Review of illicit drug use among Indigenous peoples (peer reviewed)
ReviewCatto M, Thomson N (2008)
Review of illicit drug use among Indigenous peoples. Australian Indigenous HealthBulletin 8(4). Retrieved [access date] from https://healthbulletin.org.au/articles/review-of-illicit-drug-use-among-indigenous-peoples
View PDF version (PDF – 434KB)
Introduction
Drug misuse has significant impacts on families and communities and is a major concern for Australia. The misuse of licit drugs (such as alcohol and tobacco) continues to have the most significant negative impacts, but the use of illicit drugs is also a contributing factor in ill-health, injuries, violence and criminal behaviour, workplace problems and the disruption of family, community and the broader society [1]. For categories and definitions of illicit drugs: view information.
The greater level of substance misuse in the Indigenous population reflects the history of dispossession and oppression of Indigenous people; their entrenched social and economic marginalisation requires holistic and well-funded strategies to address the underlying social determinants of Indigenous ill-health [2].
General aspects of illicit drug use in Australia
Morbidity and mortality
The use of illicit drugs by Indigenous people needs to be seen in the overall context of illicit drug use in Australia (for the extent of illicit drug use in Australia see appendix 1). Illicit drug use accounts for significant morbidity and mortality. There were 8,389 hospital separations in Australia in 2005-06 for which the principal diagnosis was in relation to the four major illicit drug types (opioids, amphetamines, cannabis, and cocaine) [3]. For the period 1993-2006, separations were highest for opioids across the entire period, followed by amphetamines, cannabis and cocaine [4].
In 2005, there were a total of 410 deaths in which opioids (n=374), methamphetamines (n=26) and cocaine (n=10) were determined to be the underlying cause of death among those aged 15-54 years [5, 6]. Opioid deaths are not necessarily heroin; for example, in Tasmania and the Northern Territory deaths are more likely to be related to pharmaceutical opioids [7]. Methamphetamine and cocaine were mentioned in a further 42 and 5 ‘drug-induced’ deaths respectively [6].
In 2003, illicit drug use accounted for 2% of the total burden of disease in Australia [8].
The cost of drug use
The health and economic cost of drug use in Australia is significant. Collins and Lapsley (2008) estimated the total social cost (burden of disease) of drug use in Australia in 2004-05 to be $56.1 billion, of which $8.1 billion (15%) related to the cost of illicit drug use. In real terms this represents an increase of 11.3% in the annual total social cost of illicit drug use in Australia from $6.1 billion in 1998-99 (representing $7.3 billion in 2004-05 figures) to $8.1 billion in 2004-05 [9].
In 2002-03, a total of $3.2 billion was spent by governments in relation to illicit drugs; law enforcement-related activity accounted for 75% of spending, and prevention, treatment, and harm reduction accounted for 10%, 7%, and 1% respectively [10]. Proactive spending (the direct actions of government in relation to drug policy), accounted for 42% ($1.3 billion) of total government expenditure; law enforcement-related activity accounted for more than half of proactive spending (56%), prevention, treatment, and harm reduction accounted for 23%, 17%, and 3% respectively [10].
The extent of illicit drug use among Indigenous people
Evidence of illicit drug use among Indigenous people – population surveys
According to recent population surveys (2004-2005 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS); 2007 National Drug Strategy Household Survey (NDSHS)) the overall level of illicit drug use in the previous 12 months among the Indigenous population aged 15 years or older living in non-remote areas (28%) was more than twice the level of the general Australian population aged 14 years or older (13%) (Figure 1) [11, 12]. The higher level of drug use applied across all drug types.
For both the Indigenous population and the general Australian population cannabis was the most commonly used illicit drug. For the Indigenous population cannabis was followed by amphetamines, analgesics (painkillers) and then ecstasy; in the general Australian population cannabis was followed by ecstasy, analgesics and then amphetamines [11, 12].
Figure 1 Proportions of illicit drug use in the previous 12 months for the Indigenous and general Australian populations, by drug type, Australia, selected years
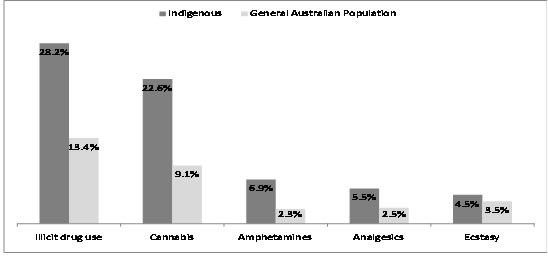
Sources: 2004-2005 NATSIHS [13]; 2007 NDSHS [12]
Note: Proportions are for: (1) Indigenous people aged 15 years or older living in non-remote areas; and (2) general Australian population aged 14 years or older
The overall level of illicit drug use in the previous 12 months by Indigenous people aged 15 years or older living in non-remote areas was 4.7% higher in 2004-2005 than in 2002 (Figure 2) [11]. This change reflects a 20% increase in the number of Indigenous people using illicit drugs in this 2-3 year period. The increase in cannabis use (18%) was around the same as the overall increase, but the increases in amphetamine and ecstasy use were much greater (46% and 137% respectively) [11].
Figure 2 Changes in proportions of Indigenous people using illicit drugs, by drug type, Australia, 2002 and 2004-2005
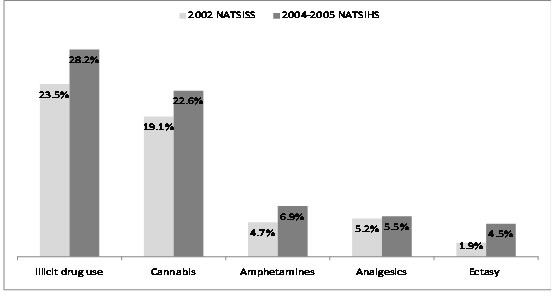
Sources: 2002 NATSISS [14]; 2004-2005 NATSIHS [13]
Note: Proportions are for Indigenous people aged 15 years or older living in non-remote areas
For information on sources and limitations of information on illicit drug use among Indigenous people see appendix 2.
Polydrug use
Use of an illicit drug does not occur in isolation and is often associated with other health-risk factors. According to the 2004-2005 NATSIHS, 12% of Indigenous males and 7% of Indigenous females had used three or more illicit substances in the previous 12 months [11].
Generally, Indigenous people who had used illicit drugs in the previous 12 months were more likely than those who had never used illicit drugs to smoke (66% compared with 34%) and to consume alcohol at risky or high risk levels (28% compared with 13%) [15].
Evidence from other sources
Age of first use
Data relating to the age of Indigenous people when they first use drugs is based mostly on small surveys (Cannabis: Gray et al, 1997; Dance et al, 2004; Clough et al, 2004. Injecting drug use: Larson, 1996; Shoobridge et al, 1998). It indicates that the mean age of first use for illicit drugs is up to 6 years younger than the national average: 12-17 years for cannabis (18 years non-Indigenous) and 17-18 years for injecting drug use (21 years non-Indigenous) [12, 16].
Cannabis use in remote communities
The use of cannabis by Indigenous people in remote communities in Arnhem Land has increased dramatically over the past 20 years or so [17]. Cannabis use was not detected in the ‘Top End’ communities in the mid 1980s, but the most recent research found 67% of males and 22% of females aged 13-36 years were currently using cannabis; these figures represent cannabis use among males more than twice that reported in the late 1990s for males aged over 15 years (31%) and cannabis use among females nearly three times that reported in the late 1990s for females aged over 15 years (8%).
In comparison with figures from the 2004-05 NATSIHS, this equates to cannabis use among Indigenous males in remote communities more than twice that of their non-remote counterparts (28%), and cannabis use among Indigenous females in remote communities nearly one third higher than their non-remote counterparts (17%) [13].
Illicit drug use other than cannabis
Emerging evidence supports a preference among Indigenous injecting drug users for amphetamines over heroin; this is most likely a reflection of the longer lasting euphoric effects of amphetamine and its economic affordability in comparison to heroin [18]. With evidence that amphetamine use is increasing among Indigenous people there are fears that non-Indigenous suppliers will use the existing, largely Indigenous, cannabis networks in rural and remote communities for the flow of amphetamines [19].
Polydrug use
Cannabis and other drugs
The studies of remote Indigenous populations in Arnhem Land found that tobacco smokers were more likely than non-smokers to use cannabis and that the likelihood increased as the quantity of cannabis used increased [20]. Cannabis users, who also smoked tobacco, reported smoking tobacco more heavily than non-users of cannabis (although tobacco use had been taken up more recently among cannabis users) [17]. For lifetime users of both tobacco and cannabis, one-third had initiated the use of both substances at the same time [20]. These findings suggest that for those who use both tobacco and cannabis it is likely that their use is heavy in relation to both drugs, with significant impacts on morbidity and mortality.
The Arnhem Land studies also found that petrol sniffers and those who used amphetamines were all cannabis users [17].
Heroin, amphetamines and other drugs
A study of over 300 Indigenous people in South Australia who injected drugs (the largest single study of its type in Australia) found that most people were polydrug users, using about four different drugs within a six-month period. The most common variations were heroin, speed, cannabis, alcohol and tobacco. The drugs most often used in the previous 6 months were heroin (97%), speed (68%), alcohol (66%), cannabis (63%), tobacco (55%), benzodiazepines (34%) and methadone (34%) [21].
Impact of Indigenous illicit drug use
Health impacts
Deaths and hospitalisation
National data on mortality among Indigenous people are not available [22], but data collated by the Health Department of Western Australia found that the deaths of 26 Indigenous males and 14 Indigenous females in 1990-99 had been attributed to the use of drugs other than alcohol or tobacco (age-standardised rates were 11.1 and 5.9 per 100,000 population respectively) [23]. These death rates are similar to those for the total Australian population in 1999: 14 per 100,000 population for males and 5 per 100,000 for females [24].
The only detailed information about hospitalisation as a result of illicit drug use was compiled as a part of reporting against the Aboriginal and Torres Strait Islander health performance framework [11]. Hospitalisation rates for drug-related causes were generally higher for Indigenous people than for non-Indigenous people living in Queensland, Western Australia, South Australia and the Northern Territory in July 2002 to June 2004 (comprising about 60% of the total Indigenous population), particularly for mental/behavioural disorders relating to use of cannabinoids and multiple drugs and psychoactive substances (Table 1).
The trend of increasing prevalence of illicit drug misuse among Indigenous people is reflected in studies by Patterson et al. (1999) and Gray et al. (2001) of increases in morbidity for drugs other than alcohol and tobacco in Western Australia between 1980 and 1995 and 1994 and 2000. Significant increases in admissions for illicit drug use problems and increases in Hepatitis C notification rates and hospital admission rates for conditions related to illicit drug use were reported [23].
Table 1: Hospitalisation related to drug use, by Indigenous status and cause, Queensland, WA, SA and the NT, July 2002 to June 2004
| Cause of hospitalisation |
Indigenous
|
Non-Indigenous
|
|||
| Poisoning | |||||
| Psychotropic drugs, including antidepressants | 258 | 0.4 | 0.4 | 1.1 | |
| Narcotics, including opium, heroin, methadone and cocaine | 78 | 0.1 | 0.1 | 1.3 | |
| Accidental poisoning | |||||
| Antidepressants and barbiturates | 220 | 0.4 | 0.3 | 1.5 | |
| Narcotics (includes cannabis, cocaine, heroin, opium and methadone) and hallucinogens | 80 | 0.1 | 0.1 | 1.5 | |
| Mental/behavioural disorders | |||||
| From use of cannabinoids | 284 | 0.4 | 0.1 | 4.8 | |
| From use of multiple drugs and psychoactive substances | 269 | 0.4 | 0.1 | 3.0 | |
| From use of other stimulants | 226 | 0.4 | 0.2 | 2.0 | |
| From use of opioids | 60 | 0.1 | 0.1 | 0.9 | |
| From use of sedatives | 15 | – | 0.1 | 0.5 | |
Source: AIHW, 2007 [11]
Notes:
1. Some of the causes of hospitalisation include non-illicit use of drugs
2. Rates are admissions per 1,000 population
3. Rate ratios are the Indigenous rates divided by the non-Indigenous rates prior to rounding of rates for presentation
Hepatitis C and HIV/AIDS
A concerning proportion of Indigenous users of amphetamines and opiates inject their drugs, with a high level of users sharing needles [2]. Findings from the South Australian study on Indigenous injecting drug users found that the people who regularly shared needles (12% of the surveyed participants) were more likely to be dependent, heavy polydrug users and frequent users of amphetamines [21]. These findings have implications for the spread of blood-borne viruses such as Hepatitis C and HIV/AIDS.
Although poor reporting systems make it difficult to determine the rate of viral infection among Indigenous drug users [2], the ‘HIV/AIDS, viral hepatitis and sexually transmissible infections in Australia, Annual Surveillance Report 2007’ found that in the most recent five-year period (2002-2006), the rate of hepatitis C diagnosis increased in both the Indigenous and non-Indigenous population in the Northern Territory (in contrast with a decreasing trend nationally), but was lower in the Indigenous population. The rate of newly diagnosed hepatitis C infection in the Indigenous population of Western Australia and South Australia was between two and three times, and five and 10 times higher respectively than that in the non-Indigenous population [25]. This is likely to be a significant underestimation given that as recently as 2005 Indigenous status was not recorded for 65% of new Hepatitis C notifications [2].
Similarly, despite the equivalency in HIV infection rates between Indigenous and non-Indigenous Australians, Indigenous Australians are more likely than non-Indigenous Australians to contract HIV infection through the use of shared needles. In the most recent five-year period (2002-2006), the ‘HIV/AIDS, viral hepatitis and sexually transmissible infections in Australia, Annual Surveillance Report 2007’ reveals a three-fold increase in the proportion of HIV infections attributed to injecting drug use among Indigenous Australians since the 2000 report (18% compared with 6%), while the non-Indigenous rate has remained unchanged at 3% [25, 26].
Overdose
The National Drug and Alcohol Research Centre (NDARC), in their report ‘Findings from the Illicit Drug Reporting System’ (IDRS), found that 56% of participants using heroin and other opioids in 2007 had overdosed at some point in their lifetime. For participants who used amphetamines, 6% reported overdosing at some point in their lifetime [7]. In 2005, 46% of injecting drug users surveyed in Australia had overdosed at some point in their lifetime [8].
In 2001, a Western Australian study of 74 Indigenous people who inject drugs found that 24% of participants had overdosed at some time [27]. The authors note that these findings contrast with the findings of Larson (1996), where 52% of Indigenous heroin users had personally experienced overdose, however the lower overdose rate in the Western Australian study was attributed to a lesser use of heroin [27]. In 2002, a South Australian study of Indigenous injecting drug users found that 21% had overdosed after injecting, and in contrast to the Western Australian study, 97% of participants had used heroin in the last six months [21]. These figures suggest the overdose rate for Indigenous injecting drug users is variable; being less than or equal to that of the general Australian injecting drug user population.
The concern for Indigenous injecting drug users relates to the stigma and shame of injecting drug use and the associated increased risks of overdose when injecting alone to conceal drug use from family and friends [28].
Social and emotional wellbeing
The 2002 NATSISS found that Indigenous people experience stressors in their lives at a rate one and a half times that of the non-Indigenous population [14]. The most common stressors reported in the 2004-05 NATSIHS were the death of a family member or close friend (42%), serious illness or disability (28%), alcohol and other drug related problems (20%), family member in jail (19%), and inability to get work (17%) [15]. Indigenous people are also hospitalised for mental disorders at twice the rate of other Australians, with the greatest excess of mental health-related hospitalisations in the younger adult age groups and the greatest excess of mortality in the 35-54 year age group [1].
Findings from hospital data and mental health service providers suggest Indigenous people have significantly more mental health disorders associated with illicit drug misuse than non-Indigenous Australians. The National Hospital Morbidity Database found that Indigenous Australians were hospitalised for mental/behavioural disorders from use of cannabinoids and from use of multiple drug and psychoactive substances at a rate 5 times and 3 times respectively that of non-Indigenous Australians [11]. Similarly, Indigenous people presenting to public mental health services are nearly 3 times more likely to have a principal diagnosis of disorders due to psychoactive substance use than non-Indigenous Australians (8% compared with 3%) [29].
Co-morbidity
Co-morbidity is the co-occurrence of more than one disease or disorder in an individual. It is known that mental health problems co-occur with drug use problems and that both may influence each other. Co-morbidity of substance use disorders with psychosis, anxiety, affective, personality and other substance use disorders is widespread and treatment outcomes are often poor [30].
The National Survey of the Mental Health and Wellbeing of Adults (SMHWB) conducted in Australia in 1997 provided information on prevalence rates of mental disorders, including anxiety, affective and substance use disorders among the Australian population. Although a significant survey, and the first of its kind, it did not cover people in remote areas and the number of Aboriginal and Torres Strait Islander people who took part in the survey was too small to provide reliable estimates of their mental health [31, 32].
The SMHWB found significant rates of comorbidity among the general Australian population. Of those with a substance use disorder, 31% also had another mental disorder [32]. Although there are no comprehensive studies of co-morbidity among Indigenous people it is likely that the rates of co-morbidity are higher than those of the general population [2].
Suicide
Over the last decade the Indigenous suicide rate has grown compared to that of non-Indigenous people [15]. For the period 2001-2005, the Indigenous suicide rate was 3 and 4 times higher for males (0-24 years and 25-34 years respectively) and 5 times higher for females (0-24 years) compared with the corresponding age-specific rates for non-Indigenous males and females. Between 1997 and 2000 the Indigenous suicide rate was 1.8 times higher for males and 1.3 times higher for females than their non-Indigenous counterparts [16].
Whereas alcohol remains the drug most associated with suicidal ideation, various studies have shown that intoxication from drugs other than alcohol also facilitates the suicide decision: Clough and colleagues (2006) found a slight increase in the incidence of self-harm (including suicide attempts) among cannabis users; Shoobridge and colleagues (1998) found that more than half of injectors had attempted suicide at least twice, and just over 90% of those attempting suicide were intoxicated at the time [16]. In the Northern Territory there has been an 800% increase in Indigenous suicide over the period 1981 – 2002. Those most at risk are Indigenous males aged 45 years and under. In 2000-2002 misuse of drugs other than alcohol was identified in 16% of cases [33].
Impact on families
Relationships
The impact of drug use on families is significant. In an Adelaide study of Indigenous injecting drug users, half of those interviewed cited family breakdown as a result of injecting drug use [21]. Similarly, in a Western Australian study in 2001, users were overwhelmingly more concerned about the impact of their drug use on family and close relationships (60%) than the impact on their own health (9%) [27]. Relationships suffer on many levels, and a constant tension relates to sourcing money for substance use [19].
Violence
Family violence was a recurring concern of community members in remote areas; the heavy use of cannabis was believed to compound the violence arising from the use of alcohol, kava or inhalant misuse. The majority of police in remote areas (76%) also believed cannabis use contributed to domestic/family violence [19].
The increasing levels of amphetamine use (especially among those with a predisposition for violence) is also likely to increase the levels of violence in communities already experiencing high levels of violence [18].
Whereas illicit drug users are often associated with the perpetration of violence, Indigenous Australians who used at least one illicit drug in the past 12 months were more than twice as likely to have been a victim of physical or threatened violence compared with those who did not use illicit drugs (41% compared with 18%) [29].
Child harm
In remote areas, communities expressed concern for child neglect and the sexual exploitation of young people in relation to drug use. This concern was echoed by police who associated cannabis use with disruption to schooling and with children trading sexual favours for money or drugs [19].
The influence of parental illicit drug use on children was highlighted in a West Australian survey which found that children of parents who used drugs other than alcohol or tobacco were more than twice as likely to use marijuana than children whose parents did not use illicit drugs (24% compared with 11%), were more likely to both smoke and to use marijuana and were more likely to drink alcohol and to drink to excess than those children whose parents did not use illicit drugs [34].
Crime and incarceration
Indigenous people are incarcerated at highly disproportionate rates compared with the non-Indigenous population. Data from the National Prisoner Census showed that at 30 June 2007, 6,630 prisoners were Indigenous – an increase of 9% on 2006 numbers and representing 24% of the total prisoner population (unchanged from 2006). Using age-standardised rates, Indigenous people were 13 times more likely to be in prison than non-Indigenous people (also unchanged from 30 June 2006); in Western Australia Indigenous people were 21 times more likely to be in prison than non-Indigenous people – the highest Indigenous to non-Indigenous rates of imprisonment in Australia [35].
In 2005, data from the Australian Institute of Criminology (AIC) Drug Use Monitoring in Australia (DUMA) survey (carried out in Queensland, New South Wales, South Australia and Western Australia), which collects information on illicit drug use from recently arrested detainees, found that positive drug tests were returned for a higher proportion of Indigenous detainees than non-Indigenous detainees in all seven of the police stations surveyed; the proportion returning positive drug tests ranged from 62% and 85% for Indigenous detainees compared with 47% and 73% for non-Indigenous detainees. For both Indigenous and non-Indigenous detainees who tested positive to drugs, cannabis was the most common drug and benzodiazepines and methamphetamine were also common [11].
Examination of the 2002 NATSISS found that the two most important factors relating to Indigenous prosecution and imprisonment were high-risk alcohol consumption and illicit drug use [36]. Use of certain drugs is, to some degree, associated with specific criminal activities: cannabis and inhalant use is associated with property damage, intravenous drug use is associated with sex work, and alcohol is associated with violence. Various studies have shown that the more common forms of criminal activities carried out by Indigenous drug users are stealing, break and entry, vandalism, gambling, dealing and violent crime such as assault. [16]. Supporting this, data from the National Prisoner Census showed that at 30 June 2007, acts intended to cause injury and unlawful entry with intent accounted for over 43% (2,204) of imprisonment for Indigenous prisoners [35].
Economic costs
In remote communities it is likely that substance users spend a significant proportion of their income on cannabis alone: up to a third of their weekly median income of $160/week for those aged 13-36 and representing 6-10% of the total monetary resources in these communities [17]. While much of this money remains in the community, it places significant strain on the users themselves and their families. In a South Australian study in 2001, Indigenous injecting drug users experienced significant financial problems. The average weekly expenditure on injectable drugs among Indigenous users ranged from $50 to $2100, with the median cost per ‘taste’ being $75 [21]. This spending occurred within the context of a median average income of $350 per week [16].
The high costs associated with funding illicit drug dependence account, at least in part, for the increased rate of involvement in crime [36].
Factors contributing to illicit drug use among Indigenous people
Historical context of Indigenous disadvantage and illicit drug use
A political economy perspective of Indigenous disadvantage views political and economic factors as broadly determinative of the more microbiological, psychological and social/cultural factors that influence the behaviour of individuals and groups [37]. Indigenous people experience significant disadvantage across all socioeconomic indicators, including income, education, employment and housing conditions [29]. Gray and colleagues (2007) illustrate that the root of this disadvantage lies in the dispossession and oppression of Indigenous people since the arrival of the British in 1788. The British claimed Australia on the grounds of terra nullius (a legal term meaning the land was unoccupied and belonged to no one) despite the fact that an estimated 750,000 people lived in Australia, with ancestry dating back more than 60,000 years. Around the turn of the twentieth century ‘social Darwinism’ (which held that less technologically complex societies would give way to more technologically complex societies) was used to justify the continued dispossession of Indigenous people. It was considered that Indigenous people would die out, a belief that was actively assisted through the establishment of poorly resourced missions and government settlements which closely regulated every aspect of Indigenous lives. In this environment children of mixed descent were taken from their parents and their culture ‘for their own good’. Indigenous people were denied access to mainstream society; education was denied and employment was limited to the most basic and menial roles. Such overt discrimination continued through until the implementation of policies of assimilation from the 1950s, but it was not until 1962 that Indigenous people were able to vote and it was not until 1967 that the Commonwealth could pass laws in relation to Indigenous people [2].
The period of assimilation denied Indigenous people their culture and gave way to policies of self-determination in the 1970s, but this era ended in non-Indigenous declarations of failure and a return to more assimilationist policies in the beginning of the twenty first century [2]. Within this political economy context the social determinants of health weigh heavily on Indigenous people.
Social determinants of health
Education
Education is a critical pathway to employment opportunities and associated increased living standards. In 2007, the Australian Bureau of Statistics and Australian Institute of Health and Welfare (2008) reported that the retention rates for Indigenous people in years 10, 11 and 12 were around 10%, 20% and 30% less respectively than the non-Indigenous retention rates for those years. In 2006, Indigenous people aged 15 years and over were half as likely as non-Indigenous people to have completed school to year 12 (23% compared with 49%) and twice as likely to have left school at year 9 or below (34% compared with 16%). Indigenous people living in rural areas and remote areas were less likely to have completed year 12 than their urban counterparts (22% and 14% respectively compared with 31%). [15]. Lowell and colleagues (2003), found that Indigenous people from rural and remote communities in the Northern Territory believe that the loss of cultural knowledge has contributed to the poor health status of their people and that better health is not dependent on improved Western education, but rather cultural education related to health issues, cultural systems and knowledge [38]. Schwab (2006) provides support for these beliefs, suggesting that the quality and cultural appropriateness of education are important factors in determining the influence of education on health outcomes for Indigenous people [38].
Various studies have explored the link between educational outcomes and substance use: A study of two remote communities in Arnhem Land found that current cannabis users were less likely to participate in education or training [17]; in an Adelaide study of injecting drug users the average age of leaving was 15 years [21]; and a study by Gray and colleagues (1997), showed that children aged 8-17 disaffected from school were 23 times more likely to be ‘polydrug users’[23].
Employment
As with education, the relationship between employment and drug use is circular. An environment of underemployment or unemployment is more likely to sustain drug use, and established drug use is more likely to inhibit the ability or desire to work [16]. In 2006, one-third (33%) of Indigenous young people (aged 18-24 years) were fully engaged in work or study; less than half the rate of non-Indigenous young people (71%). In remote areas, less than one-fifth (18%) of Indigenous young people (aged 18-24 years) were fully engaged in work or study [15].
The low rates of engagement in work or study for Indigenous people compared with non-Indigenous people can be compared with the higher rate of drug use in the previous 12 months for Indigenous people aged 15 years or over compared with non-Indigenous people aged 14 years and over (28% compared with 13%) [11, 12]. For Indigenous people in remote areas the lower rate of engagement in work or study compared with Indigenous people in non-remote areas reflects an even greater rate of illicit drug use: in remote communities, 67% of males and 22% of females aged 13 years and over currently use cannabis compared with 28% of males and 18% of females aged 15 years and over in non-remote areas [11, 17]. These figures represent an inverse relationship between active engagement in work or study and drug use.
Similarly, low employment rates were characteristic of injectors in an Adelaide study where two-thirds were unemployed and only 3% had stable employment. [21]. Polydrug use may also be more common among the unemployed: most injectors in the Adelaide study cited above were polydrug users and unemployed youth aged 15-17 were 13.5 times more likely to be ‘frequent polydrug users’ [23].
Income
Studies show a clear and consistent relationship between individual level of income and level of morbidity and mortality, with the highest rates of morbidity and mortality experienced by those on the lowest income [22]. In 2006, the median equivalised gross household income of Indigenous Australians was equal to 56% that of non-Indigenous Australians ($362 compared with $642) [15].
The relationship between income and health status has been contested at the population level for Western industrialised countries where an association between income and life expectancy has not been found. Attention has therefore focused on the contextual effects of inequality; the way in which factors such as social status rather than income per se influence health status. For Indigenous Australians the experience of ‘long-term social exclusion and material marginalisation’ is manifest in their much lower life expectancy [22]. How low income and low social status impact on illicit drug use relates to the association between social determinants such as unemployment, homelessness and poverty and behaviours that damage health – including illicit drug use; some have found the association is strongest between deprivation and licit and illicit drug use, although evidence suggests that this association is mediated by risk and protective factors [22]. Importantly, Indigenous poverty cannot be viewed directly through the lens of mainstream social determinant models of health without also considering the complex interplay between the ‘social, political and economic consequences of being an Indigenous person in Australia’ [39].
Housing
Overcrowding is associated with adverse health outcomes including higher rates of smoking and drinking at hazardous levels [15]. In 2006, around one quarter of the Indigenous population (27% or 102,300 people) were living in overcrowded conditions; 23% of Indigenous households had 5 or more people resident, and in Indigenous or mainstream community housing (representing 55% of the housing tenure in remote areas) an average of 4.8 people are resident per household [15].
No specific studies have investigated the relationship between overcrowding and illicit drug use, but it seems likely that rates of illicit drug use would also be higher. The Northern Territory’s Select Committee on Substance Abuse in Communities (2007) found that levels of stress attributable to overcrowding resulted in greater harms from substance abuse and recommended that the highest priority be given to alternatives to current approaches to housing in remote communities [40].
Family and social factors
Family functioning and resilience is a protective factor just as family stressors (grief, domestic violence, ‘absent’ parents) are a risk factor. Family stressors are commonplace in communities where substance use is problematic [16].
Inducement by friends, or peer pressure, is a major influence in the initiation of drug taking. Among the general Australian population peer pressure was the second most common factor for first use (54%) after curiosity (77%) [41]. The influence of the peer group is likely to be stronger among those for whom home life is stressful [16].
In communities where drug use is not problematic it has been found that meaningful activity (and not necessarily paid work) is a protective factor. So too, recreational activities including sport and cultural activities are considered a crucial primary intervention, particularly in those areas where there is little structured social activity [16].
Policies and strategies addressing illicit drug use among Indigenous people
National Strategic Framework for Aboriginal and Torres Strait Islander Health 2003-2013 (NSFATSIH)
The NSFATSIH is historically based in the articulation of the health aspirations of Indigenous Australians as set out in the National Aboriginal Health Strategy (1989) [42]. The NSFATSIH aims to direct government action over the next ten years using a coordinated, collaborative and multi-sectoral approach [43]. Social and emotional wellbeing is a priority area of the framework which recognises the impact of alcohol and other drug misuse on the health and wellbeing of Indigenous people. The NSFATSIH supports the aims and activities of the National Drug Strategy Aboriginal and Torres Strait Islander Peoples’ Complementary Action Plan [43].
The National Drug Strategy
The National Drug Strategy (developed by the Ministerial Council on Drug Strategy (MCDS)) is an umbrella framework which seeks to reduce the harmful effects of drugs and drug use through a series of national action plans addressing tobacco, alcohol, school-based drug education and illicit drugs [44].
Harm minimisation
Since 1985 Australia’s drug strategy has embraced the principle of harm minimisation to reduce drug-related harm. Harm minimisation refers to the policies and strategies of supply reduction, demand reduction and harm reduction which seek to reduce drug-related harm by improving the health, social, and economic outcomes for both the individual and the community [44].
Supply reduction strategies seek to reduce the production and supply of illicit drugs and to control and regulate licit drugs [45].
Demand reduction strategies seek to reduce demand for substances and include strategies aimed at preventing the uptake of harmful drug use as well as strategies aimed at reducing drug use [45].
Harm reduction strategies seek to reduce drug-related harm for individuals and communities while not necessarily reducing drug use [45]
Funding
In 2002-03, proactive spending (the direct actions of government in relation to drug policy), accounted for 42% ($1.3 billion) of total government expenditure in relation to illicit drugs ($3.2 billion); law enforcement-related activity accounted for more than half of proactive spending (56%), prevention, treatment and harm reduction accounted for 23%, 17%, and 3% respectively [10].
National Drug Strategy Aboriginal and Torres Strait Islander Peoples’ Complementary Action Plan 2003-2009
The Aboriginal and Torres Strait Islander Complementary Action Plan was developed in recognition of the particular challenges Indigenous people are faced with in reducing the harm arising from substance use and provides national direction for the reduction of harm, complementing all other existing national action plans under the National Drug Strategy Framework [44].
Roles and responsibilities
The Aboriginal and Torres Strait Islander Peoples’ complementary action plan stresses the need for a whole-of-system response based on effective partnerships across levels of government, across portfolios, with Aboriginal and Torres Strait Islander community-controlled organisations, and with the communities themselves to ensure the best use of available resources in minimising the harms arising from substance use [46].
Key result areas
The following six key result areas shape the action plan [16]:
- building individual, family and community capacity to address current and future issues in the use of alcohol, tobacco and other drugs, and promote their own health and wellbeing
- actively promoting a whole-of-government commitment, alongside collaboration with community-controlled services and non-governmental organisations, in reducing drug-related harm
- improving access to the appropriate range of health and wellbeing services that play a role in addressing alcohol, tobacco and other drug issues
- recognising the role of holistic approaches from prevention through to treatment and continuing care that is locally available and accessible
- introducing and improving workforce initiatives to enhanced capacity of community-controlled and mainstream organisations to provide quality data
- increasing ownership and sustainable partnerships for research, monitoring, evaluation and dissemination of information
Performance indicators
The National Illicit Drug Action Plan performance indicators are as follows [46]:
- prevalence of use in the previous 12 months in the general population and by young people under 25 years of age
- perception that it is all right to use drugs regularly (at least monthly)
- purity and price of illicit drugs
- number of community-based episodes of care
- number of people diverted to treatment from the police
- participation in treatment by Aboriginal and Torres Strait Islander peoples’, and people from culturally and linguistically diverse backgrounds
- number of people receiving methadone treatment at mid-year census
- number of fatal overdoses
- incidence of HIV diagnoses attributable to injecting drug use
- illicit drug use among arrestees
Specific national indicators for the National Aboriginal and Torres Strait Islander Complementary Action Plan 2003-2006 are as follows [46]:
- an increase in the capacity to report nationally on improvements for Aboriginal and Torres Strait Islander populations in meeting the mainstream performance indicators specified by the substance-specific national action plans
- the number of regional health plans developed under the partnership agreements that incorporate ATOD strategies listed in the complementary action plan
- evidence that all appropriate workforce, research, and evaluation and monitoring actions that arise from funding for the substance-specific action plans are developed in line with the intentions of the complementary action plan to improve capacity and to promote holistic models of intervention
Services
Services provided to Indigenous Australians for substance misuse can be conceptualised using the harm minimisation framework of Australia’s National Drug Strategy. This framework uses demand reduction, harm reduction and supply control strategies (explained above) in a tripartite approach to interventions to reduce substance misuse [47].
The interventions under this tripartite approach can be categorised as primary, secondary or tertiary [47]. Primary interventions are those which seek to prevent the uptake of substance use in the first place; secondary interventions are those which address the needs of the user and the problems associated with that use for the individual and the community; tertiary interventions are those which address the treatment and rehabilitation of chronic users as well as the interventions required for those impaired as a result of their use [16].
Demand reduction
Primary interventions
Primary intervention includes strategies addressing the broader social determinants of health as well as health sector specific strategies focussing on education and information on the risks associated with drug use [47].
Social determinants of health
It is widely acknowledged that interventions need to address the social determinants of health that propel Indigenous Australians into drug use [16]. The most essential determinant being education, and particularly secondary education and youth training whereby meaningful employment and recreation are requisite for stemming the tide of boredom, frustration and directionless experienced by so many young Indigenous people.
Recreation
The introduction of recreational activities is especially important in regional and remote settings where few opportunities for recreational activity exist. D’Abbs and McLean (2000) found that success is more likely if a wide range of activities are provided encompassing a greater range of interests inclusive of gender relevant interests [16]. Likewise, the Northern Territory’s Select Committee on Substance Abuse in the Community (2007) found that the provision of recreational activities is a major element of demand reduction and the key to guiding young people away from substance misuse and therefore recommended recreation facilities be accorded due significance in funding priorities by government [40].
Education/information on drug use
Gray and colleagues (2004) describe a range of culturally specific drug use education interventions; health promotion projects including theatre which reflects local and regional circumstances, advertising through regional Indigenous television, and promotional materials developed by Aboriginal Community Controlled Health Services (ACCHSs) using local people on posters and pamphlets. State and territory health departments have also produced culturally appropriate and relevant health promotion materials [47].
The Australian Government funded Aboriginal and Torres Strait Islander Primary Health Care Services, Service Activity Reporting 2003-04 Key Results (SAR) found that all services provided ‘health promotion/education’ but as this is not broken down into specific areas it is not possible to determine what percentage of interventions applied to substance use health promotion [48]. Less than 5% of Australian Government funded Aboriginal and Torres Strait Islander Substance Use Specific Services provided community-based education and prevention programs [49]. Australian Government funded Alcohol and other drug treatment services in Australia provided information and education to 11% of Indigenous clients [50].
Screening
In 2004-05, 20% of Indigenous people had seen a general practitioner in the previous two weeks and 17% had seen an Aboriginal Health Worker in the previous two weeks [13]. Primary health care settings, therefore, provide an ideal opportunity to identify substance use through programs such as ‘Ferret’; a program widely used in ACCHSs which prompt staff to ask about alcohol and tobacco consumption as part of annual health checks [47].
Secondary and tertiary interventions
Secondary interventions include ‘brief intervention’; the advice given by health practitioners on reducing or giving up substance use. Tertiary interventions include treatment, rehabilitation and counselling of chronic drug users [47].
Brief interventions
Brief intervention describes strategies including screening, brief advice, referral to specialist support, counselling and brief motivational interviewing [51]. In a study to determine the feasibility and acceptability of providing brief intervention in an urban Indigenous health setting, brief intervention was found to be ‘culturally appropriate, but barriers to wider administration included lack of time and the complexity of patients’ presenting health problems’ [52, p. 375]. It was also found that the research raised awareness of the utility of brief intervention for substance use in primary health care settings.
The use of primary health care services by Indigenous people (as cited above) provides the ideal opportunity for ‘brief intervention’ for those for whom substance use has become problematic [47].
The Illicit Drug Diversion Initiative (IDDI) in rural and remote Australia
The IDDI is an initiative of the Council of Australian Governments (COAG) which sought early intervention in the prevention of a new generation of drug users. The strategy involves diverting offenders who have had little prior contact with the justice system for drug offences, and/or whose apprehension involves a small quantity of illicit drugs, into appropriate drug treatment services. Diversion can occur via the police or the courts [52].
As at June 2006, 22 of the 32 IDDI-funded programs were operating in rural and remote areas. The IDDI has been responsible for increasing the pathways to drug assessment, education and treatment through the police and court diversion programs as well as increasing the number of locations where alcohol and drug workers operate. The IDDI has also served to increase the involvement of service providers in the assessment, education and treatment of people diverted under the program in 231 rural and remote locations [52].
The IDDI has limited quantitative data about the outcomes of those who have attended diversion programs. In 2005-06, compliance rates indicated that completion for police diversion programs ranged from 56% and 95%, while completion for court diversion programs ranged from 29% to 100%. The extent of positive outcomes for clients (aside from completion rates) cannot be determined due to insufficient evidence, although many service providers believe diversion provides a valuable opportunity to access this important client group [52].
The Alcohol and other drug treatment services in Australia 2006-07 – Report on the National Minimum Data Set (AODTS-NMDS)
The AODTS-NMDS includes Australian Government funded agencies (government and non-government) providing alcohol and/or other drug treatment services. Services which do not fall within the scope of the AODTS-NMDS include Aboriginal and Torres Strait Islander substance use specific services and health care services, treatment services based in prisons, agencies providing overnight stays such as ‘sobering-up shelters’ and health promotion services such as needle and syringe exchange programs [50].
A closed treatment episode is defined as a period of contact having defined dates of commencement and cessation between an agency and a client. In 2006-07, Indigenous clients comprised one in ten closed treatment episodes (10%), unchanged from the previous three reporting periods [50].
Treatment episodes among the 10-19 years age group were more common for Indigenous clients than non-Indigenous clients (18% compared with 11%); for those aged over 40, Indigenous clients were less common than non-Indigenous clients. These differences may relate to the younger age structure of the Indigenous population compared with the non-Indigenous population [50].
Indigenous clients reported the same drugs of concern as the total population – alcohol, cannabis, opioids and amphetamines; alcohol was more likely to be nominated by Indigenous clients (49% compared with 42%) and opioids were less likely to be nominated by Indigenous clients (11% compared with 15%).
The main treatment types involving Indigenous clients were counselling (38%), assessment (18%), withdrawal management (detoxification) (12%), and information and education (11%). Indigenous clients were less likely to receive withdrawal management than non-Indigenous clients (12% compared with 17%), and more likely to receive information and education only, and assessment only, than non-Indigenous clients (11% and 18% compared with 9% and 14%) [50].
Aboriginal and Torres Strait Islander substance use specific services
In 2005-06, 37 out of 40 Australian Government funded Aboriginal and Torres Strait Islander substance use specific services (which comprised 27 residential and 13 non-residential services) responded to the Drug and Alcohol Services Report (DASR) [49].
An episode of care is defined as contact between a client and a staff member and, in contrast to the AODTS-NMDS, any change in treatment or drug of concern does not constitute a new episode of care [50]. Residential episodes of care begin at admission and end at discharge [49]. In the case of ‘other care’ (non-residential care), higher estimates of activity will be recorded as this relates to the number of visits or phone calls between the service and clients. Clients are counted only once regardless of how many times they access assistance during the reporting year [49].
In 2005-06, 28,200 clients were seen by DASR services, of which 21,400 were Indigenous (76%). Approximately 1,900 Indigenous clients received residential care involving 3,700 episodes of care. Approximately 13,000 Indigenous clients received non-residential care involving 49,200 episodes of care [49].
The principal drugs of concern treated by DASR were alcohol, cannabis, amphetamines, tobacco and benzodiazepines [49]. This differs from the AODTS-NMDS which includes opioids in the top four drugs of concern.
The most common methods of providing care reported by DASR services included transport (100%), counselling (97%) and referral services (97%). The most frequently used substance use treatment approach by DASR services was abstinence (43%) [49]. These findings cannot be contrasted with the AODTS-NMDS because they relate to the services provided and approaches used by the services rather than the numbers of clients receiving those services.
Aboriginal and Torres Strait Islander Primary Health Care Services
In 2003-04, 139 of 140 Australian Government funded Aboriginal and Torres Strait Islander primary health care services responded to the Service Activity Reporting (SAR), of which, 138 provided usable data [48].
An episode of care is defined as contact between a client and health service staff for the provision of health care. Approximately 88% of health care episodes were provided to Aboriginal and Torres Strait Islander clients.
At least one substance use program targeting cannabis was offered by around 50% of services and up to 25% of services offered programs for illicit drugs other than cannabis; principally opiates, benzodiazepines and amphetamines. Programs addressing multiple drug use were offered by 30% of services. More generally, substance use issues are covered on an individual client basis as they arise in the course of client care [48].
Harm reduction
Secondary intervention
Loxley and colleagues (2004) noted the programs with the strongest evidential support for harm reduction were needle and syringe distribution to reduce the spread of blood-borne viruses, the use of methadone for opiate dependence to reduce the risk of overdose and blood-borne viruses, and hepatitis B vaccinations [22].
In 2005-06, the DASR found that 27% of services used harm reduction interventions (such as information about safe using practices) in relation to substance use, and approximately 1,170 Indigenous clients received sobering up/residential respite involving 5,220 episodes of care [49]. In terms of injecting drug users, in 2003-04, 30 ACCHSs (22%) operated needle exchange programs [2].
Barriers to treatment
Barriers to treatment for Indigenous Australians relate to the availability of services, the accessibility of services, the cultural appropriateness of services, the range of treatment options and the cost of services.
Availability of services
Remoteness
The Australian Institute of Health and Welfare (2006) has acknowledged the barrier of geography in providing intervention services in remote communities [16]. Multi-function police facilities in remote areas of Western Australia (in which police share remote facilities with staff from the health, education and welfare sectors in an attempt to adequately respond to family violence and child abuse) may provide an opportunity to incorporate substance misuse services (to date, nine remote areas have been prioritised for multi-function police facilities) [53].
Identification of service needs
The Northern Territory’s Select Committee on Substance Abuse in the Community (2007) found that there was a lack of consultation with communities to ascertain their needs and resources and recommended a ‘community audit’ to ensure program provision is prioritised for individual communities [40]. Similarly, Teasdale and colleagues (2008) in their study assessing acceptability and accessibility of mainstream services for Indigenous Australians in a Sydney Area Health Service found that there was a lack of identification of the drug and alcohol needs of people living in the service area [54].
Accessibility of services
In 2005-06, all of the Australian Government funded Aboriginal and Torres Strait Islander substance use specific services who responded to the DASR (37 out of 40 services) provided transport services to clients [49]. This finding highlights the role the provision of transport services play in the accessibility of services. Similarly, where clients are not provided with transport to services there is a need for outreach services; Teasdale and colleagues (2008) identified a lack of outreach services for Indigenous clients needing to access mainstream services in a Sydney Area Health Service. Additionally, a narrow timeframe to access opioid pharmacotherapy was also identified as a barrier to accessibility [54].
Culturally appropriate services
The Australian Institute of Health and Welfare (2006) has highlighted the continuing need to ensure the cultural appropriateness of services. Services need to be more Indigenous ‘specific’, ‘friendly and accessible’ and ‘controlled’. In meeting these requirements non-Indigenous staff require cultural awareness training and adequate support (especially in remote areas) [16]. Similarly, Teasdale and colleagues (2008) identified the need for culturally appropriate clinical services including a culturally appropriate clinic environment, more Indigenous staff, cultural awareness training for non-Indigenous staff, and holistic care including partnerships with Indigenous communities and community services [54].
Range of treatment options
The Australian Institute of Health and Welfare (2006) highlighted the need for the provision of adequate training in alcohol and other drug work for those staff whose skills are lacking, and importantly, to ensure treatment encompasses a broad range of options to minimise treatment drop-out rates reflective of restrictive and incompatible program availability. [16]. Limited treatment options identified by Teasdale and colleagues (2008) included a lack of brief intervention for Indigenous youth as well as limited access to hepatitis C assessment and treatment [54].
Cost of services
The Road to Recovery: Report on the inquiry into substance abuse in Australian communities (2003) found that naltrexone treatment for opioid dependent people, in contrast to alcohol dependent people, is not available through the Pharmaceutical Benefits Scheme and, at that time, incurred a cost of $167.00 for thirty 50mg tablets. The Road to Recovery report also found that the shift from public to private providers in the provision of methadone maintenance resulted in dispensing fees charged by pharmacists ranging from $3.50 to $7.00 per day, placing a considerable financial burden on those individuals already experiencing significant social and economic disadvantage [55]. Reflecting this burden of cost, Teasdale and colleagues (2008) identified a lack of subsidised pharmacotherapy dispensing in community pharmacies for Indigenous clients [54].
Supply reduction
Primary and secondary intervention
Legislative and regulatory interventions in relation to the production, supply, possession and use of illicit substances are supply reduction strategies and can be categorised as both a primary and secondary prevention strategy; seeking to prevent the uptake of use by reducing demand, and minimising existing use by reducing supply [16].
Research by Loxley and colleagues (2004) showed limited evidence for supply reduction strategies and highlighted the need for much more research into those strategies in use [22]. National data from the Australian Crime Commission (2005) shows that for 2003-04 the number of arrests made in relation to drug offences is overwhelmingly for ‘consumption’ rather than supply (80% compared with 20%) [53]. It is unlikely that these arrests deter use given that there are high rates of re-offending among those convicted for illicit drug use [22].
Despite the limited evidence for supply reduction strategies, in 2002-03, 75% of government spending in relation to illicit drugs was spent on crime-related consequences (reactive activity) and law enforcement-related activities (proactive activity) [10]. Similarly, Collins and Lapsley (1996) estimated that in 1992, over 80% of Commonwealth and State government expenditure in relation to illicit drugs was allocated to law enforcement [56].
Those law enforcement strategies aimed at reducing demand among users which showed evidence for implementation included [22]:
- combined law enforcement and community development; operating within a target area and combining partnership development, law enforcement targeting drug offenders, community policing, and community program and infrastructure development
- use of civil penalties to control drug and disorder problems; typically aimed at non-offending third parties to take preventive action to end criminal or nuisance behaviour, for example, bans, injunctions, and restraining orders, and the fulfilment of health and safety regulations
- police crackdowns; designed to move drug dealers and sellers away from a particular area
Law enforcement strategies aimed at suppliers of illicit drugs which showed evidence for implementation was limited to [22]:
- cannabis law reform; those policies designed to reduce penalties for cannabis possession or use
Weatherburn (2006) makes the point that supply reduction strategies are effective in reducing the harms of use by reducing the level of availability, and in fact, have been requested by Indigenous communities (as seen in dry-community initiatives), and espouses the argument for the effectiveness and necessity of supply reduction initiatives as highlighted by the work of Pearson, who views alcohol and other drug addiction as so endemic that they are now the principal cause of disadvantage rather than a symptom of it [57]. Pearson believes the ‘gammon economy’ (dependence on welfare and effective exclusion from the mainstream economy), and the ensuing lack of meaning and purpose, together with citizen rights that were equated with ‘drinking rights’, compounded the effects of dispossession and trauma for Indigenous people, leading to the epidemic of substance misuse and addiction based disadvantage [58]. These views support the initiatives of community driven supply control strategies to disrupt the ‘normalisation’ of harmful substance use.
Policy implications
Funding
Loxley (2004) found that expenditure in Indigenous Affairs over the past three decades has failed to meet the needs of Indigenous Australians or to remedy the social and economic inequalities that underlie and perpetuate substance misuse among Indigenous Australians. This inadequacy of funding includes health services and substance misuse services and has limited the ability to build capacity in communities and community organisations in regard to infrastructure, research capabilities and staff development and support [22].
The inadequacy of funding in substance misuse prevention and treatment services is, in part, a reflection of the national imbalance in expenditure in favour of law-enforcement. As cited previously, in 2002-03, government expenditure in relation to prevention, treatment and harm reduction accounted for only 10%, 7%, and 1% respectively of total spending in relation to illicit drugs, and in terms of proactive spending (the direct actions of government in relation to drug policy), prevention, treatment and harm reduction accounted for only 23%, 17%, and 3% respectively [10].
The disproportionate expenditure in relation to law-enforcement remains despite the Ministerial Council on Drug Strategy (2001) endorsing the statement that “treatment is one of the most effective strategies for preventing drug use, crime and the next generation of problems” [59]. The cost effectiveness of addressing drug problems through treatment is supported by research from the United States which found that for every $1 invested in addiction treatment programs, a return in excess of $12 in the reduction of crime, criminal justice costs and health care savings could be made [60].
The views of Weatherburn and Pearson as to the efficacy of supply reduction (cited above) do not undermine the need for funding in prevention and treatment at least commensurate with that of law enforcement, but rather underline it (especially in relation to engagement with the ‘real economy’). Strategies to address drug-related harms must necessarily address both the causes and the symptoms or risk the complexity of the symptoms (drug use and drug-related harms) overshadowing the causes.
Funding which is insufficient and unbalanced undermines all of the key result areas of the National Drug Strategy Aboriginal and Torres Strait Islander Peoples’ Complementary Action Plan 2003-2009.
Data
The Australian Institute of Health and Welfare (2006) recognises the need to improve the gaps in the information needed to discern the nature of substance use problems, the contextual factors underlying the prevalence and patterns of substance use, and the effectiveness of interventions. Planning, implementation, monitoring and evaluation of interventions cannot be considered truly reflective of, and responsive to, substance use and the harms associated with that use until data collection improves [16]. The most fundamental data gaps are those which enable substance use and Indigenous status to be consistently recorded and therefore allow basic prevalence estimates across locations and population groups – such limitations reduce the usefulness of available information on, for example, contextual factors, information relating to patterns of substance use, and access to services [16].
Primary health care services
Loxley and colleagues (2004) have shown that the link between underlying social factors and substance use has failed to result in a coordinated and holistic approach incorporating substance misuse policy and policies in other portfolio areas such as education, housing and employment. Further, Indigenous community-controlled organisations, all levels of government, and all sectors need to be involved in substance misuse interventions. The utility of Indigenous involvement in substance misuse interventions is highlighted in community action frameworks which emphasise local coalition empowerment and evidence-based investment cognisant of local evidence of elevated risk factors and depressed protective factors [22].
Workforce development
In 2002, funding provided for workforce development in substance misuse specific intervention projects was less than 3% [2].
Single and Rohl (1997), in their evaluation of the National Drug Strategy 1993-1997, recognised that a significant investment in workforce development was essential in improving outcomes in response to drug problems and recommended that training of mainstream health, law enforcement and community officials was required to effectively minimise drug-related harm, and that new developments in prevention, treatment and research needed to be more readily available to health care practitioners, law enforcement officers and the public at large [61].
Research findings highlight the necessity of comprehensive training for those people working in the field of substance misuse treatment. Intervention strategies for those with a substance misuse problem need to be cognisant of the stage of change that an individual is at in order to achieve successful behaviour change [62]. The most frequently used substance use treatment approach reported by DASR was abstinence, which highlights a likely mismatch between program provision and the client’s stage of change. Similarly, the IDDI (cited above) offers assessment, education and treatment to offenders diverted through police and court programs. The outcome of these programs (apart from completion rates) has not been evaluated but it is likely that interventions that do not match an individual’s stage of change are unlikely to be successful.
Demand reduction
Social determinants of health
Research shows that those who have ‘a stake in life’ are more likely to succeed in addressing their substance misuse and highlights the fundamental significance of the social determinants of health [63]. A ‘stake in conventional life’ underpins successful ‘untreated’ behaviour change (natural recovery); those with the most resources and the most to lose from substance misuse are those most likely to terminate their problematic drug use without treatment. Conversely, those who experience a sense of hopelessness are least able to alter their drug taking behaviour. Social policy which attempts to increase a person’s stake in conventional life can serve to prevent future substance misuse as well as provide an anchor for those who become dependent.
The need for a structured approach
A widespread and structured approach to primary prevention at the individual and community level is likely to have the most significant effect on preventing substance use and misuse; to date such a structured approach does not exist for substance use [47].
At the individual level there is no systematic approach in primary health care settings to follow up substance use apart from the use of the ‘Ferret’ program in most ACCHSs which deals with tobacco and alcohol as part of a person’s health check [47]. The need for a culturally appropriate alcohol and other drugs and mental health screening tool to encourage the early identification of Indigenous people at risk has been highlighted by several government reports [64]. The Indigenous Risk Impact Screen (IRIS) is a 13 item screening instrument for ‘alcohol and other drugs and mental health risk’ developed in response to this need. Schlesinger and colleagues (2007) validated IRIS as a brief screening instrument and recommended its use in general health-care settings because it is easily implemented, delivered quickly, is easily comprehended by clients and provides early identification of alcohol and other drug misuse, mental health risks, and enables a timely response to client needs [64]. The realisation of the potential of primary health care services to provide comprehensive substance misuse interventions (highlighted by Gray and colleagues (2004)) would facilitate a seamless and timely response to those individuals screened ‘at risk’.
At the community level projects tend to be small in scale with limited one-off funding [47]. This is highlighted by data from 1999-2000, which showed that preventive programs made up only 21% of all intervention projects targeting Indigenous people. These programs received less than 10% of the allocated funding with almost half receiving only short-term, non-recurrent funding.
Secondary and tertiary intervention
The potential of primary health care services to provide comprehensive substance misuse interventions requires the availability of adequately trained staff with clearly defined roles in substance misuse intervention [47]. The potential capacity of primary health care services to provide ‘brief intervention’ for substance misuse is limited by the fact that other than acute care for injury and illness related to substance use, there are insufficient resources to provide intervention services.
Harm reduction
Currently harm reduction services such as clean needle exchanges are generally not integrated with other substance misuse services. Gray and colleagues (2004) note the potential for primary health care providers to provide a central networking role for substance misuse services, able to take referrals from those involved in services such as clean needle exchanges and other harm reduction strategies, and to provide referrals to other treatment or support services.
Supply control
The Royal Australasian College of Physicians (RACP) recommends that illicit substances be redefined as primarily a health and social issue with funding commensurate with that of law enforcement. Citing research by Loxley and colleagues (2004) of the lack of evidence supporting supply reduction law enforcement strategies, the RACP recommends that supply control strategies undergo a comprehensive economic evaluation to determine their efficacy and to determine the nature and extent of any unintended negative consequences [56]. Similarly, the Northern Territory’s Select Committee on Substance Abuse in the Community (2007) found that there was an over-reliance on supply reduction and recommended that demand reduction and rehabilitation is supported while ensuring supply reduction strategies anticipate and prevent drug substitution [40].
Summary
The use of illicit drugs among the Indigenous population is more than twice that of the non-Indigenous population; the trend shows illicit drug use increasing for all drug types. In remote areas the use of cannabis among Indigenous people is significantly greater than that of their urban counterparts.
The greater and increasing use of illicit drugs among the Indigenous population corresponds with greater and increasing health, social and economic impacts compared with the non-Indigenous population. The health impacts of illicit drug use include increases in morbidity for accidental poisoning involving illicit drugs, significant increases in HIV/AIDS and Hepatitis C rates, higher rates of drug-related mental/behavioural disorders, and the likelihood of significant rates of comorbidity and increases in suicide ideation and completion. Familial and community impacts include stressful family relationships, violence, harm to children and increases in crime and incarceration as well as significant economic costs borne by the individual, the family and the community.
Like the misuse of licit drugs among Indigenous people, the misuse of illicit drugs must be viewed against the backdrop of colonial dispossession and oppression and the continuing legacy of exclusion and marginalisation of Indigenous people in Australia. This context explains the grave disparities in the social determinants of health that exist today for Indigenous people compared with non-Indigenous people. Indigenous people are significantly less likely to be educated, to be employed, to earn a level of income above subsistence and to live in adequate housing than their non-Indigenous counterparts. Such disadvantage fuels the stressors of life and perpetuates the dysfunction of families and communities; creating the conditions in which solace in drugs is sought.
The National Drug Strategy and the National Drug Strategy Aboriginal and Torres Strait Islander Peoples’ Complementary Action Plan 2003-2009 seek to address illicit drug misuse among Indigenous people through harm minimisation; those policies of demand reduction, harm reduction and supply reduction which seek to improve the health, social, and economic outcomes for both the individual and the community. The key result areas consist of enhancing the capacity of Indigenous people to be involved in the promotion of their own wellbeing, whole-of-government responses to the reduction of drug-related harms, accessibility of services, holistic approaches, workforce initiatives, and sustainable partnerships between all stakeholders inclusive of Indigenous communities in research, monitoring, evaluation and dissemination of information.
The enhancement of the capacity of Indigenous people to be involved in the promotion of their own wellbeing requires significant improvements in education and employment, but the need to address these underlying social factors has not resulted in a coordinated and holistic approach to substance misuse policy and therefore limits several of the key result areas. Similarly, the services available to Indigenous people show a lack of primary interventions for demand reduction, with a reliance on treatment rather than prevention. The unproven over-reliance on supply control strategies and the associated focus on law rather than health are not reflective of a whole-of-government and holistic response to the reduction of drug-related harms and may in fact add to the burden of harm for the user. Fundamental to all of the key result areas is an appropriate level of funding commensurate with need; underfunding and the nature of short-term non-recurrent funding undermines the ability to make tangible and lasting improvements in Indigenous health status including illicit drug misuse and its impacts.
Effective prevention and treatment (ensuring that we are not dealing with an endless flow of symptoms) rests primarily with equity in the social determinants of health. Evidence shows us the pervasive role disadvantage plays in the stark disparities in health status experienced by Indigenous people compared with non-Indigenous people; illicit drug misuse is intrinsically a part of this picture – it is perpetrated by disadvantage, thrives in disadvantage and compounds disadvantage.
The challenge for government to address the social inequity experienced by Indigenous people remains. The change of government in November 2007 has brought the opportunity for a new beginning in Indigenous affairs. The ‘Sorry Day’ speech of the Rudd Government on 13 February 2008, formally acknowledging and expressing sorrow for the wrongs of past policies in relation to the ‘Stolen Generations’, is an important first step of healing for Indigenous people and gives us reason as a nation to hope that the will of government is now such that ‘closing the gap’ is more than rhetoric.
Appendix 1
Extent of illicit drug use in Australia
According to the 2007 National Drug Strategy Household Survey First Results (NDSHS) 1 [12]
- 38% of Australians aged 14 years or older (more than 6 million people) had used an illicit drug at least once in their lifetime; 13% (more than 2 million people) had used an illicit drug at least once in the previous 12 months
- cannabis was the most common illicit drug used – 33% of the population had ever used the drug and 9% had used in the previous year
- recent use of illicit drugs was most common among people aged 20-29 years of age (with almost one-third of males and one quarter of females using an illicit drug in the previous year), and for those aged 14–19 years (with around one-sixth of both males and females using an illicit drug in the previous year)
According to the 2004 National Drug Strategy Household Survey 2 (detailed results of the 2007 NDSHS were not available at the time of writing) [41] the highest proportion of recent drug use was for people who were unemployed – more than one-third (32%) had used an illicit drug recently, more than twice the level for the total population (15%).
- recent illicit drug use was more common among the most socioeconomically disadvantaged (17%) than among people in other socioeconomic groups
- illicit drug use in the previous 12 months was more common for people living in remote and very remote regions (19%) than for those living in other regions
- for illicit drugs other than cannabis, use in the previous 12 months was highest for people living in major cities (9%)
Appendix 2
Sources and limitations of information on illicit drug use among Indigenous people
The three main sources of information about illicit drug use among Indigenous people are population surveys; the 2002 National Aboriginal and Torres Strait Islander Social Survey (NATSISS), the 2004–2005 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) and the 2004 AND 2007 National Drug Strategy Household Surveys (NDSHS).
2002 NATSISS
The 2002 NATSISS, a household survey conducted by the ABS, collected information from 9,400 Indigenous people aged 15 years or older [14]. Respondents lived in private dwellings and came from all states and territories. The ABS plans to conduct the survey every six years.
Limitations of this survey include:
- the lack of confidentiality in gathering information, resulting in a tendency for individuals to underestimate substance use (the unreliable nature of the illicit drug use data for people living in remote areas prevented its inclusion altogether) [65]
- it did not include people living in non-private dwellings (according to the 2001 census, 4% of the Indigenous population resides in non-private dwellings [13, 65]
Given the exclusion of people living in remote areas (in 2001, around one-quarter of the Indigenous population [13]) and those living in non-private dwellings (likely to be the most socioeconomically disadvantaged group with the associated higher risks for substance use), the underestimation of illicit drug use among Indigenous people is likely to be significant [65].
2004-2005 NATSIHS
The 2004–2005 NATSIHS, also a household survey conducted by the ABS, collected information from 10,439 Indigenous people of all ages from remote and non-remote areas of Australia. Information on illicit substance use was collected from people aged 15 years or older living in non-remote areas using a voluntary self-completed form [13]. Thus, the limitations of the 2002 NATSISS also apply to the 2004–2005 NATSIHS.
2004 NDSHS
The 2004 NDSHS, conducted by the AIHW, collected drug use information from 29,445 people aged 12 years or 14 years or older (as specified) residing in private households. Information on illicit drug use was presented for people aged 14 years or older. Only 463 Indigenous respondents were included in this survey and therefore estimates must be interpreted with caution [11, 41].
2007 NDSHS: First results
The 2007 NDSHS, conducted by the AIHW, collected drug use information from 23,356 people aged 12 years or older or 14 years or older (as specified) residing in private households [12]. The analysis presented in almost all of the report relates to Australians aged 14 years and older. The 2007 NDSHS first results do not include information on the number of Indigenous respondents. Detailed findings were not available at the time of writing.
Evidence from other sources
As well as these population surveys, some information about illicit drug use among Indigenous people is available from a number of relatively small-scale studies and special reviews. Examples are the studies of cannabis use among Indigenous people living in remote communities in Arnhem Land, [17] and the reviews undertaken by the Australasian Centre for Policing Research [18] and the Australian Institute of Criminology [19].
References
Australian Health Ministers’ Advisory Council (2006) Aboriginal and Torres Strait Islander health performance framework 2006 report. Canberra: Australian Health Ministers’ Advisory Council
2 Gray D, Saggers S, Atkinson D, Wilkes E (2007) Substance misuse: ch.20. In: Couzos S, Murray R, eds. Aboriginal primary health care: an evidence-based approach. 3rd ed. South Melbourne: Oxford University Press:755-787
3 Australian Institute of Health and Welfare (2007) Australian hospital statistics 2005-06. (AIHW Catalogue no. HSE 50) Canberra: Australian Institute of Health and Welfare
4 Roxburgh A, Burns L, Degenhardt L (2008) Drug-related hospital stays in Australia 1993-2006. Sydney: National Drug and Alcohol Research Centre
5 Degenhardt L, Roxburgh A (2005) Accidental drug-induced deaths due to opioids in Australia, 2005. Sydney: National Drug and Alcohol Research Centre
6 Degenhardt L, Roxburgh A (2007) Cocaine and methamphetamine related drug-induced deaths in Australia, 2005. Sydney: National Drug and Alcohol Research Centre
7 Black E, Roxburgh A, Degenhardt L, Bruno R, Campbell G, et al. (2007) Findings from the Illicit Drug Reporting System (IDRS). (Australian Drug Trends series no. 1) Sydney: Australian Drug Trends
8 Australian Institute of Health and Welfare (2007) Statistics on drug use in Australia 2006. (AIHW catalogue no. PHE 80) Canberra: Australian Institute of Health and Welfare
9 Collins DJ, Lapsley HM (2008) The costs of tobacco, alcohol and illicit drug abuse to Australian society in 2004/05: summary version. Canberra: Department of Health and Ageing
10 Moore TJ (2005) What is Australia’s “drug budget”? The policy mix of illicit drug-related government spending in Australia. Melbourne: Turning Point Alcohol and Drug Centre
11 Australian Institute of Health and Welfare (2007) Aboriginal and Torres Strait Islander Health Performance Framework, 2006 report: detailed analyses. (AIHW Catalogue no. IHW 20) Canberra: Australian Institute of Health and Welfare
12 Australian Institute of Health and Welfare (2008) National drug strategy household survey: 2007 first results. (AIHW Catalogue no. PHE 98) Canberra: Australian Institute of Health and Welfare
13 Australian Bureau of Statistics (2006) National Aboriginal and Torres Strait Islander Health Survey: Australia, 2004-05. (ABS catalogue no. 4715.0) Canberra: Australian Bureau of Statistics
14 Australian Bureau of Statistics (2004) National Aboriginal and Torres Strait Islander Social Survey, 2002. (ABS catalogue no. 4714.0) Canberra: Australian Bureau of Statistics
15 Australian Bureau of Statistics, Australian Institute of Health and Welfare (2008) The health and welfare of Australia’s Aboriginal and Torres Strait Islander Peoples 2008. (ABS Catalogue no. 4704.0 and AIHW Catalogue no. IHW 21) Canberra: Australian Bureau of Statistics and Australian Institute of Health and Welfare
16 Australian Institute of Health and Welfare (2006) Drug use among Aboriginal and Torres Strait Islander peoples: an assessment of data sources. (AIHW catalogue no. PHE 76) Canberra: Australian Institute of Health and Welfare
17 Clough A, d’Abbs P, Cairney S, Gray D, Maruff P, et al. (2004) Emerging patterns of cannabis and other substance use in Aboriginal communities in Arnhem Land, Northern Territory: a study of two communities. Drug and Alcohol Review;23(4):381-390
18 Nicholas R (2004) Apprehension and custodial care of offenders affected by the use of amphetamine type stimulants. Marden, S.A.: Australasian Centre for Policing Research
19 Putt J, Delahunty B (2006) Illicit drug use in rural and remote Indigenous communities. (Trends and issues in crime and criminal justice, no. 322) Canberra: Australian Institute of Criminology
20 Clough AR (2005) Associations between tobacco and cannabis use in remote Indigenous populations in Northern Australia. Addiction;100(3):346-353
21 Holly C, Shoobridge J (2002) Investigating the impact of injecting drug use in Indigenous communities in metropolitan Adelaide. Adelaide: Aboriginal Drug and Alcohol Council
22 Loxley W, Toumbourou JW, Stockwell T, Haines B, Scott K, et al. (2004) The prevention of substance use, risk and harm in Australia: a review of the evidence. Canberra: The National Drug Research Institute and the Centre for Adolescent Health
23 Gray D, Saggers S (2003) Substance misuse. In: Thomson N, ed. The health of Indigenous Australians. South Melbourne: Oxford University Press:158-185
24 Australian Bureau of Statistics (2001) Australian social trends. (ABS Catalogue no. 4102) Canberra: Australian Bureau of Statistics
25 National Centre in HIV Epidemiology and Clinical Research (2007) HIV/AIDS, viral hepatitis and sexually transmissible infections in Australia: Annual Surveillance Report 2007. (AIHW Catalogue no. PHE 92) Sydney: Australian Institute of Health and Welfare
26 National Centre in HIV Epidemiology and Clinical Research (2000) HIV/AIDS, hepatitis C and sexually transmissible infections in Australia annual surveillance report 2000. Sydney: National Centre in HIV Epidemiology and Clinical Research, University of New South Wales
27 Gray D, Saggers S, Atkinson D, Carter M, Loxley W, et al. (2001) The harm reduction needs of Aboriginal people who inject drugs [community report]. Perth: National Drug Research Institute, Curtin University of Technology
28 Coupland H, Ball K, Costello M, Harvey B, Maher L (2005) ‘Something is going to get us’: a consultation and development project for a national campaign addressing injecting drug use in Indigenous communities, final report. Darlinghurst, NSW: Australian Federation of AIDS Organisations and the Australian Injecting and Illicit Drug Users League
29 Australian Bureau of Statistics, Australian Institute of Health and Welfare (2005) The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples 2005. (ABS catalogue no. 4704.0) Canberra: Australian Institute of Health and Welfare and the Australian Bureau of Statistics
30 Teesson M, Byrnes L (2001) National Comorbidity Project. Canberra: National Drug and Alcohol Research Centre
31 Andrew G, Hall W, Teesson M, Henderson S (1999) The Mental Health of Australians. Canberra: Mental Health Branch, Commonwealth Department of Health and Aged Care
32 Australian Bureau of Statistics (1997) Mental health and wellbeing: profile of adults, Australia. (ABS Catalogue no. 4326.0) Canberra: Australian Bureau of Statistics
33 Measey ML, Li SQ, Parker R, Wang Z (2006) Suicide in the Northern Territory, 1981-2002. Medical Journal of Australia;185(6):315-319
34 Zubrick SR, Silburn SR, Lawrence DM, Mitrou FG, Dalby RB, et al. (2005) The social and emotional wellbeing of Aboriginal children and young people: summary booklet. (The Western Australian Aboriginal Child Health Survey, v. 2) Perth: Telethon Institute for Child Health Research and Curtin University of Technology
35 Australian Bureau of Statistics (2007) Prisoners in Australia. (4517.0) Canberra: Australian Bureau of Statistics
36 Weatherburn D, Snowball L, Hunter B (2006) The economic and social factors underpinning Indigenous contact with the justice system: results from the 2002 NATSISS survey. (Crime and justice bulletin: contemporary issues in crime and justice, no. 104) Sydney: NSW Bureau of Crime Statistics and Research
37 Saggers S (2001) Theorising Indigenous health: a political economy of health and substance misuse. Health Sociology Review;10(2):21-33
38 Dunbar T, Scrimgeour M, eds. (2007) Education. Crows nest (NSW): Allen and Unwin
39 Walter M, Saggers S, eds. (2007) Poverty and social class. Crows nest (NSW): Allen and Unwin
40 Select Committee on Substance Abuse in the Community (2007) Substance Abuse in Remote Communities: Confronting the Confusion and Disconnection. Darwin: Legislative Assembly of the Northern Territory
41 Australian Institute of Health and Welfare (2005) 2004 National Drug Strategy Household Survey: detailed findings. (AIHW catalogue no. PHE 66) Canberra: Australian Institute of Health and Welfare
42 National Aboriginal and Torres Strait Islander Health Council (2004) National strategic framework for Aboriginal and Torres Strait Islander Health 2003-2013: context. Canberra: National Aboriginal and Torres Strait Islander Health Council
43 National Aboriginal and Torres Strait Islander Health Council (2004) National strategic framework for Aboriginal and Torres Strait Islander Health 2003-2013: framework for action by governments. Canberra: National Aboriginal and Torres Strait Islander Health Council
44 Ministerial Council on Drug Strategy (2006) National Drug Strategy: Aboriginal and Torres Strait Islander Peoples Complementary Action Plan 2003-2009: background paper. Canberra: Ministerial Council on Drug Strategy
45 Ministerial Council on Drug Strategy (2004) The National Drug Strategy: Australia’s integrated framework 2004-2009. Canberra: Ministerial Council on Drug Strategy
46 Ministerial Council on Drug Strategy (2006) National Drug Strategy: Aboriginal and Torres Strait Islander Peoples Complementary Action Plan 2003-2009: action plan. Canberra: Ministerial Council on Drug Strategy
47 Gray D, Saggers S, Atkinson D, Strempel P (2004) Substance misuse and primary health care among Indigenous Australians: review of the Australian Government’s Aboriginal and Torres Strait Islander Primary Health Care Program. (Consultant report no.7) Canberra: Office for Aboriginal and Torres Strait Islander Health
48 Office for Aboriginal and Torres Strait Islander Health, National Aboriginal Community Controlled Health Organisation (2006) Service activity reporting 2003-2004 key results: a national profile of Australian Government funded Aboriginal and Torres Strait Islander primary health care services. Canberra: Department of Health and Ageing, Australian Government
49 Office for Aboriginal and Torres Strait Islander Health (2007) Drug and alcohol service reporting: 2005-06 key results: a national profile of Australian Government funded Aboriginal and Torres Strait Islander substance use specific services. Canberra: Australian Government Department of Health and Ageing
50 Australian Institute of Health and Welfare (2008) Alcohol and other drug treatment services in Australia 2006–07: report on the National Minimum Data Set. (AIHW Catalogue no. HSE 59) Canberra: Australian Institute of Health and Welfare
51 Brady M, Sibthorpe B, Bailie R, Ball S, Sumnerdodd P (2002) The feasibility and acceptability of introducing brief intervention for alcohol misuse in an urban Aboriginal medical service. Drug and Alcohol Review;21(4):375-380
52 Australian Institute of Health and Welfare (2008) The effectiveness of the Illicit Drug Diversion Initiative in rural and remote Australia. (AIHW Catalogue no. PHE 96) Canberra: Australian Institute of Health and Welfare
53 Delahunty B, Putt J (2006) The policing implications of cannabis, amphetamine and other illicit drug use in Aboriginal and Torres Strait Islander communities. (Monograph series no.15) Canberra: Australian Institute of Aboriginal and Torres Strait Islander Studies and Australian Government Department of Health and Ageing
54 Teasdale KE, Conigrave KM, Kiel KA, Freeburn B, Long G, et al. (2008) Improving services for prevention and treatment of substance misuse for Aboriginal communities in a Sydney Area Health Service. Drug and Alcohol Review;27(2):152-159
55 Standing Committee on Family and Community Affairs (2003) Road to Recovery: report on the inquiry into substance abuse in Australian communities, Illicit drug use: prevention and treatment. Canberra: Parliament of the Commonwealth of Australia
56 The Royal Australasian College of Physicians, The Royal Australian and New Zealand College of Psychiatrists (n.d.) Illicit drugs policy: using evidence to get better outcomes.br />
57 Weatherburn D (2006) Disadvantage, drugs and gaol: re-thinking Indigenous over-representation in prison. Sydney: Bureau of Crime Statistics and Research
58 Pearson N (2001) On the human right to misery, mass incarceration and early death: The Charles Perkins Memorial Oration. Quadrant:9-20
59 National Expert Advisory Committee on Illicit Drugs (2001) National action plan on illicit drugs, 2001 to 2002-03: background paper. Canberra: Ministerial Council on Drug Strategy
60 Macintosh A (2006) Drug law reform: beyond prohibition. (Discussion paper number 83) Canberra: The Australia Institute
61 Roche AM (2002) Workforce development issues in the AOD field: a briefing paper for the Inter-Governmental Committee on Drugs. Canberra: National Centre for Education and Training on Addiction
62 Prochaska JO, DiClimente CC, Norcross JC (1992) In search of how people change: applications to addictive behaviors. American Psychologist;47(9):1102-1114
63 Granfield R, Cloud W (1996) The elephant that no one sees: natural recovery among middle-class addicts. Journal of Drug Issues;26(1: Health module):45-61
64 Schlesinger CM, Ober C, McCarthy MM, Watson JD, Seinen A (2007) The development and validation of the Indigenous Risk Impact Screen (IRIS): a 13-item screening instrument for alcohol and drug and mental health risk. Drug and Alcohol Review;26(2):109-117
65 Chikritzhs T, Brady M (2006) Substance use in the 2002 NATSISS. Canberra: Centre for Aboriginal Economic Policy Research
Endnotes
1 The NDSHS is conducted every three years. In 2007 the sample size was 23,356 persons aged 12 years and over. The analysis presented in almost all of the report relates to Australians aged 14 years and older [12].
2 In 2004 the sample size was 29,445 persons aged 12 years and over. The analysis presented in almost all of the report relates to Australians aged 14 years and older [41].