). Canberra: Australian Institute of Health and Welfare.
- Australian Institute of Health and Welfare. (2011). Cardiovascular disease: Australian facts 2011 (AIHW Catalogue no. CVD 53, cardiovascular disease series no. 35). Canberra: Australian Institute of Health and Welfare.
- Calabria, B., Korda, R. J., Lovett, R. W., Fernando, P., Martin, T., Malamoo, L., . . . Banks, E. (2018). Absolute cardiovascular disease risk and lipid-lowering therapy among Aboriginal and Torres Strait Islander Australians. Medical Journal of Australia, 209(1), 35-41.
- Wiemers, P. D., Fraser, J. F., Marney, L., Yadav, S., & Tam, R. (2019). A review of coronary artery bypass grafting in the Indigenous Australian population. Heart, Lung and Circulation, 28(4), 530-538.
- Durey, A. (2010). Reducing racism in Aboriginal health care in Australia: where does cultural education fit? Australian and New Zealand Journal of Public Health, 34(S1), S87-S92.
- Durey, A., & Thompson, S. C. (2012). Reducing the health disparities of Indigenous Australians: time to change focus. BMC Health Services Research, 12. Retrieved from: https://doi.org/10.1186/1472-6963-12-151
- Thompson, S. C., Haynes, E., Woods, J. A., Bessarab, D. C., Dimer, L. A., Wood, M. M., . . . Katzenellenbogen, J. M. (2016). Improving cardiovascular outcomes among Aboriginal Australians: lessons from research for primary care. SAGE Open Medicine, 4. Retrieved from: https://doi.org/10.1177/2050312116681224
- Shepherd, F., Battye, K., & Chalmers, E. (2003). Improving access to cardiac rehabilitation for remote Indigenous clients. Australian and New Zealand Journal of Public Health, 27(6), 632-636.
- Mincham, C. M., Toussaint, S., Mak, D. B., & Plant, A. J. (2003). Patient views on the management of rheumatic fever and rheumatic heart disease in the Kimberley: a qualitative study. Australian Journal of Rural Health, 11(6), 260-265.
- Ilton, M. K., ,, Walsh, W. F., Brown, A. D. H., Tideman, P. A., Zeitz, C. J., & Wilson, J. (2014). A framework for overcoming disparities in management of acute coronary syndromes in the Australian Aboriginal and Torres Strait Islander population: a consensus statement from the National Heart Foundation of Australia. Medical Journal of Australia, 200(11), 639-643.
- Stanford, J., Charlton, K., McMahon, A. T., & Winch, S. (2019). Better cardiac care: health professional’s perspectives of the barriers and enablers of health communication and education with patients of Aboriginal and Torres Strait Islander descent. BMC Health Services Research, 19. Retrieved from: https://doi.org/10.1186/s12913-019-3917-4
- Reath, J., & Brown, N. (2010). Managing cardiovascular disease in Aboriginal and Torres Strait Islander people. Australian Prescriber, 33(3), 72-75.
- Australian Institute of Health and Welfare. (2019). Indigenous health checks and follow-ups [web report]. Retrieved 24 June 2019 from https://www.aihw.gov.au/reports/indigenous-health-welfare-services/indigenous-health-checks-follow-ups/contents/overview
- Wang, Z., & Hoy, W. E. (2005). Is the Framingham coronary heart disease absolute risk function applicable to Aboriginal people? Medical Journal of Australia, 182(2), 66-69.
- Central Australian Rural Practitioners Association. (2017). CARPA standard treatment manual: a clinic manual for primary health care practitioners in remote and Indigenous health services in central and northern Australia (7th ed.). Alice Springs: Centre for Remote Health.
- Hua, X., McDermott, R., Lung, T., Wenitong, M., Tran-Duy, A., Li, M., & Clarke, P. (2017). Validation and recalibration of the Framingham cardiovascular disease risk models in an Australian Indigenous cohort. European Journal of Preventive Cardiology, 24(15), 1660-1669.
- Tray-Duy, A., McDermott, R., Knight, J., Hua, X., Barr, E. L. M., Arabena, K., . . . Clarke, P. M. (2019). Development and use of prediction models for classification of cardiovascular risk of remote Indigenous Australians. Heart, Lung and Circulation, 28(4), 530-538.
- Wang, Z., Hoy, W. E., & Wang, Z. (2013). The correlates of urinary albumin to creatinine ratio (ACR) in a high risk Australian Aboriginal community. BMC Nephrology, 14. Retrieved from: http://dx.doi.org/10.1186/1471-2369-14-176
- Gray, C., Brown, A., & Thomson, N. (2012). Review of cardiovascular health among Indigenous Australians (Australian Indigenous HealthReviews no. 9). Perth: Australian Indigenous HealthInfoNet.
- Hamilton, S., Mills, B., McRae, S., & Thompson, S. (2016). Cardiac rehabilitation for Aboriginal and Torres Strait Islander people in Western Australia. BMC Cardiovascular Disorders, 16. Retrieved from: http://dx.doi.org/10.1186/s12872-016-0330-3
- Heart Foundation. (2016). Priority 6: improve participation in cardiac rehabilitation and ongoing care (pp. 3). Melbourne: Heart Foundation.
- National Health and Medical Research Council. (2005). Strengthening cardiac rehabilitation and secondary prevention for Aboriginal and Torres Strait Islander peoples: a guide for health professionals. Canberra: National Health and Medical Research Council.
- Clark, R. A., Conway, A., Poulsen, V., Keech, W., Tirimacco, R., & Tideman, P. (2015). Alternative models of cardiac rehabilitation: a systematic review. European Journal of Preventative Cardiology, 22(1), 35-74.
- Field, P. E., Franklin, R. C., Barker, R. N., Ring, I., & Leggat, P. A. (2018). Cardiac rehabilitation services for people in rural and remote areas: an integrative literature review. Rural and Remote Health, 18(4). Retrieved from: https://doi.org/10.22605/RRH4738
- Lopez, D., Katzenellenbogen, J. M., Sanfilippo, F. M., Woods, J. A., Hobbs, M. S., Knuiman, M. W., . . . Thompson, S. C. (2014). Disparities experienced by Aboriginal compared to non-Aboriginal metropolitan Western Australians in receiving coronary angiography following acute ischaemic heart disease: the impact of age and comorbidities. International Journal for Equity in Health, 13. Retrieved from: https://doi.org/10.1186/s12939-014-0093-3
- Bradshaw, P. J., Alfonso, H. S., Finn, J., Owen, J., & Thompson, P. L. (2010). The use of coronary revascularisation procedures in urban Australian Aboriginals and a matched general population: coronary procedures in Aboriginals. Heart, Lung and Circulation, 19(4), 247-250.
- Roe, Y. L., Esterman, A., McDermott, R., & Zeitz, C. (2016). The management of Indigenous patients presenting with non ST-segment elevation acute coronary syndrome in South Australia: a retrospective cohort study. Internal Medicine Journal, 46(2), 202-213.
- Tavella, R., McBride, K., Keech, W., Kelly, J., Rischbieth, A., Zeitz, C., . . . Brown, A. (2016). Disparities in acute in-hospital cardiovascular care for Aboriginal and non-Aboriginal South Australians. Medical Journal of Australia, 205(5), 222-227.
- Artuso, S., Cargo, M., Brown, A., & Daniel, M. (2013). Factors influencing health care utilisation among Aboriginal cardiac patients in central Australia: a qualitative study. BMC Health Services Research, 13. Retrieved from: https://doi.org/10.1186/1472-6963-13-83
- Nour, D., Kang, S., Vangaveti, V., & Saxena, P. (2019). A retrospective analysis investigating the incidence of major cardiac adverse events (MACE) in Indigenous patients who received percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) surgery [conference abstract]. Heart, Lung and Circulation, 28(Supplement 4), S353-S354.
- The Heart Foundation. (2017). Beating hearts: cardiovascular policy proposals to save lives and money. Melbourne: The Heart Foundation.
- Stroke Foundation. (2017). National stroke audit acute services 2017. Victoria: Stroke Foundation.
- Kilkenny, M. F., Harris, D. M., Ritchie, E. A., Price, C., & Cadilhac, D. A. (2013). Hospital management and outcomes of stroke in Indigenous Australians: evidence from the 2009 Acute Care National Stroke Audit. International Journal of Stroke, 8(3), 164-171.
- Blacker, D., & Armstrong, E. (2019). Indigenous stroke care: differences, challenges and a need for change. Internal Medicine Journal, 49(8), 945-947.
- Stroke Foundation. (2017). Clinical guidelines for stroke management 2017: Aboriginal and Torres Strait Islander people. Melbourne: Stroke Foundation.
- Tiederman, C., Suthers, B., Julien, B., Hackett, A., & Oakley, P. (2019). Management of stroke in the Australian Indigenous population: from hospitals to communities. Internal Medicine Journal, 49(8), 962-968.
- Quigley, R., Mann, J., Robertson, J., & Bonython-Ericson, S. (2019). Are we there yet? Exploring the journey to quality stroke care for Aboriginal and Torres Strait Islander peoples in rural and remote Queensland. Rural and Remote Health, 19. Retrieved from: https://doi.org/10.22605/RRH4850
- Armstrong, B., & Coffin, J. (2019). Aboriginal Australians want care after brain injury. But it must consider their cultural needs. Retrieved 23 May 2019 from https://theconversation.com/aboriginal-australians-want-care-after-brain-injury-but-it-must-consider-their-cultural-needs-115128
- Brown, A., Keech, W., McBride, K., Kelly, J., Stewart, S., & Dowling, A. (2016). South Australian Aboriginal heart and stroke plan 2017-2021. Adelaide: South Australian Health and Medical Research Institute.
- Ralph, A. P., Read, C., Johnston, V., de Dassel, J. L., Bycroft, K., Mitchell, A., . . . Carapetis, J. R. (2016). Improving delivery of secondary prophylaxis for rheumatic heart disease in remote Indigenous communities: study protocol for a stepped-wedge randomised trial. Trials, 17. Retrieved from: http://dx.doi.org/10.1186/s13063-016-1166-y
- Steer, A. C., & Carapetis, J. R. (2009). Acute rheumatic fever and rheumatic heart disease in Indigenous populations. Pediatric Clinics of North America, 56(6), 1401-1419.
- Armstrong, C. (2010). AHA guidelines on prevention of rheumatic fever and diagnosis and treatment of acute streptococcal pharyngitis. American Family Physician, 81(3), 346-359.
- Parks, T., Smeesters, P. R., & Steer, A. C. (2012). Streptococcal skin infection and rheumatic heart disease. Current Opinion in Infectious Diseases, 25(2), 145-153.
- Ralph, A. P., Noonan, S., Boardman, C., Halkon, C., & Currie, B. J. (2017). Prescribing for people with acute rheumatic fever. Australian Prescriber, 40, 70-75.
- Dale, J. B., Batzloff, M. R., Cleary, P., Courtney, H. S., Good, M. F., Grandi, G., . . . Steer, A. C. (2016). Current approaches to Group A Streptococcal vaccine development. In J. J. Ferretti, D. L. Stevens & V. A. Fischetti (Eds.), Streptococcus pyogenes: basic biology to clinical manifestations. Oklahoma City: University of Oklahoma Health Sciences Center.
- Sekuloski, S., Batzloff, M. R., Griffin, P., Parsonage, W., Elliott, S., Hartas, J., . . . Good, M. F. (2018). Evaluation of safety and immunogenicity of a group A streptococcus vaccine candidate (MJ8VAX) in a randomized clinical trial. PLOS ONE, 13(7). Retrieved from: https://doi.org/10.1371/journal.pone.0198658
- Wyatt, K. (2019). $35 Million for vaccine to end rheumatic heart disease [media release]. Retrieved 24 February 2019 from http://webarchive.nla.gov.au/gov/20190510024616/http://www.health.gov.au/internet/ministers/publishing.nsf/Content/B6E37D317FAA4CF8CA2583AB007E8A7A/$File/KW031.pdf
- RHDAustralia. (2019). Rheumatic heart disease control programs. Retrieved 2019 from https://www.rhdaustralia.org.au/programs
- Rémond, M. G. W., Severin, K. L., Hodder, Y., Martin, J., Nelson, C., Atkinson, D., & Maguire, G. P. (2013). Variability in disease burden and management of rheumatic fever and rheumatic heart disease in two regions of tropical Australia. Internal Medicine Journal, 43(4), 386-393.
- Cannon, J., Roberts, K., Milne, C., & Carapetis, J. R. (2017). Rheumatic heart disease severity, progression and outcomes: a multi-state model. Journal of the American Heart Association, 6(3). Retrieved from: https://doi.org/10.1161/JAHA.116.003498
- Ralph, A. P., de Dassel, J. L., Kirby, A., Read, C., Mitchell, A. G., Maguire, G. P., . . . Carapetis, J. R. (2018). Improving delivery of secondary prophylaxis for rheumatic heart disease in a high‐burden setting: outcome of a stepped‐wedge, community, randomized trial. Journal of the American Heart Association, 7(14). Retrieved from: https://doi.org/10.1161/JAHA.118.009308
- Katzenellenbogen, J., Bond-Smith, D., Ralph, A., Wilmot, M., Marsh, J., Bailie, R., & Matthews, V. (2019). Priorities for improvement in management of Acute Rheumatic Fever and Rheumatic Heart Disease: analysis of cross-sectional continuous quality improvement data in Aboriginal primary health care centres in Australia. Australian Health Review, Accepted article(https://doi.org/10.1071/AH19132).
- Rheumatic Heart Disease Australia. (2017). What does a culturally competent model of self-management look like? Retrieved 13 November 2017 from https://www.rhdaustralia.org.au/news/arf-rhd-self-management-resource
- Haynes, E., Marawili, M., Marika, B. M., Mitchell, A. G., Phillips, J., Bessarab, D., . . . Ralph, A. P. (2019). Community-based participatory action research on rheumatic heart disease in an Australian Aboriginal homeland: evaluation of the ‘On track watch’ project. Evaluation and Program Planning, 74, 38-53.
- Kelly, J. (2017). World Health Organization makes rheumatic heart disease a global health priority. Retrieved 22 June 2017 from https://www.heartfoundation.org.au/news/world-health-organization-makes-rheumatic-heart-disease-a-global-health-priority
- Katzenellenbogen, J. M., Bond-Smith, D., Seth, R. J., Dempsey, K., Cannon, J., Nedkoff, L., . . . Bessarab, D. (2019). The End Rheumatic Heart Disease in Australia Study of Epidemiology (ERASE) Project: data sources, case ascertainment and cohort profile. Clinical Epidemiology, 2019(11), 997-1010.
- Health Policy Analysis. (2017). Evaluation of the rheumatic fever strategy: final report. Canberra: Australian Department of Health.
- National Heart Foundation of Australia. (2013). Coronary heart disease (pp. 2). Canberra: National Heart Foundation of Australia.
- Ambrose, J. A., & Barua, R. S. (2004). The pathophysiology of cigarette smoking and cardiovascular disease: an update. Journal of the American College of Cardiology, 43(10), 1731-1737.
- Scollo, M. M., & Winstanley, M. H. (2019). Tobacco in Australia: facts and issues. Retrieved July 2019 from https://www.tobaccoinaustralia.org.au/
- Banks, E., Joshy, G., Korda, R. J., Stavreski, B., Soga, K., Egger, S., . . . Lopez, A. D. (2019). Tobacco smoking and risk of 36 cardiovascular disease subtypes: fatal and non-fatal outcomes in a large prospective Australian study. BMC Medicine, 17. Retrieved from: https://doi.org/10.1186/s12916-019-1351-4
- Cancer Australia. (2019). Smoking prevalence- adults. Retrieved 28 June 2019 from https://ncci.canceraustralia.gov.au/prevention/smoking-prevelance/smoking-prevalence-adults
- Lovett, R., Thurber, K. A., & Maddox, R. (2017). The Aboriginal and Torres Strait Islander smoking epidemic: what stage are we at, and what does it mean? Public Health Research & Practice, 27(4). Retrieved from: https://doi.org/10.17061/phrp2741733
- Australian Bureau of Statistics. (2017). Aboriginal and Torres Strait Islander peoples: smoking trends, Australia, 1994 to 2014-15. Retrieved 19 October 2017 from https://www.abs.gov.au/ausstats/abs@.nsf/mf/4737.0?OpenDocument
- Australian Bureau of Statistics. (2016). National Aboriginal and Torres Strait Islander Social Survey, 2014-15. Canberra: Australian Bureau of Statistics.
- Australian Institute of Health and Welfare. (2019). Australia’s mothers and babies 2017 – in brief (Perinatal statistics series no. 35. Cat. no. PER 100). Canberra: Australian Institute of Health and Welfare.
- Nicholson, A., Borland, R., Bennet, P., Davey, M., Sarin, J., Van der Sterren, A., . . . Thomas, D. (2017). The effect of pack warning labels on quitting and related thoughts and behaviours in a national cohort of Aboriginal and Torres Strait Islander smokers. Nicotine & Tobacco Research, 19(10), 1163-1171.
- Nicholson, A. K., Borland, R., Couzos, S., Stevens, M., & Thomas, D. P. (2015). Smoking-related knowledge and health risk beliefs in a national sample of Aboriginal and Torres Strait Islander people. Medical Journal of Australia, 202(10 Suppl), S45-S50.
- van der Sterren, A., Greenhalgh, E. M., Knoche, D., Winstanley, M. H., Scollo, M. M., & Winstanley, M. H. (2019). Prevalence of tobacco use among Aboriginal peoples and Torres Strait Islanders Tobacco in Australia: facts and issues (4 ed.). Melbourne: The Cancer Council.
- Australian Bureau of Statistics. (2007). Tobacco smoking – Aboriginal and Torres Strait Islander people: a snapshot, 2004-05. from http://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/4722.0.55.004Main%20Features12004-05?opendocument&tabname=Summary&prodno=4722.0.55.004&issue=2004-05&num=&view=
- Australian Institute of Health and Welfare. (2019). Australian Burden of Disease Study 2015: interactive data on risk factor burden. from https://www.aihw.gov.au/reports/burden-of-disease/interactive-data-risk-factor-burden/contents/tobacco-use
- Intergovernmental Committee on Drugs. (2012). National tobacco strategy 2012-2018. Canberra: National Drug Strategy.
- Better Health Channel. (2013). Aboriginal health – barriers to physical activity (pp. 3). Melbourne: Better Health Channel.
- Australian Government Department of Health. (2019). Australia’s physical activity and sedentary behaviour guidelines and the Australian 24-hour movement guidelines. Canberra: Australian Government Department of Health.
- Australian Government Department of Health. (2014). Australia’s physical activity and sedentary behaviour guidelines- guidelines evidence summary. Canberra: Australian Government Department of Health.
- National Heart Foundation of Australia. (2013). Physical activity (pp. 2). Canberra: National Heart Foundation of Australia.
- Katzmarzyk, P. T., Church, T. S., Craig, C. L., & Bouchard, C. (2009). Sitting time and mortality from all causes, cardiovascular disease, and cancer. Medicine and Science in Sports and Exercise, 41(5), 998-1005.
- Australian Bureau of Statistics. (2014). Australian Aboriginal and Torres Strait Islander health survey: physical activity, 2012–13 (ABS cat. no. 4727.0.55.004). Canberra: Australian Bureau of Statistics.
- Macniven, R., Richards, J., Gubhaju, L., Joshy, G., Bauman, A., Banks, E., & Eades, S. (2016). Physical activity, healthy lifestyle behaviors, neighborhood environment characteristics and social support among Australian Aboriginal and non-Aboriginal adults. Preventive Medicine Reports, 3, 203–210.
- Bruner, M. W., Hillier, S., Baillie, C. P. T., Lavallee, L. F., Bruner, B. G., Hare, K., . . . Lévesque, L. (2015). Positive youth development in Aboriginal physical activity and sport: a systematic review. Adolescent Research Review, 1(3), 257–269.
- Canuto, K. J., Spagnoletti, B., McDermott, R. A., & Cargo, M. (2013). Factors influencing attendance in a structured physical activity program for Aboriginal and Torres Strait Islander women in an urban setting: a mixed methods process evaluation. International Journal for Equity in Health, 12. Retrieved from: https://doi.org/10.1186/1475-9276-12-11
- Ferguson, M., Brown, C., Georga, C., Miles, E., Wilson, A., & Brimblecombe, J. (2017). Traditional food availability and consumption in remote Aboriginal communities in the Northern Territory, Australia. Australian and New Zealand Journal of Public Health, 41(3), 294-298.
- National Health and Medical Research Council. (2000). Nutrition in Aboriginal and Torres Strait Islander peoples: an information paper. Canberra: National Health and Medical Research Council.
- National Health and Medical Research Council. (2013). Australian Dietary Guidelines: providing the scientific evidence for healthier Australian diets. Canberra: National Health and Medical Research Council.
- Australian Institute of Health and Welfare. (2018). Nutrition across the life stages. Canberra: Australian Institute of Health and Welfare.
- Bowen, K. J., Sullivan, V. K., Kris-Etherton, P. M., & Petersen, K. S. (2018). Nutrition and cardiovascular disease- an update. Current Atherosclerosis Reports, 20(2). Retrieved from: https://doi.org/10.1007/s11883-018-0704-3
- Australian Bureau of Statistics (ABS). (2016). Australian Aboriginal and Torres Strait Islander Health Survey: consumption of added sugars, 2012-13 (4727.0.55.009). Canberra: Australian Bureau of Statistics (ABS).
- Esselstyn, C. B. (2017). A plant-based diet and coronary artery disease: a mandate for effective therapy. Journal of Geriatric Cardiology, 14(5), 317–320.
- Eilat-Adar, S., Sinai, T., Yosefy, C., & Henkin, Y. (2013). Nutritional recommendations for cardiovascular disease prevention. Nutrients, 5(9), 3646-3683.
- Merone, L., & McDermott, R. (2017). Nutritional anti-inflammatories in the treatment and prevention of type 2 diabetes mellitus and the metabolic syndrome. Diabetes Research and Clinical Practice, 127, 238-253.
- Davy, D. (2016). Australia’s efforts to improve food security for Aboriginal and Torres Strait Islander peoples. Health and Human Rights, 18(2), 209-218.
- Australian Bureau of Statistics. (2015). Australian Aboriginal and Torres Strait Islander health survey: nutrition results – food and nutrients, 2012-13 (ABS cat. no. 4727.0.55.005). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2016). Australian Aboriginal and Torres Strait Islander Health Survey: consumption of food groups from the Australian Dietary Guidelines, 2012-13 (ABS report no. 4727.0.55.008). Canberra: Australian Bureau of Statistics.
- Australian Bureau of Statistics. (2015). Australian Aboriginal and Torres Strait Islander health survey: nutrition results – food and nutrients, 2012-13: Table 4 [data cube]. Retrieved 20 March 2015 from http://www.abs.gov.au/ausstats/subscriber.nsf/log?openagent&4727055005_201213_04.xls&4727.0.55.005&Data%20Cubes&F3E8C224BFBA2FE0CA257E0D000EC970&0&2012-13&20.03.2015&Latest
- World Health Organization. (2015). Guideline: sugars intake for adults and children. Geneva, Switzerland: World Health Organization.
- Australian Bureau of Statistics. (2015). Australian Aboriginal and Torres Strait Islander health survey: nutrition results – food and nutrients, 2012-13: Table 14.1 [data cube]. Retrieved 20 March 2015 from https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4727.0.55.0052012-13?OpenDocument
- McCarthy, L., Chang, A. B., & Brimblecombe, J. (2018). Food security experiences of Aboriginal and Torres Strait Islander families with young children in an urban setting: influencing factors and coping strategies. International Journal of Environmental Research and Public Health, 15(12). Retrieved from: https://doi.org/10.3390/ijerph15122649
- Brown, C., Laws, C., Leonard, D., Campbell, S., Merone, L., Hammond, M., . . . Brimblecombe, J. (2019). Healthy Choice Rewards: a feasibility trial of incentives to influence consumer food choices in a remote Australian Aboriginal community. International Journal of Environmental Research and Public Health, 16. Retrieved from: https://doi.org/10.3390/ijerph16010112
- Australian Institute of Health and Welfare. (2004). The relationship between overweight, obesity and cardiovascular disease: a literature review prepared for the National Heart Foundation of Australia. Canberra: Australian Institute of Health and Welfare.
- Poirier, P., Giles, T. D., Bray, G. A., Hong, Y., Stern, J. S., Pi-Sunyer, F. X., & Eckel, R. H. (2006). Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Circulation, 113(6), 898-918.
- Australian Bureau of Statistics. (2008). Overweight and obesity in adults, Australia, 2004-05 (4719.0). Canberra: Australian Bureau of Statistics.
- Dawson, J., Morland, R., & Brooks, R. (2017). A picture of overweight and obesity in Australia: 2017. Canberra: Australian Institute of Health and Welfare.
- Dunford, M., & Prescott, V. (2017). Impact of physical inactivity as a risk factor for chronic conditions: Australian Burden of Disease Study. Canberra: Australian Institute of Health and Welfare.
- National Health and Medical Research Council. (2013). Eat for Health: Australian dietary guidelines summary. Canberra: National Health and Medical Research Council.
- World Health Organization. (2011). Waist circumference and waist–hip ratio: report of a WHO expert consultation Geneva.
- Li, M., & McDermott, R. (2015). Obesity, albuminuria, and gamma-glutamyl transferase predict incidence of hypertension in Indigenous Australians in rural and remote communities in northern Australia. Journal of Hypertension, 33(4), 704-710.
- Adegbija, O., Hoy, W. E., & Wang, Z. (2015). Corresponding waist circumference and body mass index values based on 10-year absolute type 2 diabetes risk in an Australian Aboriginal community. BMJ Open Diabetes Research & Care, 3(1). Retrieved from: https://doi.org/10.1136/bmjdrc-2015-000127
- Daniel, M., Rowley, K., McDermott, R., & O’Dea, K. (2002). Diabetes and impaired glucose tolerance in Aboriginal Australians: prevalence and risk. Diabetes Research and Clinical Practice, 57(1), 23-33.
- Li, M., & McDermott, R. A. (2010). Using anthropometric indices to predict cardio-metabolic risk factors in Australian Indigenous populations. Diabetes Research and Clinical Practice, 87(3), 401-406.
- Gracey, M., Burke, V., Martin, D. D., Johnston, R. J., Jones, T., & Davis, E. A. (2007). Assessment of risks of “lifestyle” diseases including cardiovascular disease and type 2 diabetes by anthropometry in remote Australian Aborigines. Asia Pacific Journal of Clinical Nutrition, 16(4), 688-697.
- Evans, R., Liu, J., Miller, D., Harvey, M., Howle, T., & Seebus, I. (2018). National Key Performance Indicators for Aboriginal and Torres Strait Islander primary health care: results for 2017. Canberra: Australian Institute of Health and Welfare.
- Gray, D., Cartwright, K., Stearne, A., Saggers, S., Wilkes, E., & Wilson, M. (2018). Review of the harmful use of alcohol among Aboriginal and Torres Strait Islander people. Australian Indigenous HealthBulletin, 18(1), 42.
- Zhang, Y., & Ren, J. (2018). MicroRNA‐21: bridging binge drinking and cardiovascular health. Alcoholism: Clinical and Experimental Research, 42(4), 678-681.
- Nadew, G. T. (2012). Exposure to traumatic events, prevalence of posttraumatic stress disorder and alcohol abuse in Aboriginal communities. Rural and Remote Health, 12. Retrieved from: https://www.rrh.org.au/journal/article/1667
- Intergovernmental Committee on Drugs. (2015). National Aboriginal and Torres Strait Islander peoples’ drug strategy 2014-2019. Canberra: National Drug Strategy.
- Gray, D., & Wilkes, E. (2010). Reducing alcohol and other drug related harm (Resource sheet no. 3). Canberra: Closing the Gap Clearinghouse.
- Emberson, J. R., & Bennett, D. A. (2006). Effect of alcohol on risk of coronary heart disease and stroke: causality, bias, or a bit of both? Vascular Health Risk Management, 2(3), 239-249.
- Heart Foundation. (2019). Drinking alcohol. Retrieved 2019 from https://www.heartfoundation.org.au/healthy-eating/food-and-nutrition/drinks/drinking-alcohol
- National Health and Medical Research Council. (2009). Australian guidelines to reduce health risks from drinking alcohol. Canberra: National Health and Medical Research Council.
- Australian National Health and Medical Research Council. (2019). Draft Australian guidelines to reduce health risks from drinking alcohol. Canberra: Australian National Health and Medical Research Council.
- Australian Institute of Health and Welfare. (2017). National Drug Strategy Household Survey 2016: detailed findings. Canberra: Australian Institute of Health and Welfare.
- Garvey, D. (2008). Review of the social and emotional wellbeing of Indigenous Australian peoples- considerations, challenges and opportunities. Australian Indigenous HealthBulletin, 8(4), 1-29.
- Priest, N. C., Paradies, Y. C., Gunthorpe, W., Cairney, S. J., & Sayers, S. M. (2011). Racism as a determinant of social and emotional wellbeing for Aboriginal Australian youth. Medical Journal of Australia, 194(10), 546-550.
- Vlachakis, C., Dragoumani, K., Raftopoulou, S., Mantaiou, M., Papageorgiou, L., Champeris Tsaniras, S., . . . Vlachakis, D. (2018). Human emotions on the onset of cardiovascular and small vessel related diseases. In Vivo, 32(4), 859-870.
- Chaddha, A., Robinson, E. A., Kline-Rogers, E., Alexandris-Souphis, T., & Rubenfire, M. (2016). Mental health and cardiovascular disease. The American Journal of Medicine, 129(11), 1145-1148.
- Sin, N. L. (2016). The protective role of positive well-being in cardiovascular disease: review of current evidence, mechanisms, and clinical implications. Current Cardiology Reports, 18(11). Retrieved from: https://doi.org/10.1007/s11886-016-0792-z
- Compare, A., Zarbo, C., Manzoni, G. M., Castelnuovo, G., Baldassari, E., Bonardi, A., . . . Romagnoni, C. (2013). Social support, depression, and heart disease: a ten year literature review. Frontiers in Psychology, 4. Retrieved from: https://doi.org/10.3389/fpsyg.2013.00384
- Australian Government Department of Health. (2013). Health plan at a glance. In A. G. D. o. Health (Ed.), National Aboriginal and Torres Strait Islander health plan 2013-2023. Canberra: Australian Government Department of Health.
- Australian Health Ministers’ Advisory Council. (2017). National Strategic Framework for Chronic Conditions. Canberra: Australian Government.
- Chronic Disease Prevention Directorate. (2012). Western Australian health promotion strategic framework 2012–2016. Perth: Western Australia Department of Health.
- Queensland Health. (2015). Queensland Aboriginal and Torres Strait Islander cardiac health strategy 2014-2017. Brisbane: Queensland Health.
- Northern Territory Department of Health. (2012). Cardiac rehabilitation and secondary prevention: a framework for the Northern Territory. Darwin: Northern Territory Department of Health.
- New South Wales Health. (2016). Better cardiac care for Aboriginal and Torres Strait Islander people. Sydney: New South Wales Health.
- Victoria Department of Health and Human Services. (2015). Heart health: improved services and better outcomes for Victorians. Melbourne: Victoria Department of Health and Human Services.
- National Heart Foundation of Australia. (2019). Fighting for Australian hearts. National Heart Foundation of Australia.
- Department of the Prime Minister and Cabinet. (2016). Closing the Gap 2016- Australian government programmes and initiatives. Canberra: Department of the Prime Minister and Cabinet.
- Australian Human Rights Commission. (2018). Close the Gap calls for urgent joint action to address national shame. from https://www.humanrights.gov.au/about/news/close-gap-calls-urgent-joint-action-address-national-shame
- Council of Australian Governments. (2018). COAG statement on the Closing the Gap Refresh. Canberra: Council of Australian Governments.
- National Congress of Australia’s First Peoples. (2016). The Redfern statement: Aboriginal and Torres Strait Islander peak organisations unite. Sydney: National Congress of Australia’s First Peoples.
- Referendum Council. (2017). Uluru statement from the heart: Referendum Council.
Footnotes
A group of health conditions which includes: ischaemic heart disease (including heart attack and angina); cerebrovascular disease (including stroke); heart failure; oedema (fluid retention); diseases of arteries, arterioles and capillaries.
Hospitalisations for the combined diagnostic groups ST-Elevation Myocardial Infarction (STEMI), Non-ST-elevation myocardial infarction (NSTEMI), Unstable Angina and Heart Failure
‘SA4 Regions’ are statistical regions based on the Australian Statistical Geography Standard (ASGS) according to Statistical Area Level 4. Note that data was not available for some regions for this indicator, including all Tasmanian and most Victorian regions.
The NEHS was a cross-sectional population-based study that included a representative sample of Indigenous people aged 40 years and older (n= 1,738 Indigenous people).
It is not possible to directly compare data from Qld, WA, SA and the NT as the registers are at different stages of establishment and coverage. The NHMRC-funded End Rheumatic Heart Disease Centre of Research Excellence is currently working on a comprehensive data linkage strategy to establish a replicable overview of national ARF and RHD burden.