Review of respiratory diseases among Aboriginal and Torres Strait Islander children
ReviewO’Grady KF, Hall, KK, Bell, A, Chang AB, Potter, C (2018)
Review of respiratory disease among Aboriginal and Torres Strait Islander children. Australian Indigenous HealthBulletin 18(2). From https://healthbulletin.org.au/articles/review-of-respiratory-diseases-among-aboriginal-and-torres-strait-islander-children
Introduction.
About this review
Acknowledgements
Key facts
The context for respiratory health among Aboriginal and Torres Strait Islander children
Factors contributing to respiratory disease
Extent of respiratory disease among Aboriginal and Torres Strait Islander children
Prevention and management
Aboriginal and Torres Strait Islander specific resources for lung conditions
Programs and services
Policies and strategies
Future directions and research needs
Concluding comments
Glossary
Abbreviations
References
View PDF version (675 KB)
The term respiratory disease refers to a number of conditions that affect the lungs or their components [1]; each of these conditions is characterised by some level of impairment of the lungs in performing the essential function of gas exchange [2]. Respiratory diseases, which can be caused by a variety of different factors and other medical problems (which may or may not start in the lungs), are generally divided into two basic categories: acute respiratory infections and chronic respiratory diseases [3].
While respiratory diseases are major causes of poor health across the lifespan and death in Aboriginal and Torres Strait Islander people [4], this review focuses on the respiratory health of Aboriginal and Torres Strait Islander children. In 2012–2013, one-fifth of Aboriginal and Torres Strait Islander children aged 0–14 years were reported to have had a long-term respiratory condition [5]. In 2014–15, they were up to two times more likely to be hospitalised for selected respiratory conditions (asthma, influenza and pneumonia, whooping cough and acute respiratory infections) compared with non-Indigenous children [6]. Selected respiratory diseases (asthma, upper and lower respiratory conditions) were in the top ten specific conditions responsible for the total burden of diseases among Aboriginal and Torres Strait Islander children in 2011 [3]. The high levels of respiratory disease among Aboriginal and Torres Strait Islander children reflect a broad range of contributing factors, which are discussed in this review.
Throughout this review, it important for readers to take into account that Aboriginal and Torres Strait Islander groups vary with regard to geography, socioeconomic status and local customs, and ‘Indigenous’ as a descriptor belies the heterogeneity among cultures and belief systems that impacts on perceptions of disease and treatments. Further, as the review highlights, there is a paucity of high quality data and research that addresses respiratory diseases in children, with most limited to children in remote regions of Western Australia (WA), the Northern Territory (NT) and Queensland (Qld). Hence caution is required in generalising information from limited data to all Aboriginal and Torres Strait Islander children, particularly from data collected in remote communities and applying to urban communities and vice-versa.
About this review
The purpose of this review is to provide a comprehensive synthesis of key information on respiratory disease among Aboriginal and Torres Strait Islander children in Australia to:
- inform those involved or interested in Aboriginal and Torres Strait Islander health
- provide the evidence for future policy, strategy and program development and delivery.
The review provides general information on the historical, social and cultural context of respiratory health, and the environmental and behavioural factors that contribute to respiratory disease. It provides information on the extent of respiratory disease, including: incidence and prevalence data; hospitalisations and health service utilisation; mortality and burden of disease. It discusses the issues of prevention and management of respiratory health, and provides information on relevant programs, services, policies and strategies that address the health issue of respiratory diseases among Aboriginal and Torres Strait Islander children. It concludes by discussing possible future directions for respiratory health in Australia.
This review draws primarily on journal publications and government reports and some national data collections and surveys, the majority of which can be accessed through the HealthInfoNet’s publications database (http://aih-wp.local/key-resources/publications).
Edith Cowan University prefers the term ‘Aboriginal and Torres Strait Islander’ rather than ‘Indigenous Australian’ for its publications. However, when referencing information from other sources, authors may use the terms from the original source. As a result, readers may see these terms used interchangeably with the term ‘Indigenous’ in some instances. If they have any concerns they are advised to contact the HealthInfoNet for further information.
Acknowledgements
Special thanks are extended to:
- the anonymous reviewer whose comments greatly assisted finalisation of this review
- Jane Burns and other staff at the Australian Indigenous HealthInfoNet for their assistance and support
- the Australian Government Department of Health for their ongoing support of the work of the Australian Indigenous HealthInfoNet.
Key facts
The context of Aboriginal and Torres Strait Islander health and respiratory disease
- The factors contributing to respiratory disease among Aboriginal and Torres Strait Islander children reflect a combination of broad historical, social and cultural factors as well as proximal health risk factors.
- Risk factors for respiratory diseases common among Aboriginal and Torres Strait Islander mothers and children include: exposure to tobacco smoke during pregnancy; maternal immunisation during pregnancy; air pollution, maternal nutrition and stress; pre and post natal care of mothers; a child’s home, social and physical environment, family history; nutrition and physical activity.
The extent of respiratory disease among Aboriginal and Torres Strait Islander children
- Aboriginal and Torres Strait Islander children are hospitalised for respiratory diseases at a higher rate than non-Indigenous children.
- Lower respiratory tract infections and upper respiratory conditions were in the top ten conditions contributing to the total burden of disease for Aboriginal and Torres Strait Islander female children.
- Asthma was a leading contributor to the total burden of disease for both Aboriginal and Torres Strait Islander male and female children.
Prevention and management of respiratory diseases
- Prevention of respiratory diseases depends on ongoing changes in socioeconomic disparities between Aboriginal and Torres Strait Islander children and non-Indigenous children, and a reduction in modifiable risk factors.
- Effective respiratory disease management through early detection; use of evidence-based, multi-disciplinary, culturally appropriate management pathways; established models of care and patient heath education, which are easy to access could assist in sustained improvements in respiratory disease care and health outcomes for Aboriginal and Torres Strait Islander children
Programs and services
- Specific Government funded Aboriginal and Torres Strait Islander paediatric outreach respiratory clinics are run in Qld and WA.
- National initiatives that focus on housing, Aboriginal and Torres Strait Islander specific immunisation programs, reducing tobacco smoking, health checks, funding of key research organisations and the monitoring of trends in diseases over time are vital to reducing the burden of disease among Aboriginal and Torres Strait Islander children.
Policies and strategies
- The National Aboriginal and Torres Strait Islander Health Plan 2013–2023 includes an expansion of the focus on child health.
- The National Early Childhood Development Strategy aims to strengthen universal maternal, child and health services.
The context for respiratory health among Aboriginal and Torres Strait Islander children
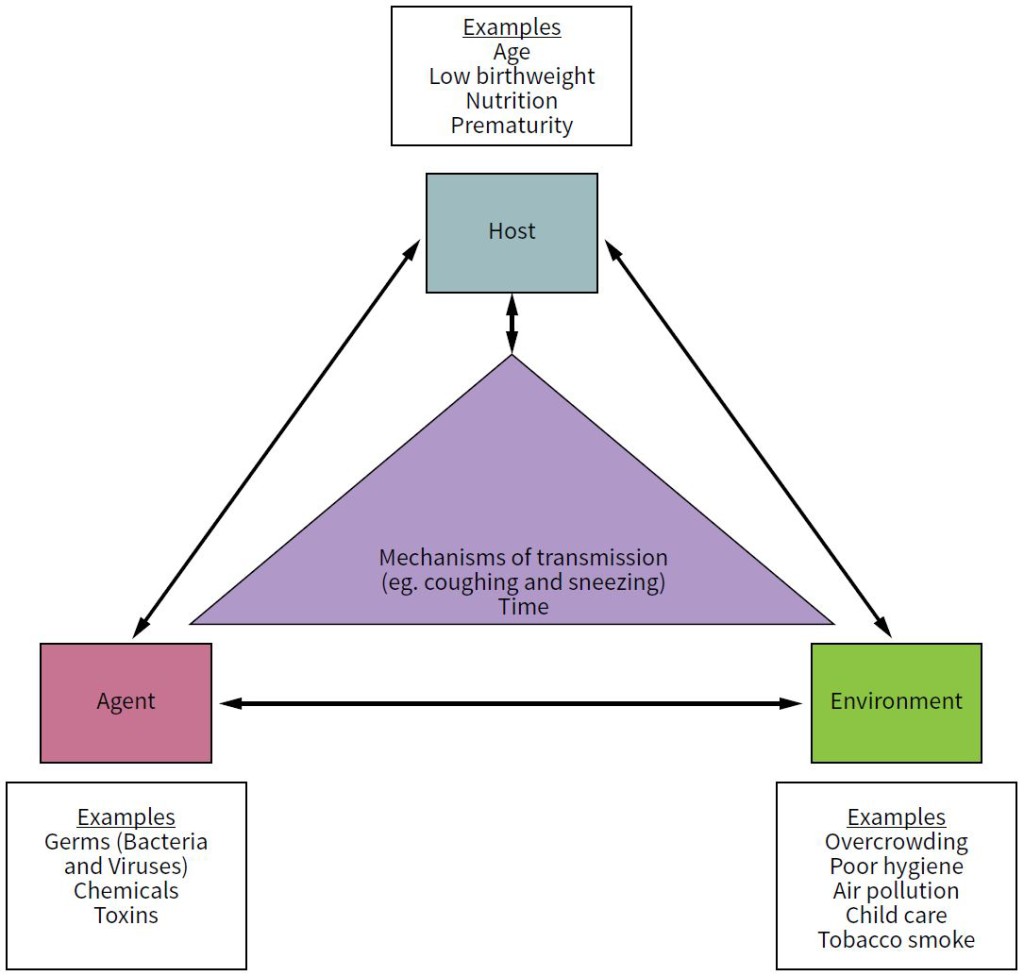
Respiratory diseases, both acute and chronic, are major causes of poor health and death in children worldwide. The burden is highest in children who live in environments of socioeconomic disadvantage, including in wealthy countries such as Australia. Respiratory diseases in children result from complex interactions between multiple factors including genetic, environmental, socioeconomic and demographic characteristics and the relationship between the host, environment, agents responsible for disease (e.g. viruses, bacteria, toxins, chemicals, pollution etc.), the mechanisms by which an agent causes disease, how those agents are transmitted (e.g. inhaled, ingested, direct contact) and time since first exposed to an agent (Figure 1). While it is essential for a person to be exposed to a virus or bacteria to get an infection, whether that person actually gets sick from that infection is dependent on many other factors.
Figure 1. Interactions between the host, the environment and agents in the causal pathways of disease
Source: O’Grady, KF (2018)
A child has unique and different exposure pathways that begin in the pre-conception period and continue into the post-natal period. Children have a dynamic physiology that is turned up on high due to growth and developmental demands that occur during embryonic and foetal life [7]. Further rapid growth and development in the post-natal period – in particular the respiratory, neurological and immune systems – make children vulnerable to environmental exposures. A child’s exposure to environmental stimulants whether they be external, physical, social, cultural, economic or prenatal/antenatal is a major concern in all aspects of children’s health worldwide [8].
Focusing on respiratory health among Aboriginal and Torres Strait Islander children is important as respiratory diseases are common and can be serious. Many chronic lung diseases are potentially modifiable through clinically based interventions, or are preventable. Reasons for this include; (a) the lung continues to grow at least until 7–8 years of age, if not longer; and (b) the pulmonary immunity and respiratory phenotype is influenced by genetic-environmental interactions that commence very early in life (possibly in-utero). It is highly biologically plausible that many common conditions in adulthood emerge from early childhood factors [9] and there is indeed increasing evidence that a substantial proportion of lung disease in adults (such as chronic obstructive lung disease and bronchiectasis) has its roots in childhood (where it is potentially reversible) [9-11].
The historical, social and cultural context
Aboriginal populations were fragmented by colonisation [12, 13]. Traditional life was suppressed and people who had lived with well-established traditional laws, languages, dress, religions, sacred ceremonies, rituals, healers, and remedies were adversely affected [12]. This disruption to physical, social, emotional, mental health and wellbeing in traditional societies was worsened by legalised socioeconomic and political marginalisation and racial prejudice, which was often entrenched and institutionalised [12-15]. The process hastened the dispossession of traditional lands, subsequent poverty, under-education and unemployment. This disempowerment, marginalisation and the cultural destruction of Aboriginal and Torres Strait Islander people are described as transgenerational trauma [12, 16, 17]. The Stolen Generations is a particular example; children were separated from their families, institutionalised, subjected to physical and emotional abuse, racism, maltreatment and little or no exposure to culture, spiritual knowledge and identity [15, 16, 18-21]. These factors, in conjunction with poor living conditions, inadequate nutrition and high exposure rates to infectious organisms are associated with health inequalities and a heavy burden of disease in infants and children. The inequalities of transgenerational trauma in Aboriginal and Torres Strait Islander people led to unsatisfactory disease and health outcomes, impaired emotional and social wellbeing, and poor prospects for future generations [12, 15, 16].Social factors not only have an impact on health across the course of life, but the ensuing health issues may create conditions that subsequently influence health and they represent a well-recognised determinant of health [22-25].
The impacts of colonisation on Aboriginal and Torres Strait Islander people continue to be witnessed today. The current health status of Aboriginal and Torres Strait Islander people is directly linked to the disruption that occurred to cultural, social, holistic and economic way of life [26-28]. For Aboriginal and Torres Strait Islander people, the determinants of good health and health behaviours are broader than socioeconomic issues; these include history, the quality and quantity of relationships with the wider mainstream community, the ability to connect with other Aboriginal and Torres Strait Islander community members, connection to land, the ability to express themselves culturally, and the ability to have personal and community control of issues surrounding their health [27]. Negative health outcomes among Aboriginal and Torres Strait Islander people can be linked to factors such as inadequate housing, poor education and employment outcomes, low income, and poor access to services, loss of identity, poor nutrition, low physical activity, smoking and consumption of alcohol [29]. Underlying causes of these factors include racism and discrimination, forced removal of children, loss of identity, language, culture and land [6]. These factors influence the broader social, cultural and economic environment in which Aboriginal and Torres Strait Islander people live.
Urban Aboriginal and Torres Strait Islanders face many of the same problems of their remote counterparts. Urban dwelling Aboriginal and Torres Strait Islander people can suffer from having their Aboriginality denied and it is assumed that they have assimilated into mainstream society [30]. The stereotype of ‘real’ Aboriginals being those living ‘out bush’ or in ‘traditional’ settings may lead to a denial of the possibility of a dynamic, contemporary Aboriginal and Torres Strait Islander culture [31]. In urban areas, there may be no ‘community’ as such, but a loose network of geographically dispersed family and organisational affiliations not at all obvious to non-Indigenous observers [30, 31]. The needs of those without social networks often go unnoticed and unmet. The disadvantages of cultural isolation can be just as acute as those of geographic isolation. All of the above factors have led to a loss of autonomy which has undermined social vitality, which, in turn, affected the capacity to meet challenges, including health challenges, leading to a cycle of transgenerational dispossession, demoralisation and poor health [32].
Despite the disadvantage and barriers faced by Aboriginal and Torres Strait Islander people since the time of colonisation, communities have survived and many have thrived. This largely reflects the resilience of individuals, their families and communities that has been evident since colonisation and persists today [33]. It is an important strength that needs more recognition in the efforts directed at improving Aboriginal and Torres Strait Islander health [34].
Socioeconomic factors
Socioeconomic factors such as income, education, family structure (e.g. single parent, both parents at home and household size), access to transport, mobile phones, and the internet, geographic location and quality of housing are all important determinants of health. Not only are they important to the prevention of illness but also to the early diagnosis and management of an illness to prevent adverse outcomes. All of these factors are important in the prevention and management of respiratory illnesses in children. The substantial disparity in socioeconomic status between Aboriginal and Torres Strait Islander people and non-Indigenous people [35] is a well-recognised cause of the higher respiratory disease burden in Aboriginal and Torres Strait Islander children [36]. Major changes in this burden are only likely to occur once the socioeconomic disadvantage experienced by Aboriginal and Torres Strait Islander people has been addressed.
According to the 2016 Census, more than one-third (38%) of Aboriginal and Torres Strait Islander people lived in major cities, with 44% in regional areas and 18% in remote areas [37]. There is a gradient in the burden of disease and injury by region of residence in Australia, with those in remote areas experiencing the highest burden, followed by very remote areas [3]. However a lack of data on urban and regional Indigenous children is an important impediment to closing the gap in health disparities [38], given the majority of Aboriginal and Torres Strait Islander people live in those areas. Most research conducted on respiratory diseases in Aboriginal and Torres Strait Islander children has been undertaken in remote areas, or settings with a large proportion of Aboriginal and Torres Strait Islander people (e.g. NT, WA and north Qld). An urban study of the characteristics of young Aboriginal and Torres Strait Islander children registered with a primary health care centre identified levels of socioeconomic disadvantage that were similar to their remote peers [39]. That finding highlights the limitations in applying national or state composite data (e.g. hospitalisations) to describe Aboriginal and Torres Strait Islander disadvantage and health status.
Factors contributing to respiratory disease
The traditional Aboriginal and Torres Strait Islander perspective of health is holistic [40]; it encompasses everything important in a person’s life, including land, environment, physical body, community relationships and law. Health is the social, emotional, and cultural wellbeing of the whole community and the concept is linked to the sense of being Aboriginal and Torres Strait Islander.
There is a paucity of data on the perceptions, knowledge and attitudes of Aboriginal and Torres Islander families with respect to protective and risk factors for respiratory illness in their children. As stated by Thompson et al. [18], ‘risk factors relating to health outcomes can only be understood in terms of their social meanings and consequences, recognising the important role that social identity, connections, and sense of coherence and control play in the physical configuration of risk’. In a qualitative study undertaken by an Aboriginal social worker of the perceptions of respiratory risk in urban Aboriginal and Torres Strait Islander families and their children [41] families reported key protective factors as heightened parental vigilance, access to support networks, traditional Indigenous culture and values, knowledge about respiratory illnesses, traditional Indigenous medicines, social and emotional wellbeing and exercise. Families reported key risk factors as parental neglect, lack of support networks, poor communication with and lack of trust in medical professionals, stress, loss of traditional culture and values, the external environment, tobacco smoking, hereditary factors and poverty. Parent/carer perceptions of risk and impact of respiratory diseases in their children were influenced by traditional values, connections to family, friends and community, beliefs about both illness and wellness handed down from Elders and family members, experiences within mainstream and Indigenous-specific health services, access to knowledge and information about respiratory diseases, access to reliable support networks and social, emotional and spiritual wellbeing.
Studies undertaken in many countries have identified many risk factors for respiratory illnesses in children, including early life risk factors as predictors of future lung health. These include overcrowding, malnutrition, exposure to tobacco smoke, young maternal age, low birthweight, anaemia, poverty, illiteracy, overcrowding, parental smoking, pollution, socioeconomic status, social behaviours, cultural exposure, family history, and a history of prior illness [42]. While the above factors are highly visible in Aboriginal and Torres Strait Islander communities in both urban and remote settings, little research has been done to specifically examine the effects, interactions and relative importance of these factors with respect to respiratory health.
Prenatal and antenatal factors
The first environment a child is exposed to is the in-utero environment during foetal development; this means that whatever the mother is exposed to has the potential to affect the foetus. Sources of in-utero exposure include maternal disease and maternal exposure to toxins and infectious agents. Maternal asthma has been shown to have adverse developmental effects including low birthweight and intrauterine growth retardation [43]. Maternal exposures (particularly tobacco and infectious organisms) nutrition, stress and the quality of antenatal/postnatal care are important predictors of infant outcomes, including respiratory health.
Exposure to tobacco smoke during pregnancy
Maternal smoking and passive exposure to environmental tobacco smoke during pregnancy is a significant risk factor for respiratory illnesses in the mother, the foetus and the baby [44]. Smoking during pregnancy has also been associated with sudden infant death syndrome, childhood cancers, high blood pressure, asthma, obesity, lowered cognitive development and psychological problems [45]. It can also result in poor health outcomes for the newborn, including low birthweight, intrauterine growth restriction, prematurity, placental complications, birth defects, lung function abnormalities and respiratory symptoms and perinatal mortality [46-48]. The effects of smoking during pregnancy persist into infancy and childhood [49-51]. Maternal smoking is of particular concern as high rates of smoking have been reported for Aboriginal and Torres Strait Islander mothers [52]. In 2015, almost half of Aboriginal and Torres Strait Islander mothers (45%) reported smoking during pregnancy, compared with 12% of non-Indigenous mothers.
Maternal immunisation during pregnancy
Maternal vaccinations can influence acute respiratory illness/infections (ARI) rates. Among infants born during the influenza season, maternal vaccination has been associated with reduced risk of preterm delivery, small-for-gestational age at birth, and foetal death [53], likely due to the prevention of maternal respiratory illness, particularly pneumonia, that has been negatively associated with these birth outcomes [54]. Maternal vaccination in pregnancy may be an effective strategy for protecting infants against influenza prior to six months of age and it is now recommended in several countries including Australia [55, 56]. However, maternal influenza vaccination uptake remains poor and is associated with a number of factors [57]. Demographic factors appear to have little influence on influenza vaccine uptake during pregnancy; however, factors related to antenatal care provision and access (antenatal care type, hospital of delivery and parity) can influence uptake [58]. In a small pilot study of urban Aboriginal and Torres Strait Islander women, 9 out of 53 women had been vaccinated in their pregnancy and only 21 women had been offered the vaccine [58]. Data collected in the study through yarning circles suggested perceived benefits to the women and their infants were important factors in the decision to be vaccinated but that there was insufficient information available to women to make an informed choice [58]. These data differ from a study of Aboriginal mothers in WA where 56/94 (56%) of women received the vaccine during pregnancy; rural mothers were more likely than metropolitan mothers to have been vaccinated (odds ratio (OR) 4.1, 95% confidence interval (CI), 1.7-10.2) [59]. Influenza vaccine coverage during pregnancy in NT Aboriginal women participating in a randomised controlled trial was 16% (35/214), however when comparing periods before and during an influenza pandemic, uptake increased from 2.2% to 41% [60].
Pertussis (whooping cough) is an important respiratory infection in young infants and hospitalisation rates for pertussis in Aboriginal and Torres Strait Islander children are up to three times higher than non-Indigenous children [61]. Pertussis vaccine is recommended in the third trimester of pregnancy to assist in the protection of very young infants before they complete their primary series of pertussis vaccines in the first six months of life. There are limited data on pertussis vaccine uptake in pregnant Aboriginal and Torres Strait Islander women. A study of 93 women in WA [59] reported that 63% had been vaccinated and, as for influenza vaccine, rural women were more likely to have received the vaccine than urban women (OR 3.1, 95% CI, 1.2-7.6). Perinatal data for all women who gave birth in the NT in 2015 identified 24% of Aboriginal and Torres Strait Islander mothers had received a pertussis vaccine during their pregnancy, similar to non-Indigenous mothers (22%) [62].
Air pollution
A major source of foetal environmental exposure is the mother’s external environment; air pollution has been linked to infertility, early pregnancy loss, premature labour and low birthweight [63]. There are some data suggesting social inequity in the distribution of industrial air pollution with Indigenous and other similarly socioeconomically disadvantaged communities disproportionately represented in areas with significant air pollution, including the number of different types, volume and toxicity of emissions [64]. A NT study identified that the effects of ambient air pollution from bushfires on respiratory and cardiovascular illnesses are greater in Indigenous people compared with non-Indigenous people [65].
Maternal nutrition
Evidence from several studies with respect to the relationship between maternal nutrition and dietary behaviours during pregnancy and the development of wheeze, asthma and atopy in offspring is conflicting. A systematic review of 32 studies that assessed vitamins, trace minerals, food groups and dietary patterns during pregnancy [66] found a protective effect of vitamin D, vitamin E and zinc intake against childhood wheeze but results were inconsistent for asthma and other atopic conditions. Maternal Vitamin D concentration in particular is receiving increased interest internationally with several studies suggesting associations with infant health. A meta-analysis of data from 34 observational studies indicated prenatal exposure to Vitamin D was inversely associated with the risk of respiratory infections in childhood (pooled odds ratio (pooled OR) 0.64, 95% CI, 0.47-0.87) [67]. A study of 109 NT Aboriginal and Torres Strait Islander mother-infant pairs [68] reported cord blood concentrations of Vitamin D at birth were about half those in maternal blood during the third trimester of pregnancy (about seven weeks earlier). Cord-blood concentrations of infants hospitalised with acute lower respiratory infection (ALRI) during the first 12 months of life (n = 7) were lower than infants who were not hospitalised (n = 77) (p = 0.025) [68].
Maternal stress
Stress during pregnancy is highly prevalent in Aboriginal and Torres Strait Islander women [69-71]. Maternal stress prior to and during pregnancy has been linked to several health outcomes in offspring [72, 73], including adverse birth outcomes such as prematurity and low birthweight [74], which are recognised risk factors for a number of diseases of childhood, including respiratory illness. The effects are thought to be due to epigenetic influences on gene expression and hence an alteration of disease risk [75]. Further, chronic stress has been linked to immune suppression and an increased susceptibility to infections [76]. Maternal life-time and antenatal stress has been associated with wheezing and asthma [75, 77] and early infection, including respiratory infections, in children [73]. Stress is also a key influence on health behaviours such as smoking during pregnancy, including for Aboriginal and Torres Strait Islander women [78, 79].
Antenatal/postnatal care
As illustrated above, both physical and psychological exposures during and after pregnancy are associated with the risk of respiratory illness in infants and children. The importance of quality antenatal and postnatal care with respect to a broad range of maternal and infant health outcomes is well established. Such care allows the opportunity to screen for and manage a number of problems, as well as undertake health promotion activities and implement strategies to reduce potential or actual identified risks. High quality antenatal care is seen as a right of all women to safeguard their health and that of their infants, providing opportunities for risk factor intervention.
The Australian Government Department of Health recommends 10 antenatal care visits for first-time pregnancy without complications and seven visits for subsequent uncomplicated pregnancies [80]. In 2015, pregnant Aboriginal and Torres Strait Islander women attended an average of nine antenatal visits [52]. Over half (57%) of these women attended the first antenatal visit during the first trimester of pregnancy. In 2014, 99% of Aboriginal and Torres Strait Islander mothers accessed antenatal care services at least once during their pregnancy, similar to non-Indigenous mothers [35]. However, Aboriginal and Torres Strait Islander mothers, on average, accessed services later in the pregnancy and had fewer antenatal care sessions than non-Indigenous mothers.
The child’s home environment
There is a large body of work on home environmental factors that could impact maternal and child health. A recent review on the effects of household air pollution is discussed below [81]. Indoor residential risk factors with links to respiratory health include exposure to dust-mites, cockroaches, pet dander, moisture, mould, combustion of biomass and solid fuels, tobacco smoke, gas and wood stoves, kerosene or gas heaters, mosquito coils, BBQs, candles, overcrowding, and volatile organic compounds that are found in household items such as cleaners, furnishings and paint [81-83]. Many of these are strongly associated with the development of asthma and allergies and increased risk of severe respiratory infections.
Exposure to indoor tobacco smoke is of particular concern in Aboriginal and Torres Strait Islander children. In 2014–2015, 57% of Aboriginal and Torres Strait Islander children aged 0–14 years lived in a household with members who were current daily smokers; 73% in remote areas and 53% in regional and urban areas [84]. For those children living with a daily smoker, 13% were living in households where people smoked indoors. In a study in an urban community, 76% of Aboriginal and Torres Strait Islander children were regularly exposed to environmental tobacco smoke (including indoor, outdoor and in-the-car exposures) [39]. Environmental tobacco smoke exposure in the home increases the incidence of middle-ear disease, asthma, wheeze, cough, phlegm production, bronchitis, bronchiolitis and pneumonia [85].
Crowding may increase the risk of respiratory infection by increasing the opportunity for cross-infection amongst the family. Respiratory pathogens are readily transmitted, usually through air by droplets or aerosols, in crowded and ill-ventilated rooms where people are sneezing and coughing [86, 87]. There have been limited studies that have quantified the link between living conditions and ARI in Aboriginal and Torres Strait Islander children, particularly in urban children. Overcrowding is a well-known concern in Aboriginal and Torres Strait Islander communities and is a result of a complex interplay of social and economic factors. Overcrowding results in a greater intensity of exposure to agents of respiratory disease and facilitates transmission of infectious organisms. In 2014–2015, 16% of Aboriginal and Torres Strait Islander people reported that they were living in overcrowded households compared with 6% of non-Indigenous people [88]. This figure was particularly high for Aboriginal and Torres Strait Islander people living in state owned and managed Indigenous housing, with 23% of people living in an overcrowded household. On a positive note; in 2014-2015, 7% of Aboriginal and Torres Strait Islander adults reported overcrowding as a stressor, down from 21% in 2002 [35]. This change was greatest in very remote areas.
The child’s external physical environment
The external physical environment of the child include factors such as childcare, school attendance, and exposure to industry and air-pollution as well as natural environments that may increase the risk of respiratory illness (e.g. pollen concentrations and dust).
A child’s attendance at a childcare facility can account for an increased frequency and severity of episodes of ARI associated with a broad range of respiratory pathogens [89-92]. Children in childcare are also considered to be important transmitters of pathogens to their siblings, parents, extended families and care workers [91, 93]. There are limited data on the relative importance of childcare to the risk of respiratory diseases in Aboriginal and Torres Strait Islander children although it is likely to play a role given the large body of data associating childcare with respiratory illness. A study of 200 urban children, of whom 90% were Aboriginal and Torres Strait Islander, reported childcare attendance as an independent risk factor for chronic cough (> four weeks duration) following an ARI with cough as a symptom (adjusted relative risk (aRR) 3.56, 95% CI, 1.28 – 9.92). Childcare attendance was not associated with recurrent illnesses [39].
Other external physical environment exposures include particulate matter from industry, motor vehicles, natural sources (e.g. dust storms), diesel exhaust particles, sulphur compounds and ozone. Exposure to particulate matter can have long-term health effects, particularly respiratory diseases, for children [94, 95], with effects starting early in the prenatal period [96]. Post-natal exposure has been associated with childhood chronic cough, wheeze, sore throat, allergy, bronchitis and an increased prevalence of asthma and exacerbations of asthma [94]. There are few studies that have examined physical external environments with respiratory diseases in Aboriginal and Torres Strait Islander children. Many Aboriginal and Torres Strait Islander communities are in areas with high levels of geogenic (i.e. resulting from geological processes) dust particles due to geography, the weather and lack of infrastructure such as sealed roads. There are however, limited studies examining the role of dust in respiratory health in these communities. A WA study indicated that geogenic dust may increase the attachment and invasion of human airway cells by non-typeable Haemophilus influenzae, a bacteria of major importance in human respiratory infections [97].
The child’s social environment
Among Aboriginal and Torres Strait Islander children, important social health factors include household income, the educational and employment status of parents/carers, family structure (i.e. single parent families), school attendance and achievement and the consequences of disadvantage and social disconnectness such as the mental health issues and the misuse of alcohol and illicit substance abuse which are related to an increase in all-cause mortality [98]. Aboriginal and Torres Strait Islander people endure not only the ill health associated with poverty but also the chronic diseases that come with the lifestyle in industrialised countries; a situation that is directly attributable to loss of land and traditions and the resultant move to urban environments. Many remote Aboriginal and Torres Strait Islander communities have schools and health centres available but a disparity still exists in health and education status.
The effects of transgenerational trauma due to loss of culture and identity, especially the effects of the Stolen Generations [99], are now increasingly being recognised as important influences on the determinants and outcomes of poor health in Aboriginal and Torres Strait Islander communities [29, 100-102]. Studies that have formally quantified a relationship between historical factors and respiratory illness are limited. A single centre study of ARI in urban Aboriginal and Torres Strait Islander children aged < five years registered with a primary health care centre reported children with an ARI at time of enrolment were approximately three times more likely to have family members from the Stolen Generation (adjusted odds ratio (aOR) 3.47, 95% CI, 1.33-9.03) or not know family history (aOR 3.35, 95% CI, 1.21-9.26), than those without ARI [103]. Given the limitations of this cross-sectional study, further studies are needed.
Tobacco smoking
As described above, exposure to environmental tobacco smoke and smoking during pregnancy is of major concern with respect to the health of Aboriginal and Torres Strait Islander children. In addition to passive smoking, active smoking, and commencing smoking at an early age is also problematic. Nationally, in 2012–2013, 23% of Aboriginal and Torres Strait Islander youth aged 15-17 years were current daily smokers [104], compared with 4.1% of non-Indigenous youth of the same age. In 2008, the Australian Secondary Students’ Alcohol and Drug (ASSAD) Survey reported approximately 35% of Aboriginal and Torres Strait Islander youth aged 12–15 years old had ever smoked, with 12% smoking in the week before the survey [105]. Smoking prevalence in Aboriginal and Torres Strait Islander people aged 15 years and over are 2.6 times higher than non-Indigenous people [104]. The prevalence is also higher in remote communities than urban settings.
Similarly, cannabis smoking has also been associated with an increased risk of respiratory infections and airway damage [106]. In 2012–2013, 19% of Aboriginal and Torres Strait Islander people aged 15 years and over reported having recently used cannabis [104], with its use considered endemic in some remote Aboriginal and Torres Strait Islander communities [107]. Aboriginal and Torres Strait Islander youth begin using earlier, persist longer, and take greater quantities of cannabis than their non-Indigenous contemporaries [108]. Further, the practice of mixing tobacco with cannabis by Aboriginal and Torres Strait Islander youth, and the resultant coalition of dependencies, has been raised as a particular concern with respect to consequent pulmonary and central nervous system pathology in the future.
Family history
Family history of both malignant and non-malignant respiratory diseases has been shown to be an independent risk factor for a number of respiratory diseases including asthma [109], chronic obstructive pulmonary disease [110] and lung cancer [111], even after accounting for age and tobacco smoke exposure. This suggests a genetic predisposition to disease although the causal pathways are complex and the subject of a large body of ongoing research. Separating genetics from the multi-factorial determinants of respiratory health in Aboriginal and Torres Strait Islander children is problematic, not least because of the concerns about genetics-based research raised by Aboriginal and Torres Strait Islander people [112].
Medical history
The general physical health and wellbeing of infants from birth throughout childhood are important determinants of respiratory health. Pre-existing or co-morbid conditions are important determinants of the development and outcomes of respiratory diseases. Low birthweight and prematurity are well established risk factors as are congenital conditions (e.g. congenital neonatal lung disease), neurological disorders such as Down syndrome and cerebral palsy [113, 114] as well as swallowing disorders such as oropharyngeal dysphagia [115]. Other early childhood infections such as gastroenteritis can predispose children to respiratory infections given impacts on nutritional status and immune function [116], and the role of the gut microbiome in the pathogenesis of respiratory diseases in children is a burgeoning area of research [117]. Gastro-oesophageal reflux and the consequent medications used to treat the disease (e.g. gastric acid inhibitors) have been associated with community-acquired pneumonia in children [118]. There is increasing evidence that particular acute respiratory infections in infancy, particularly respiratory syncytial virus (common cause of bronchiolitis) and rhinovirus, are associated with the development of asthma and bronchiectasis in later years [119, 120], including in Aboriginal and Torres Strait Islander children [121, 122].
Nutrition
Malnutrition is a recognised, important risk factor for respiratory disease in children globally [42]. The nutritional status of a child from birth is a core determinant of the development of a healthy and functional immune system to fight infection and other agents of disease and the ability to deal with and recover from illness. Low birthweight, a factor of maternal nutrition, means the child is disadvantaged from birth and is associated with several adverse health outcomes over the lifespan [123]. Adequate and quality nutrition in the first year of life, particularly via breastfeeding, is a key determinant of infant and child health. Breastfeeding early in infancy is critical to both the transfer of maternal antibodies to protect an infant from infection but also to the delivery of essential nutrients the infant needs to support growth.
A detailed review of the nutritional status of Aboriginal and Torres Strait Islander people, and factors contributing to nutrition such as food security is available [124], and readers are referred to that document for an in-depth presentation of the key data. Of note is that, while for a long period, underweight was a predominant indicator of nutritional status in Aboriginal and Torres Strait Islander children there is now growing evidence that overweight and obesity are becoming problematic [124]. Obesity is a particular problem in chronic lung diseases such as asthma, obstructive sleep apnoea, chronic obstructive pulmonary disease and bronchiectasis [125].
Exercise
The benefits of regular exercise to general health and wellbeing are well known and exercise is also important to respiratory health. Current guidelines recommend that children aged 2–4 years are physically active for at least three hours every day and that children aged 5–17 years do at least 60 minutes per day of moderate to vigorous intensity physical activity [126].
In the 2012–13 AATSIHS, Aboriginal and Torres Strait Islander children aged 2–4 years living in non-remote areas spent an average of 6.6 hours per day participating in physical activity and spent more time outdoors than non-Indigenous children in the same age group (3.5 hours compared with 2.8 hours) [127]. Aboriginal and Torres Strait Islander children aged 5–17 years living in non-remote areas spent an average of two hours per day participating in physical activity (exceeding the recommendation of one hour per day); this was 25 minutes more than non-Indigenous children. Around half (48%) of Aboriginal and Torres Strait Islander children met the recommended amount of physical activity, compared with 35% of non-Indigenous children.
There are limited studies addressing exercise and respiratory health in Aboriginal and Torres Strait Islander children. A qualitative study of Aboriginal and Torres Strait Islander parents/carers of children focussed on the perceptions of risk for respiratory illnesses from an Indigenous perspective [41]. Families considered exercise to be a positive and proactive way of managing respiratory illnesses that the child had control over, and the loss of traditional lifestyles that has led to sedentary behaviours contributed to poor health.
Microorganisms responsible for respiratory infections in children
There are a large number of organisms responsible for respiratory infections in children including bacteria, viruses and fungi. There is also an increasing focus on the role of bacteria-bacteria, bacteria-virus and virus-virus interactions in respiratory infections. It is beyond the scope of this review to discuss these in detail; rather the focus is on the most common bacteria and viruses identified in children.
Despite the burden of respiratory disease in Aboriginal and Torres Strait Islander children, there are surprisingly few contemporary studies that have examined the role of specific organisms in disease; particularly lower respiratory tract infections in the era of pneumococcal conjugate vaccines. This is partly because of the difficulty in obtaining the most appropriate specimens, challenges related to transport and storage of samples from remote areas. Upper airway specimens including nasal swabs and nasal aspirates are often used to identify potential respiratory pathogens. However relating the presence of a particular organism to an illness that is present at the time the specimen is collected is complicated as many of the organisms causing disease are also found in the upper airways of healthy Aboriginal and Torres Strait Islander children [128, 129]. Two small studies that examined nasal specimens from Aboriginal and Torres Strait Islander children in urban [129] and remote areas [130] detected the prevalence of multiple viruses and bacteria and associations with respiratory symptoms [129, 130].
The most common bacteria associated with respiratory infections in children are Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus and Bordetella pertussis. S. pneumoniae, H.influenzae and M. catarrhalis, which prominent in the upper airways of Aboriginal and Torres Strait Islander children in both urban and remote settings with prevalences of > 75% [129-132]. The most common viruses are human rhinoviruses, adenovirus, respiratory syncytial virus, influenza virus and parainfluenza virus [128-130, 133-136] although there are limited data in Aboriginal and Torres Strait Islander children. Aboriginal and Torres Strait Islander infants in remote areas are densely colonised with high loads of bacteria associated with respiratory infections very early in life [137-139], and this is associated with the high rates of otitis media reported in these children [137, 138]. Therefore, early carriage is likely a key factor in the high rates of respiratory infections in Aboriginal and Torres Strait Islander infants. There are very few studies that have longitudinally studied respiratory viruses in Aboriginal and Torres Strait Islander infants, although one WA study reported the median age at the time of virus identification was younger in Aboriginal than non-Aboriginal children [134]. Interventions that address early life infection are important; vaccines are currently only available for S. pneumoniae, B. pertussis and influenza virus.
Extent of respiratory disease among Aboriginal and Torres Strait Islander children
Acute respiratory infections
Acute respiratory infections are illnesses of less than 14 days duration and are classified into either upper respiratory tract infections (URTI) or lower respiratory tract infections (LRTI). URTIs include the common cold, sinusitis, croup, pharyngitis and tonsillitis. LRTIs include pneumonia, bronchitis, croup and bronchiolitis. URTIs often lead to LRTIs and many of the viruses and bacteria associated with ARIs can cause both upper and lower airway infections, for example, influenza virus. URTIs are generally mild and self-limiting while LRTIs are often associated with illnesses of higher severity and longer duration. LRTIs are predominant causes of poor health and death in children worldwide. Recurrent ARIs, particularly early in childhood, are associated with the development of chronic lung diseases [9-11, 51].
Prevalence and incidence
The prevalence of ARI refers to the proportion of children in a population who have an ARI at any particular point in time. There are few data on the prevalence of ARI and respiratory symptoms in Aboriginal and Torres Strait Islander children. In an urban single centre study [103], 33% of children (n = 180) presenting to a primary health care centre for any reason (including accompanying someone else) had symptoms of an ARI however, only 22% of children specifically presented to the centre for that illness [103]. A cross-sectional study of 651 children from remote communities in the NT reported that, at the time of assessment, 59% of children had a runny nose and 39% had a cough [132].
The incidence of ARI refers to the number of new cases of ARI that occur during a given time. Despite the importance of ARI and ARI outcomes, there are surprisingly few comprehensive studies that have examined ARI incidence at the community level in Aboriginal and Torres Strait Islander children. A recent study of urban children (90% Aboriginal and Torres Strait Islander), registered with a single primary health care provider, reported an incidence of ARI with cough as a symptom, of 25 episodes per 100 child-months at risk (95% CI, 22.3-27.5). This likely underestimates all ARI incidence as the study focussed on episodes with cough. In five remote communities in the NT, children had a median of three (interquartile range (IQR) 2-5) presentations to the clinic over a 12-month period for LRTI and six (IQR 3–10) presentations for URTI, respiratory illnesses [140].
Health service utilisation
The characteristics of patients presenting to different health services in Australia will vary and be influenced by socioeconomic and population demographics. Understanding the characteristics of Aboriginal and Torres Strait Islander communities in the primary health care context is important as it is essential to closing the health gap for Aboriginal and Torres Strait Islander people [141, 142]. The lack of contemporary, prospectively collected health service utilisation data in urban and remote Aboriginal and Torres Strait Islander children limits the ability to evaluate change over time and assess whether initiatives to improve access are working. Further, the Aboriginal and Torres Strait Islander population within and between Australian settings is not homogenous and composite statistics that are available are unlikely to reflect this diversity and identify groups that may be at risk of being lost within the system.
General practice and primary health care utilisation
There are scarce data on general practice attendances for ARI in Aboriginal and Torres Strait Islander children. While many of the differences between Aboriginal and Torres Strait Islander and non-Indigenous health outcomes can be attributed to social determinants, it is known that the accessibility of good primary health care is important to both the prevention and management of disease [143].
Utilisation of primary health care services that are culturally appropriate is important as the determinants of good health and health behaviours are broader than socioeconomic issues. These determinants include history, the quality and quantity of relationships and connection to culture [27]. There is evidence to suggest that Aboriginal and Torres Strait Islander people are less likely to access health services and encounter more barriers in the use of health services [144, 145]. This leads to delays in diagnosis and treatment or lack of exposure to health education and promotion programs.
Data from a decade of surveys of general practitioner (GP) activity suggests that 1.2% of patients visiting GPs identified as being of Aboriginal and Torres Strait Islander origin [146]. In 2015–2016, among 97,328 total GP encounters reported in the Bettering the Evaluation and Care of Health (BEACH study), the rate of encounters for Aboriginal and Torres Strait Islander people was 1.5 per 100 (95% CI, 1.2-1.8) [147]; data specific to Aboriginal and Torres Strait Islander children were not presented. Aboriginal and Torres Strait Islander people have higher rates of long or complex consultations, higher rates for management of diabetes, infections, asthma and drug use, lower rates of management for cardiovascular disease and hypertension, and lower rates of preventative health care services such as immunisations and cardiac check-ups [148]. In 2014–15, a GP or doctor was the most common health service utilised for Aboriginal and Torres Strait Islander children aged < 15 years (58% of services utilised), followed by an Aboriginal medical health service (25% of contacts) [6].
Nationally, little is known about the differences in primary health care service utilisation between Aboriginal and Torres Strait Islander and non-Aboriginal and Torres Strait Islander children [38, 149, 150]. Ou et al. [149][1] , analysed data collected in 2004 from children aged < 12 months in the Longitudinal Study for Australian Children. They found the proportion of Aboriginal and Torres Strait Islander infants in the first 12 months of life accessing a health service was lower than non-Indigenous infants (2.5% compared with 3.1%). For Aboriginal and Torres Strait Islander infants, maternal and child health services were less likely to be utilised (68% compared with 83% respectively). However, a higher proportion of Aboriginal and Torres Strait Islander infants presented to hospital outpatient clinics (16% compared with 9.7% respectively) and a higher proportion were hospitalised (17% compared with 9.9% respectively).
Clucas et al. [151] retrospectively reviewed clinic records in two remote NT primary health care clinics. They reported children presented to the community clinics an average of two times per month in the first 12 months of life. Kearns et al. [140] conducted a retrospective review of clinic presentations of 320 children living in five remote Aboriginal communities in the NT. The median number of presentations per child for any cause in the first year of life was 21 (IQR 15-29). The most common infectious presentations per child were URTI (median 6, IQR 3-10); diarrhoea (median 3, IQR 1-5); ear disease (median 3, IQR 1-5); LRTI (median 3, IQR 2-5); scabies (median 3, IQR 1-5); and skin sores (median 3, IQR 2-5).
A prospective cohort study in first-born non-Indigenous infants by Goldfeld et al. [152] conducted in two middle socioeconomic urban areas of Melbourne found that, in the first 12 months of life, children had approximately 35 health service visits (average of 2.9 per month), with 31% being visits to GPs and 42% to maternal and child health nurses. Hall et al described health service utilisation amongst a cohort of 180 urban Aboriginal and Torres Strait Islander children in South East Qld registered with a primary care service [153]. The overall incidence of health service utilisation was 52 episodes per 100 child-months (95% CI, 48.7-56.5); 81% of encounters were with GPs. Presentation rates were the highest for ARI (31 episodes per 100 child-months, 95% CI, 27.8-33.9). The next most common source of care was hospital emergency departments [153].
Hospitalisation
National and state hospitalisation rates for ARI for Aboriginal and Torres Strait Islander children are difficult to interpret given most published data reports hospitalisations for respiratory diseases overall and hence include chronic illnesses such as asthma. Further, the majority of reports of ALRI hospitalisations are based on one or more combinations of International Classification of Diseases or (ICD) codes for pneumonia and influenza, with specific causative organisms for the former infrequently reported.
For July 2013 to June 2015 respiratory disease hospitalisation rates for Aboriginal and Torres Strait Islander children aged 0–4 years were 78 per 1,000 population compared with 48 per 1,000 population for non-Indigenous children [35]. The corresponding rates for children aged 5–14 years were the same for Aboriginal and Torres Strait Islander and non-Indigenous children, 12 per 1,000. The respiratory disease hospitalisation rate for Aboriginal and Torres Strait Islander males 0–4 years was 90 per 1,000 compared with 57 per 1,000 for non-Indigenous males. For Aboriginal and Torres Strait Islander females 0–4 years, the rate was 65 per 1,000 compared with 38 per 1,000 for non-Indigenous females. For Aboriginal and Torres Strait Islander and non-Indigenous males 5–14 years the rates were both 13 per 1,000. For Aboriginal and Torres Strait Islander females and non-Indigenous females 5–14 years the rates were both 12 per 1,000.
Aboriginal and Torres Strait Islander children have higher rates of hospitalisation for ARI than non-Aboriginal and Torres Strait Islander people regardless of their geographical location [154]. In WA, hospital admission rates per 1,000 live births (infants born between 1990 and 2000) for ALRI before age two years were 7.5 (95% CI, 7.2-7.7) times higher in Aboriginal than non-Indigenous children (337 compared with 45 per 1,000 live births); pneumonia rates were 13.5 (95% CI, 12.8-14.4) times higher and bronchiolitis rates were 5.8 (95% CI, 5.3-6.0) times higher [155]. However, over that time, ALRI hospitalisation rates declined in Aboriginal children aged 12-23 months (4% per year, P = 0.003) predominantly reflecting a decline in pneumonia rates [155]. Between 1997 and 2005, the rates of hospitalised, radiologically diagnosed pneumonia in Central Australian Aboriginal children aged < five years were 27 per 1,000 population per year (95% CI, 25.3-27.9); 58 per 1,000 per year in infants aged 1–11 months, 38 per 1,000 per year in those aged 12–23 months, and 13 per 1,000 per year in those aged 24–59 months [156]. Rates in Central Australian children were twice that of Top End children and were amongst the highest reported worldwide. For NT infants aged < 12 months born between 1999 and 2004, ALRI hospitalisation rates were 427 episodes per 1,000 child-years (95% CI, 416.2-437.2) and the median age at first admission for an ALRI was 4.6 months (IQR 2.6-7.3). Between 2007 and 2011, hospitalisation rates for children aged < 15 years admitted to the Mt Isa Base Hospital were almost five times higher among Aboriginal and Torres Strait Islander children compared with non-Indigenous children (24 compared with 4.5 per 1,000 population per year) [157]. In an urban Aboriginal and Torres Strait Islander cohort of children aged < five years, the hospitalisation rate for an ARI with cough was 1.5 per 100 child-months of observation [39].
National influenza hospitalisation rates for the period 2005–2010 were 2.9 times higher for Aboriginal and Torres Strait Islander children aged < five years than non-Indigenous children (2.1 per 1,000 compared with 0.7 per 1,000 population per year) and 2.6 times higher for children aged 5 – < 15 years (0.4 per 1,000 compared with 0.2 per 1,000 population per year) [61]. The data however, included influenza diagnoses in which no influenza virus was identified. Hospitalisation rates for pertussis (whooping cough) over the same period were 3.3 times higher in Aboriginal and Torres Strait Islander children aged < five years than non-Indigenous children (0.9 compared with 0.3 per 1,000 population per year) and 1.8 times higher for those aged 5 – < 15 years (0.02 per 1,000 compared with 0.01 per 1,000 population per year).
Bronchiolitis is a predominant cause of hospitalisation in young children worldwide, including Aboriginal and Torres Strait Islander children [156, 158]. There are some data suggesting the rates are rising [158]. Aboriginal and Torres Strait Islander children with bronchiolitis have more severe disease and higher rates of re-admission than non-Indigenous children [159]. The persistence of symptoms following hospitalisation for bronchiolitis was associated with an increased risk of the development of bronchiectasis in the 24 months following discharge in Aboriginal infants in the NT (OR 3.0, 95% CI, 1.1-7.0, P = 0.03) [122]. Between 2007 and 2011, the average annual bronchiolitis hospitalisation rate to Mt Isa Base Hospital for Aboriginal and Torres Strait Islander children was 71 per 1,000, compared with 15 per 1,000 for non-Indigenous children [157]. In the NT for Aboriginal infants born between 1999 and 2004, the incidence of bronchiolitis hospitalisations was 227 per 1,000 child-years in the first year of life [156]. In WA, Aboriginal children born between 1990 and 2000 were approximately 5.8 times (95% CI) more likely to be hospitalised with bronchiolitis in the first two years of life than non-Indigenous children [158]. More recent data on Aboriginal and Torres Strait Islander children are lacking nationally.
Other health service providers
There are insufficient data on the utilisation of other health service providers beyond hospitalisations and GPs for Aboriginal and Torres Strait Islander children with ARI. In 2015–16, around 6% of emergency department (ED) presentations (462,000) were reported for Aboriginal and Torres Strait Islander people (excludes the ACT) [35] however, data specific to children were not reported. Duncan et al. [160], conducted a review of ED presentations by Aboriginal and Torres Strait Islander children to Sydney Children’s Hospital between 2005 and 2008; 1,252 presentations were made by 435 children aged 0-15 years. The majority of presentations were for children aged < one year of age and 30% of presentations were for respiratory illnesses. The review found that nearly 45% of presentations were potentially preventable and could have been referred to allied health services or to a GP.
A retrospective population-based study conducted by Moore et al. [155], used the Western Australia Data Linkage System (WADLS) of live singleton births followed up to nine years of age in WA to examine ED presentations for ALRI. ALRI accounted for 53% of all presentations. Of Aboriginal children, 14% presented at least once to ED before age five years compared with 6.5% of non-Aboriginal children. Aboriginal and Torres Strait Islander children born in an urban area had a higher proportion of ED presentations for ARI (15%) compared with urban born non-Aboriginal and Torres Strait islander children (7.2%).
In the South East Qld urban cohort of Aboriginal and Torres Strait Islander children aged < five years [153], presentation rates to EDs for any cause were 1.6 per 100 child-months (95% CI, 1.0 – 2.4) of observation; ARI presentations were 1.4 per 100 child-months (95% CI, 0.8 – 2.1). Overall, presentation rates to ‘other’ services for ARI (including pharmacies, maternal and child health nurses, natural therapists and traditional healers) were 2.8 episodes per 100 child months (95% CI, 2.0 – 3.8).
Non-fatal disease burden
Non-fatal disease burden refers to years lived with ill health or disability and is a measure of the relative importance and impact of disease, that does not result in death, to the health and wellbeing of a population. It is commonly combined with years of life lost due to premature death from a disease (fatal disease burden) to produce a measure known as a disability-adjusted life year which counts the total years of healthy life lost from disease and injury [3]. In 2011, upper respiratory conditions were the 8th leading cause of non-fatal disease burden in Aboriginal and Torres Strait Islander males and females aged < five years and for those aged 5 – < 15 years, the 10th leading cause in males and 7th leading cause in females. Lower respiratory infections ranked 9th and 10th for males and females aged < five years respectively and were not in the top 10 for those aged 5 – 14 years. Caution is required in interpreting these data as acute respiratory illnesses and upper respiratory diseases can include chronic conditions such as chronic sinusitis and lower respiratory infections can include chronic infections associated with chronic lung diseases.
Mortality and fatal disease burden
Data on deaths due to ARI in Aboriginal and Torres Strait Islander children are scarce as most reports use the composite category of ‘respiratory illness/disease’, and mortality due to ARI in these children has been declining over recent decades and is now rare [3, 35], likely a result of improved and early diagnosis and management. In a national report for the period 2006–2010 there were no deaths due to influenza as the underlying cause in children aged < five years [61]; deaths in older children were not reported separately to adults, nor were deaths due to pneumonia reported. As mortality due to ARI in Aboriginal and Torres Strait Islander children is rare, those illnesses do not contribute significantly to fatal disease burden (i.e. years of life lost) [3].
Total disease burden
In 2011, lower respiratory tract infections were the 8th leading cause of disability adjusted life years in Aboriginal and Torres Strait Islander females aged < five years (3.1% of total disease burden) and upper respiratory conditions were the 10th leading cause in females aged 5 – < 15 years (2.6% of total disease burden) [3]. Neither conditions were in the top ten conditions contributing to total disease burden for Aboriginal and Torres Strait Islander males in either age group. The reasons for this discrepancy by gender are not clear.
Chronic respiratory diseases
Chronic respiratory diseases of importance in Aboriginal and Torres Strait Islander children include recurrent protracted bacterial bronchitis (PBB), chronic suppurative lung disease (CSLD), bronchiectasis, particularly non-cystic fibrosis bronchiectasis and asthma. Recurrent PBB, CSLD and bronchiectasis are thought to exist on a spectrum of disease characterised by chronic lower airway infection and inflammation [161]. PBB is characterised by a chronic wet or productive cough without signs of an alternative cause and responds to two weeks of appropriate antibiotics [162]. Recurrent episodes occur [163] and this is thought to lead to chronic suppurative lung disease and bronchiectasis [163]. CSLD is characterised by recurrent episodes of prolonged wet cough and may be accompanied by other problems such as recurrent chest infections, difficulty breathing on exertion, growth failure and, occasionally, wheeze [164]. Bronchiectasis is clinically similar to CSLD however and is diagnosed on the basis of high-resolution computed tomography (HR-CT) which reflects dilatation (widening) of the peripheral airways [161]. Bronchiectasis is a major concern in Indigenous children in Australia, Alaska and New Zealand with common risk factors amongst the three populations [165], particularly premature birth and frequent/severe respiratory infections in early childhood. Asthma is defined by the presence of both excessive variation in lung function and respiratory symptoms (e.g. wheeze, shortness of breath, cough and chest tightness) that vary over time [166].
Mortality and morbidity from chronic respiratory diseases are greater for Aboriginal and Torres Strait Islander people than for non-Indigenous people [3]. Falling mortality rates [167] in the context of increasing hospitalisation and self-report of disease may reflect better diagnosis and disease management. However, the possibility of increasing disease prevalence cannot be discounted in the absence of comprehensive community based data.
Prevalence and incidence
Despite the burden of chronic respiratory infections in Aboriginal and Torres Strait Islander children with respect to hospitalisations, there is a paucity of data on the prevalence of disease, largely reflecting a widespread lack of research that covers different regions of Australia. The incidence of chronic respiratory diseases in Aboriginal and Torres Strait Islander children is largely unknown outside a very small number of studies in selected regions of the country. There are no data on the incidence or prevalence of CSLD or recurrent PBB in Aboriginal and Torres Strait Islander children. As recurrent PBB and CSLD are likely precursors to bronchiectasis, the prevalence of those diseases are likely to be much higher than bronchiectasis.
Bronchiectasis
There is only one study to date that has estimated the prevalence of bronchiectasis in Aboriginal and Torres Strait Islander children. This study of Central Australian children reported a prevalence of approximately 15 per 1,000 children [168]. The only data on bronchiectasis incidence in Aboriginal and Torres Strait Islander children are from studies that reflect those predominantly living in remote areas. In the early 2000s, the average annual incidence of bronchiectasis among children living in Central Australia was 735 per 100,000 population [169]. In a population based study of ALRI hospitalisations in Aboriginal and Torres Strait Islander infants born between January 1999 and December 2004, the incidence of first diagnosis for bronchiectasis in the first year of life was 1.2 per 1,000 child-years (95% CI, 0.60-2.16) [156, 170]. In a prospective study of 157 Aboriginal and Torres Strait Islander infants hospitalised for bronchiolitis (median age at admission was five months), 30 (19%) were subsequently diagnosed with bronchiectasis within 24 months of admission [171].
A national bronchiectasis register has been established and this is likely to improve estimates of bronchiectasis burden in the coming years [172].
Asthma
There are uncertainties around the accuracy of prevalence data for asthma in children as other chronic respiratory diseases are commonly misdiagnosed as asthma [173]. In 2012–2013, approximately 15% of Aboriginal and Torres Islander children aged < 15 years were reported as having asthma, compared with 9.3% of non-Indigenous children [104]. Asthma prevalence is higher in Aboriginal and Torres Strait Islander children in urban and regional areas compared with those in remote areas. A north Qld study extrapolated data from children presenting to a paediatric outreach service (n = 3,562) between 2001 and 2006 [174] to the census population of the relevant communities and estimated the prevalence of asthma in Aboriginal children to be 32 cases per 1,000 Aboriginal children and 20 cases per 1,000 Torres Strait Islander children. A number of limitations with the study are the likely explanation for the lower prevalence reported in national studies. Overall, national data suggest the prevalence of asthma in the Aboriginal and Torres Strait Islander population has reportedly not changed since 2001 [104].
There are no data on the incidence of asthma in Aboriginal and Torres Strait Islander children, possibly in part due to the difficulties in accurately diagnosing asthma in young children with symptoms of cough and wheeze [175]. A small study of 47 Aboriginal children admitted to Royal Darwin hospital evaluated the accuracy of reporting of cough by their carers [176]. It compared carer report to a 24-hour digital recording of the child’s cough and found carer report to be unreliable, highlighting the need for community education.
Health service utilisation
General practice attendances
There are no data on general practice attendances for PBB, CSLD and bronchiectasis in Aboriginal and Torres Strait Islander children. Similarly, data are lacking on GP use by Aboriginal and Torres Strait Islander children for asthma. A randomised controlled trial of an asthma education intervention for 88 Torres Strait Islander children with asthma [177], with unscheduled asthma presentations i.e. hospitalisations or GP attendances for asthma exacerbations over a 12 month period as the primary endpoint, reported 44% of children in the control group (n = 53) had at least one presentation with 4% having three or more presentations. There were no differences in presentation rates between the intervention and control groups.
Hospitalisation
Protracted bacterial bronchitis, chronic suppurative lung disease and bronchiectasis
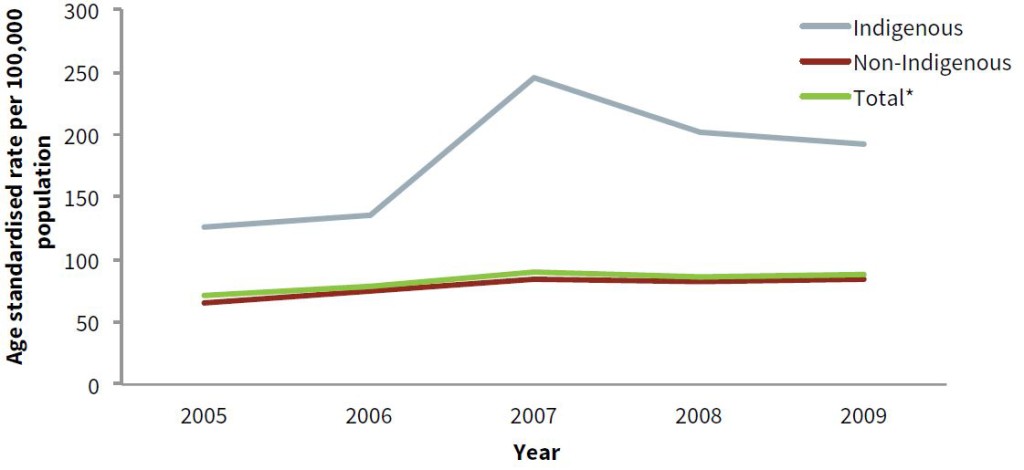
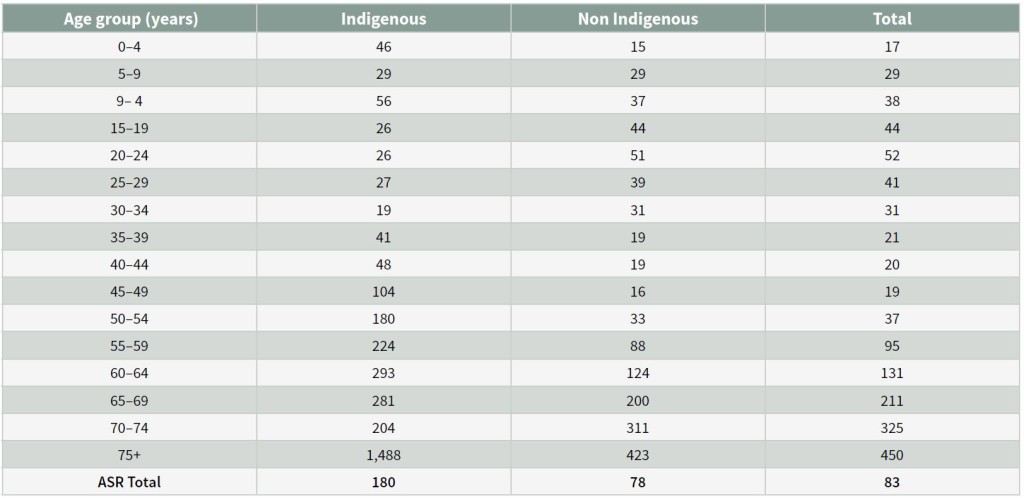
There are no published data on PBB and CSLD hospitalisation rates in Aboriginal and Torres Strait Islander children, and limited data on bronchiectasis hospitalisations. The accuracy of currently available paediatric hospitalisation data is questionable given there is some evidence that paediatric bronchiectasis was being coded as chronic obstructive pulmonary disease given the lack of a diagnosis related group (DRG) code for bronchiectasis [178]. This limitation will change in July 2018 when a new DRG for bronchiectasis comes into effect (Goyal V, personal communication, March 2018). O’Grady et al., analysed age-standardised hospitalisation rates for bronchiectasis in Qld for the period 2005–2009. Over that period, bronchiectasis hospitalisation rates increased in all age groups and in all years (Figure 2) and rates were, on average, two times higher for Aboriginal and Torres Strait Islanders than non-Aboriginal and Torres Strait Islanders. In children aged 0–4 years, average annual rates were 46 per 100,000 for Aboriginal and Torres Strait Islander children compared with 15 per 100,000 for non-Indigenous children (Table 1). Data were not presented by urban versus remote residence. A retrospective chart review conducted during 2007–2011 at the Mount Isa Base Hospital in Qld, reported an average annual bronchiectasis hospitalisation rate of 410 per 100,000 in children < two years of age [157].
Figure 2: Age-standardised hospitalisation rates per 100,000 population for bronchiectasis, by year and Indigenous status, Queensland, 2005–2009
Notes: 1. Includes 690 episodes in which Indigenous status was not stated
- Directly standardised to the 2007 Australian Estimated Resident Population.
Source: O’Grady KF, Revell A, Maguire G, Millonig R, Newman M, Reid D, Hill DC, Chang AB, 2010 [178].
Table 1: Bronchiectasis average annual age-standardised hospitalisation rates per 100,000 population by Indigenous status, Queensland, 2005–2009
Note: Directly standardised to the 2007 Australian Estimated Resident Population.
Source: O’Grady KF, Revell A, Maguire G, Millonig R, Newman M, Reid D, Hill DC, Chang AB, 2010 [178].
Asthma
There are limited reliable and specific data on asthma hospitalisations in Aboriginal and Torres Strait Islander children, including trends over time, and the data that are available are largely limited to national composites. In 2014–2015, asthma hospitalisation rates for Aboriginal and Torres Strait Islander children aged 0–14 years were 4.3 per 1,000 population compared with 4.5 per 1,000 for non-Indigenous children [6]. Rates for Aboriginal and Torres Strait Islander youth/young adults aged 15–24 years were 1.2 per 1,000 population compared with 0.8 per 1,000 for non-Indigenous youth/young adults.
Non-fatal disease burden
Data on chronic respiratory disease non-fatal burden (i.e. years of life with disability (YLD)) in Aboriginal and Torres Strait Islander children are only available for asthma. In 2011, asthma ranked as the 3rd leading cause of YLD in male and female children aged < five years and 2nd for children aged 5 – < 14 years [3]. For males aged < five years, asthma accounted for 15% of total YLD and 13% of total YLD for those aged 5 – < 15 years. The corresponding proportions for females were 8.1% and 13%.
Mortality and fatal disease burden
As with ARI, there are limited data specifically reporting mortality due to chronic respiratory diseases in Aboriginal and Torres Strait Islander children. In The Australian Burden of Disease Study, focusing on the disease burden of Aboriginal and Torres Strait Islander people in 2011 [3], respiratory diseases were not in the top five contributors to fatal disease burden (i.e. years of life lost) in children.
Total disease burden
In 2011, asthma ranked as the 8th leading contributor to total disease burden in Aboriginal and Torres Strait Islander males aged < five years (3.6% of total burden) and 2nd in males aged 5 – < 15 years (10% of total burden) [3]. For females, asthma was not in the top ten contributors to total disease burden for those aged < five years but was leading contributor in those aged 5 – < 15 years (10% of total disease burden). The total disease burden of other chronic respiratory diseases in children was not reported in the top ten.
Prevention and management
As expressed previously, a focus on both children’s lung and general health is required to reduce the burden of chronic respiratory illness in later life and in adulthood. However, a systematic overview of interventions addressing the social determinants of health found a striking lack of reliable evaluations of the various potential interventions [179]. Where evidence was available, the health improvement associated with interventions was modest or uncertain.
Prevention
The prevention of respiratory illnesses in Aboriginal and Torres Strait Islander children, or at the very least a closure of the gap in disease burden between them and their non-Indigenous contemporaries, will be largely dependent on ongoing changes in socioeconomic disparities and a reduction in modifiable risk factors. Preventing recurrent ARIs and addressing risk factors early in life is likely to translate to long-term health benefits, particularly the prevention of chronic lung disease. In this section, we do not differentiate between prevention of acute and chronic illnesses as the important determinants of disease are largely the same. Further, whilst socioeconomic change is critical, it will take time and a focus on more readily modifiable risk factors is necessary [180, 181].
The critical factors to address are maternal health and wellbeing (before, during and after pregnancy) to improve neonatal and infant outcomes from birth, infant and child nutrition, reductions in exposure to environmental tobacco smoke and other pollutants, prevention of the uptake of smoking in youth, timely provision of recommended vaccines during pregnancy, infancy and early childhood (particularly influenza, pertussis and pneumococcal vaccines) and the education and empowerment of parents/carers to recognise abnormal respiratory signs and symptoms and to seek timely care. Enabling parents/carers to feel confident in seeking care and discussing their concerns with health care providers is important given data suggesting some families feel they are not taken seriously by their provider [41]. The prevention of chronic respiratory infections can be facilitated by adequate follow-up following illness, particularly following lower respiratory infections such as pneumonia and bronchiolitis and when illness progresses to chronic cough (> four weeks duration) [181]. Further, educating parents on the importance of seeking care for persistent symptoms and completing courses of prescribed medications, including antibiotics, is important. There are scarce data on parent/carer knowledge of cough and medication use for ARI. In an urban study of Aboriginal and Torres Strait Islander children [39], 95% of parents (n = 180) were aware that persistent and wet cough was abnormal, however 13% incorrectly reported antibiotics should only be taken until there were no more symptoms present suggesting more education is required.
Management
In managing illnesses among Aboriginal and Torres Strait Islander people, the commonly encountered paradigm of a defeatist approach of ‘minimal treatment’ needs to be changed to a ‘best possible care of intensive and appropriate treatment’. The major improvement in longevity of people with cystic fibrosis over the last three decades is not related to major technological or genetic breakthroughs, but related to improved clinical care through better attention to nutrition, airway clearance and intensive treatment of infections. If Aboriginal and Torres Strait Islander children receive optimal treatment (including a system-wide approach that includes multi-disciplinary, evidence-based, culturally appropriate, management pathways), the clinical outcomes should be similar to their non-Indigenous counterparts. Readers are referred to specific management guidelines for individual conditions.
Early detection
There are no specific respiratory risk assessment tools for Aboriginal and Torres Strait Islander children that have been developed and evaluated. However, there are many symptoms suggestive of chronic lung disease. In children, the most common is cough. Indeed, chronic cough is one of the earliest symptoms of airway disease and may reflect an underlying serious disorder [173]. It is also one of the most common symptoms presenting to respiratory (lung) specialists. Delayed diagnosis of an underlying disorder may cause further chronic morbidity [173], while early diagnosis leads to appropriate management and subsequent resolution of cough and improved quality of life (QoL) [173, 182]. In a national multicentre study, 18% of the 346 children newly referred for chronic cough had a serious underlying diagnosis (bronchiectasis, aspiration, cystic fibrosis) and 41% (n = 142) of children had PBB, a likely pre-bronchiectasis condition [162] in children at high risk of CSLD. The 31 (9%) children who had bronchiectasis were significantly more likely to be Indigenous than non-Indigenous (OR = 4.4, 95% CI, 1.9, 10) [173]. Importantly, 70% of the cohort were misdiagnosed as asthma [173]. In another study where children who presented to the ED were recruited, a new and serious chronic lung disease was diagnosed in 36 of the 117 (31%) followed-up for their persistent cough on day 28 [183]. Therefore, management of chronic cough is paramount to early diagnosis of an underlying lung disorder. Obtaining the correct diagnosis also reduces the morbidity from incorrect medications used.
Primary health care setting
Use of appropriate cough pathways or algorithms is one strategy that leads to earlier diagnosis of underlying chronic illness and reduce the morbidity of chronic cough and unnecessary costs. In a multi-centre randomised controlled trial based in referral centres [182], it was found that use of a cough management pathway embedded within a guideline improved clinical outcomes (improved QoL and reduced the duration of cough i.e. earlier diagnosis and management of the aetiology of the cough). A systematic review [184] and an expert panel report [185] found high quality evidence that the use of cough management protocols improves clinical outcomes in children with chronic cough (> four week duration).
The presence of chronic wet cough in children implies lower airway infection and intense inflammation, as seen in PBB [164, 186]. In an NT-based follow-up study, Indigenous children with persistent wet cough (n = 30) after an acute hospitalisation for an ALRI were significantly more likely to have bronchiectasis compared with those without a cough (n = 126), (OR = 3, 95% CI, 1.1, 7, p = 0.03) [122]. Treatment of the endobronchial infection present in these children with chronic wet cough [185] would likely halt the ongoing infection and inflammation and prevent CSLD [187]. In children from a population at risk of chronic lung disease, a model of care that follows up (and treats when required) children post-hospitalisation for a lung illness could prevent development of CSLD.
Models of care
Established models to support and enhance lung health care ideally encompasses:
- One-to-one health education for adult caregivers of children with an acute (as they are at risk of chronic lung disease) or a chronic lung illness, using culturally appropriate tools.
- Follow-up of the child in the clinic at least 3–4 weeks post lung hospitalisation to determine resolution of all lung symptoms and signs. Earlier studies found that very few children were followed up post hospitalisation yet approximately 25% had persistent lung symptoms. Those with persistent wet cough after hospitalisation were significantly more likely to have bronchiectasis compared with those without a cough, (OR=3, 95% CI, 1-7, p = 0.03) [122]. Ideally a systems approach is required whereby all children are recalled back to the local clinic for a review 3–4 weeks post-hospitalisation and post-medical presentation for any ARI.
- Inclusion of an Indigenous health or community worker/health aide around the discharge process (pre or post) and health education [177, 188, 189]. This model is supported by evidence from a Cochrane review [190]. In a randomised controlled trial in the Torres Strait region of an asthma education model that included an Indigenous health worker, improvements were seen in some important asthma outcomes (e.g. missed school days due to wheezing, parent knowledge) in those randomised to the intervention compared with controls [177]. The improved outcomes included children missed fewer school days due to wheezing, improvement of carers knowledge of asthma medication. In the exploration of the benefits of the model [191], common themes were expressed by community members. The most important themes were around ‘service delivery quality’ and ‘clear transfer of knowledge and education/clinical knowledge of asthma’. The parents/carer responses strongly valued the high level of communication, professional approach and rapport. Parents/carers also indicated their appreciation of access to a specialist in the community, the interaction experienced with the health professionals was positive and their sense of empowerment evident by learning how to manage their child’s asthma.
Working in partnership with the local community
In chronic diseases, individualised and multi-disciplinary case management operating within an inter-professional framework is optimal [192]. One of the recommendations in the bronchiectasis guidelines (pp. 23), [161] states ‘Coordination of care among health care providers is necessary’. Specialist evaluation is recommended if bronchiectasis is suspected to confirm diagnosis, investigate aetiology, assess baseline severity and to develop management plans [193]. Those with moderate or severe disease are best managed using a multi-disciplinary approach to chronic care with individualised case management. Clinical deterioration should prompt early referral to services with CSLD/bronchiectasis expertise.
Aboriginal and Torres Strait Islander specific resources for lung conditions
Health education is a key component in improving clinical outcomes [194] but there are limited data on the best method of providing health education. Different settings likely require different approaches, championed locally and undertaken in conjunction with local Aboriginal and Torres Strait Islander partners. An assessment of resources for lung health for Aboriginal and Torres Strait Islander Queenslanders [195] and a qualitative study of parent/carer perceptions of respiratory illnesses in Aboriginal and Torres Strait Islander children [41] both identified the lack of appropriate educational resources as important barriers to the prevention and management of disease. A lack of education and accessible information was also identified as a contributor to maternal uptake of influenza vaccine in Aboriginal and Torres Strait Islander women [58]. One NT-based study found that carers of Indigenous children hospitalised with common serious respiratory illness had low knowledge of respiratory conditions and that using culturally appropriate educational flipcharts improves the knowledge of these respiratory conditions [196]. These resources are available at the Australian Indigenous HealthInfoNet web site (http://aih-wp.local) and have also morphed to adult-specific Aboriginal and Torres Strait Islander resources available on the Menzies School of Health Research website (https://www.menzies.edu.au/page/Resources). Lung-specific education is important in the remote Aboriginal and Torres Strait Islander setting as cough is under reported by Aboriginal and Torres Strait Islander carers of children hospitalised for a lung illness [176]. While flipcharts are well-received educational resources in Aboriginal and Torres Strait islander health, it is likely that, but remains unknown if, interactive app-based resources lead to better health education specific for Aboriginal and Torres Strait Islander people.
Programs and services
Generically, as most Aboriginal and Torres Strait Islander people prefer using culturally specific services such as Aboriginal community controlled health organisations, it is assumed that people with lung conditions also prefer accessing those services however there are no specific data available to support the assumption. As found in Qld however [195], the specific services and resources available for Aboriginal and Torres Strait Islander people with lung diseases are limited and those that do exist are, with the exception of asthma, largely directed at adults with chronic lung diseases.
Government-based programs and services
A Qld state-based review of lung health and service provision highlighted the lack of data on disease and the limited available services for Aboriginal and Torres Strait Islander Queenslanders [178]. Subsequently, in Qld, a specific Indigenous Respiratory Outreach Care program funded by the Aboriginal and Torres Strait Islander Unit of Queensland Health through Federal funds started in 2011 [197]. In this program, teams are dedicated to each area of service with individualised plans (including educational and community activities) developed in conjunction with the local area services. The program provides dedicated paediatric and adult teams. A quarterly specialist paediatric respiratory clinic also operates in one Aboriginal Medical Service in WA however, whether other similar services operate elsewhere is unknown.
There is a specific spacer program for use with asthma medications for Aboriginal and Torres Strait Islander Australians [198]. Other government programs that Aboriginal and Torres Strait Islander people may benefit from are generally generic rather than specific for lung conditions. This includes Aboriginal and Torres Strait Islander specific Medical Benefits Schedule (MBS) items for check-ups (715 health check) and the Pharmaceutical Benefit Scheme’s ‘close the gap’ initiative which provides medications at a reduced cost. The aim of the 715 health check is to ensure Aboriginal and Torres Strait Islander people receive appropriate primary health care that includes early detection, diagnosis and intervention for common and treatable conditions [199]. Arguably, this program is far too superficial for lung health as it does not include any specific measurement such as spirometry and recent data suggests the uptake of the health checks is poor [35]; in 2015–16, assessments were undertaken for only 26% of the paediatric target group (i.e. children aged 0–14 years). Only 33% of children aged 0–4 years who were regular clients of Commonwealth-funded Aboriginal and Torres Strait Islander primary health care organisations had received an assessment in the 12 months to May 2015.
With respect to immunisations that target respiratory infections, the National Immunisation Program [200] differs between Aboriginal and Torres Strait Islander children and non-Indigenous children with respect to; a) influenza vaccine (which is funded for the former from six months to < five years of age and for those aged 15 years and over), and; b) an extra dose of the 13-valent pneumococcal conjugate vaccine is scheduled for between 12 and 18 months of age for those living in high risk areas of the NT, Qld, WA and South Australia. The 23-valent pneumococcal polysaccharide vaccine is recommended for Aboriginal and Torres Strait Islander people aged 15 to 49 years with medical risk factors. As the Australian Childhood Immunisation Register (now known as the Australian Immunisation Register) has only just been expanded to include immunisation data on children over seven years of age, data on uptake and coverage in older children are limited. However, while the data are limited, uptake of influenza vaccine in Aboriginal and Torres Strait Islander children in some communities is poor [39, 201] and timeliness of all childhood immunisations in these children remains problematic [202, 203].
Non-government based programs and services
The websites of both the Lung Foundation Australia and Asthma Australia have Aboriginal and Torres Strait Islander-specific components (http://lungfoundation.com.au/patient-support/indigenous/) and https://www.asthmaaustralia.org.au/qld/education-and-training/i-am-a-health-professional/aboriginal-and-torres-strait-islander-health-services.
National initiatives
Overall, Aboriginal and Torres Strait Islander early child health and development is a priority in the Council of Australian Government’s Close the Gap initiative [35]. The National Aboriginal and Torres Strait Islander Health Plan 2013–2023 [204] includes an expansion of the focus on child health to broader issues in child development. There are many national initiatives in Aboriginal and Torres Strait Islander health that may directly or indirectly reduce the burden of respiratory disease in children (e.g. housing initiatives, Aboriginal and Torres Strait Islander specific immunisation programs, programs to reduce tobacco smoke exposure and funding of key research organisations such as The Lowitja Institute and the new Central Australia Academic Health Science Centre, to name a few). Monitoring trends in disease over time is important and the regular collection, analysis and publication of relevant data occurs via studies such as the National Aboriginal and Torres Strait Islander health surveys, the Health performance framework reports and the Health and welfare of Aboriginal and Torres Strait Islander people reports. As described above, initiatives aimed at screening, and early detection and management of disease such as the 715 health checks are also operating at a national level. What is lacking however, are evaluations of the impacts of national initiatives on respiratory disease in Aboriginal and Torres Strait Islander children, other than monitoring broad trends in rates over time.
Policies and strategies
As with the national initiatives described above there are a broad range of policies and strategies at national, state, local government and community levels that may directly and/or indirectly address the respiratory health of Aboriginal and Torres Strait Islander children. It is beyond the scope of this review to describe them all. Examples include the National Early Childhood Development Strategy [205] that aims to strengthen universal maternal, child and health services. Specific programs include: New Directions: Mothers and Babies Services, Australian Nurse Family Partnership, Strong Fathers Strong Families and Healthy for Life.
State governments have specific Aboriginal and Torres Strait Islander units and health strategies. At the community level, health service providers including Aboriginal community controlled health organisations, divisions of general practice, public health networks and not-for profit organisations have various programs ranging from smoking interventions to healthy housing initiatives.
Future directions and research needs
Despite the importance of respiratory diseases in Aboriginal and Torres Strait Islander children, and their long-term consequences, as highlighted throughout this review, the available data with which to inform and evaluate interventions are now ageing. Further, there are inadequate data on children in urban and regional areas compared with remote areas despite the majority of Australia’s Aboriginal and Torres Strait Islander people living in such areas. Epidemiological studies to describe the burden of disease identify possible points of intervention, and monitor trends over time, are largely limited to hospitalisation data. There are very few clinical trials of interventions that have been or are being conducted in this population. Therapeutic studies that address the severity and consequences of common respiratory problems in young Aboriginal and Torres Strait Islander children are needed [181]. With advances in laboratory techniques, it is now becoming possible to better understand the role and relative importance of infectious organisms in lung disease in children, essential to informing the use of vaccines and antibiotics/antivirals. Ideally, longitudinal studies of infection and immunity in Aboriginal and Torres Strait Islander children that start in the antenatal period and continue throughout early childhood are required. Critically, these need to cover different geographic regions of Australia and incorporate the social and environmental determinants of disease. The development and evaluation of programs to support Aboriginal and Torres Strait Islander health care providers and community members in addressing lung health are urgently needed, as are the development and evaluation of educational resources for families in remote, regional and urban settings. Finally, larger studies conducted in different settings are needed to better understand Aboriginal and Torres Strait Islander perceptions of respiratory health from within an Indigenous paradigm to ensure programs, strategies and interventions are relevant and acceptable.
Concluding comments
Respiratory illnesses in Aboriginal and Torres Strait Islander children are serious, important and the progression to chronic lung disease is mostly preventable. The burden of disease in some regions is comparable to that of low-income countries [36, 206]. However, the lung health of Aboriginal and Torres Strait Islander children receives scant attention compared with adult lung disease, cystic fibrosis, diabetes and cardiovascular disease. To reduce the burden of respiratory illness in Aboriginal and Torres Strait Islander children, best-practice medicine is essential in addition to improving socioeconomic factors, reducing harmful exposures, and addressing access to culturally acceptable health care and illness prevention programs that likely contribute to disease [181]. A detailed description of primary, secondary and tertiary preventative measures that addresses these points has been previously published [181]. Ultimately, significant change will only occur once the broader determinants of respiratory health in Aboriginal and Torres Strait Islander children are adequately addressed. However, much can be done now to enable them to ‘breathe easy’ throughout their lifetime.
Glossary
adjusted odds ratio
the odds ratio (see below) considers the effect of one variable in an analysis, the adjusted odds ratio takes into account the effect due to additional variables being included in the analysis
adjusted relative risk
adjusts for confounding variables (e.g. age, gender) of the relative risk of an event occurring after exposure to a risk variable as compared with the likelihood of its occurrence in a control group
age-standardised
age-standardised rates enable comparisons of rates of respiratory disease between two populations that have different age structures. It is often used when comparing Aboriginal and Torres Strait Islander people and non-Indigenous people because the Aboriginal and Torres Strait Islander population has a younger age structure than the non-Indigenous population
confidence interval
gives an estimated range of values which is likely to include an unknown population parameter, the estimated range being calculated from a given set of sample data
interquartile range
a measure of where the middle fifty is in a data set. Where a range is a measure of where the beginning and end are in a set, an interquartile range is a measure of where the bulk of the values lie
odds ratio
a measure of association between an exposure and an outcome. The odds ratio represents the odds that an outcome will occur given a particular exposure, compared with the odds of the outcome occurring in the absence of that exposure
pooled odds ratio
the combined odds ratio of several studies
Abbreviations
ALRI – acute lower respiratory illness
aOR – adjusted odds ratio
ARI – acute respiratory illness/infection
aRR – adjusted relative risk
CI – confidence interval
CSLD – chronic suppurative lung disease
ED – emergency department
IQR – interquartile range
LRTI – lower respiratory tract infections
OR – odds ratio
Pooled OR – pooled odds ratio
PBB – protracted bacterial bronchitis
QoL – quality of life
URTI – upper respiratory tract infections
YLD – years of life with disability
References
- World Health Organization (2017) About chronic respiratory diseases. Retrieved 2017 from http://www.who.int/respiratory/about_topic/en/
- Australian Institute of Health and Welfare (2005) Chronic respiratory diseases in Australia: their prevalence, consequences and prevention. (AIHW Catalogue no PHE 63) Canberra: Australian Institute of Health and Welfare
- Australian Institute of Health and Welfare (2016) Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. (Australian Burden of Disease Study series no. 6, Cat no. BOD 7) Canberra: Australian Institute of Health and Welfare
- Australian Institute of Health and Welfare (2015) The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples 2015. (AIHW Catalogue no IHW 147) Canberra: Australian Institute of Health and Welfare
- Australian Institute of Health and Welfare (2017) Aboriginal and Torres Strait Islander Health Performance Framework. Retrieved 30 May 2017 from https://www.aihw.gov.au/reports/indigenous-health-welfare/health-performance-framework/contents/summary
- Steering Committee for the Review of Government Service Provision (2016) Overcoming Indigenous disadvantage: key indicators 2016 report. Canberra: Productivity Commission
- Redding G.J., Byrnes C.A. (2009) Chronic respiratory symptoms and diseases among indigenous children. Pediatric Clinics of North America;56(6):1323-1342
- Frumkin H, ed. (2010) Environmental health: from global to local. 2nd ed. San Francisco: Jossey-Bass
- Galobardes B, McCarron P, Jeffreys M, Davey Smith G (2008) Association between early life history of respiratory disease and morbidity and mortality in adulthood. Thorax;63(5):423-429
- Stocks J, Sonnappa S (2013) Early life influences on the development of chronic obstructive pulmonary disease. Therapeutic Advances in Respiratory Disease;7(3):161-173
- Svanes C, Sunyer J, Plana E, Dharmage S, Heinrich J, Jarvis D, de Marco R, Norbäck D, Raherison C, Villani S, Wjst M, Svanes K, Antó JM (2010) Early life origins of chronic obstructive pulmonary disease. Thorax;65(1):14-20
- Raphael B, Swan P, Martinek N (1998) Intergenerational aspects of trauma for Australian Aboriginal people. In: Danieli Y, ed. International handbook of multigenerational legacies of trauma. New York: Springer:327-339
- Dudgeon P, Wright M, Paradies Y, Garvey D, Walker I (2014) Aboriginal social, cultural and historical contexts. In: Dudgeon P, Milroy H, Walker R, eds. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. 2nd ed. Canberra: Department of The Prime Minister and Cabinet:3-24
- Gracey M, Williams P, Houston S (1997) Environmental health conditions in remote and rural Aboriginal communities in Western Australia. Australian and New Zealand Journal of Public Health;21(5):511-518
- Gracey M, King M (2009) Indigenous health part 1: determinants and disease patterns. The Lancet;374(9683):65-75
- Priest N, MacKean T, Davis E, Waters E, Briggs L (2012) Strengths and challenges for Koori kids: harder for Koori kids, Koori kids doing well – exploring Aboriginal perspectives on social determinants of Aboriginal child health and wellbeing. Health Sociology Review;21(2):165-179
- Gee G, Dudgeon P, Schultz C, Hart A, Kelly K (2014) Aboriginal and Torres Strait Islander social and emotional wellbeing. In: Dudgeon P, Milroy H, Walker R, eds. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. 2nd ed. Canberra: Department of The Prime Minister and Cabinet:55-68
- Thompson SJ, Gifford SM, Thorpe L (2000) The social and cultural context of risk and prevention: food and physical activity in an urban Aboriginal community. Health Education & Behavior;27(6):725-743
- Parker R, Milroy H (2014) Aboriginal and Torres Strait Islander mental health: an overview. In: Dudgeon P, Milroy H, Walker R, eds. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. 2nd ed. Canberra: Department of The Prime Minister and Cabinet:25-38
- Atkinson J (2002) Trauma trails: recreating song lines: the transgenerational effects of trauma in Indigenous Australia. North Melbourne: Spinifex Press
- Penman R (2006) The ‘growing up’ of Aboriginal and Torres Strait Islander children: a literature review. (Occasional Paper No. 15) Canberra: Department of Families, Community Services and Indigenous Affairs
- DiGiacomo M, Delaney P, Abbott P, Davidson PM, Delaney J, Vincent F (2013) ‘Doing the hard yards’: carer and provider focus group perspectives of accessing Aboriginal childhood disability services. BMC Health Services Research 13.
- Thomas A, Cairney S, Gunthorpe W, Paradies Y, Sayers S (2010) Strong Souls: development and validation of a culturally appropriate tool for assessment of social and emotional well-being in Indigenous youth. Australian and New Zealand Journal of Psychiatry;44(1):40-48
- Walter M, Saggers S (2007) Poverty and social class. In: Walter M, Saggers S, eds. Social determinants of Indigenous health. Crows nest (NSW): Allen and Unwin:87-107
- Tarren‐Sweeney M, Hazell P (2006) Mental health of children in foster and kinship care in New South Wales, Australia. Journal of Paediatrics and Child Health;42(3):89-97
- Baba JT, Brolan CE, Hill PS (2014) Aboriginal medical services cure more than illness: a qualitative study of how Indigenous services address the health impacts of discrimination in Brisbane communities. International Journal for Equity in Health 13.
- Scrimgeour M, Scrimgeour D (2008) Health care access for Aboriginal and Torres Strait Islander people living in urban areas, and related research issues: a review of the literature. (Discussion paper series no. 5) Darwin: Cooperative Research Centre for Aboriginal Health
- Australian Bureau of Statistics, Australian Institute of Health and Welfare (2008) The health and welfare of Australia’s Aboriginal and Torres Strait Islander Peoples 2008. (ABS Catalogue no. 4704.0 and AIHW Catalogue no. IHW 21) Canberra: Australian Bureau of Statistics and Australian Institute of Health and Welfare
- Zubrick SR, Dudgeon P, Gee G, Glaskin B, Kelly K, Paradies Y, Scrine C, Walker R (2010) Social determinants of Aboriginal and Torres Strait Islander social and emotional wellbeing. In: Purdie N, Dudgeon P, Walker R, eds. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. Canberra: Department of Health and Ageing:75-90
- Standing Committee on Aboriginal and Torres Strait Islander Affairs (2001) We can do it! The needs of urban dwelling Aboriginal and Torres Strait Islander peoples. Canberra: House of Representatives, Parliament of the Commonwealth of Australia
- Browne-Yung K, Ziersch A, Baum F, Gallaher G (2013) Aboriginal Australians’ experience of social capital and its relevance to health and wellbeing in urban settings. Social Science & Medicine;97:20–28
- Askew DA, Schluter PJ, Spurling GKP, Bond CJR, Brown ADH (2013) Urban Aboriginal and Torres Strait Islander children’s exposure to stressful events: a cross-sectional study. Medical Journal of Australia;199(1):42-45
- Healing Foundation (2013) Growing up our children strong: the intergenerational trauma intitiative: volume 1. Canberra: Healing Foundation
- Young C, Tong A, Nixon J, Fernando P, Kalucy D, Sherriff S, Clapham K, Craig JC, Williamson A (2017) Perspectives on childhood resilience among the Aboriginal community: an interview study. Australian and New Zealand Journal of Public Health;41(4):405-410
- Australian Health Ministers’ Advisory Council (2017) Aboriginal and Torres Strait Islander Health Performance Framework 2017 report. Canberra: Department of the Prime Minster and Cabinet
- Chang AB, Chang CC, O’Grady K, Torzillo PJ (2009) Lower respiratory tract infections. Pediatric Clinics of North America;56(6):1303-1321
- Australian Bureau of Statistics (2017) Census of population and housing – counts of Aboriginal and Torres Strait Islander Australians, 2016. Canberra: Australian Bureau of Statistics
- Eades SJ, Taylor B, Bailey S, Williamson AB, Craig JC, Redman S (2010) The health of urban Aboriginal people: insufficient data to close the gap. Medical Journal of Australia;193(9):521-524
- Hall KK, Chang AB, Anderson J, Arnold D, Goyal V, Dunbar M, Otim M, O’Grady K-AF (2017) The incidence and short-term outcomes of acute respiratory illness with cough in children from a socioeconomically disadvantaged urban community in Australia: a community-based prospective cohort study. Frontiers in Pediatrics 5.
- National Aboriginal Health Strategy Working Party (1989) A national Aboriginal health strategy. Canberra: Department of Aboriginal Affairs
- Bell AM (2015) Respiratory illness in urban Indigenous children: risk and cultural context. University of Queensland, Brisbane
- Rudan I, O’Brien KL, Nair H, Liu L, Theodoratou E, Qazi S, Lukšić I, Fischer WCL, Black RE, Campbell H, Child Health Epidemiology Reference Group (CHERG) (2013) Epidemiology and etiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. Journal of Global Health 3.
- Marks G, Reddel H, Guevara-Rattray E, Ampon R (2013) Monitoring asthma in pregnancy: a discussion paper. (AIHW Catalogue no ACM 28) Canberra: Australian Institute of Health and Welfare
- Vardavas CI, Hohmann C, Patelarou E, Martinez D, Henderson AJ, Granell R, Sunyer J, Torrent M, Fantini MP, Gori D, Annesi-Maesano I, Slama R, Duijts L, de Jongste JC, Aurrekoetxea JJ, Basterrechea M, Morales E, Ballester F, Murcia M, Thijs C, Mommers M, Kuehni CE, Gaillard EA, Tischer C, Heinrich J, Pizzi C, Zugna D, Gehring U, Wijga A, Chatzi L, Vassilaki M, Bergström A, Eller E, Lau S, Keil T, Nieuwenhuijsen M, Kogevinas M (2016) The independent role of prenatal and postnatal exposure to active and passive smoking on the development of early wheeze in children. European Respiratory Journal;48(1):115-124
- Joubert BR, Håberg SE, Nilsen RM, Wang X, Vollset SE, Murphy SK, Huang Z, Hoyo C, Midttun Ø, Cupul-Uicab LA, Ueland PM, Wu MC, Nystad W, Bell DA, Peddada SD, London SJ (2012) 450K epigenome-wide scan identifies differential DNA methylation in newborns related to maternal smoking during pregnancy. Environmental Health Perspectives;120(10):1425-1431
- Maccani JZ, Maccani MA (2015) Altered placental DNA methylation patterns associated with maternal smoking: current perspectives. Advances in Genomics and Genetics;2015(5):205-214
- Abraham M, Alramadhan S, Iniguez C, Duijts L, Jaddoe VW, Den Dekker HT, Crozier S, Godfrey KM, Hindmarsh P, Vik T, Jacobsen GW, Hanke W, Sobala W, Devereux G, Turner S (2017) A systematic review of maternal smoking during pregnancy and fetal measurements with meta-analysis. PLOS ONE 12.
- McEvoy CT, Spindel ER (2017) Pulmonary effects of maternal smoking on the fetus and child: effects on lung development, respiratory morbidities, and life long lung health. Paediatric Respiratory Reviews;21:27-33
- Thomas DP, Glover M (2010) Smoking and Aboriginal and Torres Strait Islander and Māori children. Journal of Paediatrics and Child Health;46(9):516-520
- Joubert BR, Felix JF, Yousefi P, Bakulski KM, Just AC, Breton C, Reese SE, Markunas CA, Richmond RC, Xu C-J, Küpers LK, Oh SS, Hoyo C, Gruzieva O, Söderhäll C, Salas LA, Baïz N, Zhang H, Lepeule J, Ruiz C, Ligthart S, Wang T, Taylor JA, Duijts L, Sharp GC, Jankipersadsing SA, Nilsen RM, Vaez A, Fallin MD, Hu D, Litonjua AA, Fuemmeler BF, Huen K, Kere J, Kull I, Munthe-Kaas MC, Gehring U, Bustamante M, Saurel-Coubizolles MJ, Quraishi BM, Ren J, Tost J, Gonzalez JR, Peters MJ, Håberg SE, Xu Z, van Meurs JB, Gaunt TR, Kerkhof M, Corpeleijn E, Feinberg AP, Eng C, Baccarelli AA, Neelon SEB, Bradman A, Merid SK, Bergström A, Herceg Z, Hernandez-Vargas H, Brunekreef B, Pinart M, Heude B, Ewart S, Yao J, Lemonnier N, Franco OH, Wu MC, Hofman A, McArdle W, Van der Vlies P, Falahi F, Gillman MW, Barcellos LF, Kumar A, Wickman M, Guerra S, Charles M-A, Holloway J, Auffray C, Tiemeier HW, Smith GD, Postma D, Hivert M-F, Eskenazi B, Vrijheid M, Arshad H, Antó JM, Dehghan A, Karmaus W, Annesi-Maesano I, Sunyer J, Ghantous A, Pershagen G, Holland N, Murphy SK, DeMeo DL, Burchard EG, Ladd-Acosta C, Snieder H, Nystad W, Koppelman GH, Relton CL, Jaddoe VWV, Wilcox A, Melén E, London SJ (2016) DNA methylation in newborns and maternal smoking in pregnancy: genome-wide consortium meta-analysis. American Journal of Human Genetics;98(4):680-696
- Kouzouna A, Gilchrist FJ, Ball V, Kyriacou T, Henderson J, Pandyan AD, Lenney W (2016) A systematic review of early life factors which adversely affect subsequent lung function. Paediatric Respiratory Reviews;20:67-75
- Eldridge D, Sedgwick K, Cotter D (2017) Australia’s mothers and babies 2015: in brief. Canberra: Australian Institute of Health and Welfare
- Omer SB, Goodman D, Steinhoff MC, Rochat R, Klugman KP, Stoll BJ, Ramakrishnan U (2011) Maternal influenza immunization and reduced likelihood of prematurity and small for gestational age births: a retrospective cohort study. PLOS Medicine 8.
- Goodnight WH, Soper DE (2005) Pneumonia in pregnancy. Critical Care Medicine;33(10):S390-S397
- ANZIC Influenza Investigators, Webb SA, Pettilä V, Seppelt I, Bellomo R, Bailey M, Cooper DJ, Cretikos M, Davies AR, Finfer S, Harrigan PW, Hart GK, Howe B, Iredell JR, McArthur C, Mitchell I, Morrison S, Nichol AD, Paterson DL, Peake S, Richards B, Stephens D, Turner A, Yung M (2009) Critical care services and 2009 H1N1 influenza in Australia and New Zealand. New England Journal of Medicine;361(20):1925-1934
- Mangtani P, Mak TK, Pfeifer D (2009) Pandemic H1N1 infection in pregnant women in the USA. The Lancet;374(9688):429-430
- Maher L, Hope K, Torvaldsen S, Lawrence G, Dawson A, Wiley K, Thomson D, Hayen A, Conaty S (2013) Influenza vaccination during pregnancy: coverage rates and influencing factors in two urban districts in Sydney. Vaccine;31(47):5557-5564
- O’Grady K-A, F. ,, Dunbar M, Medlin LG, Hall KK, Toombs M, Meiklejohn J, McHugh L, Massey PD, Creighton A, Andrews RM (2015) Uptake of influenza vaccination in pregnancy amongst Australian Aboriginal and Torres Strait Islander women: a mixed-methods pilot study. BMC Research Notes 8.
- Lotter K, Regan AK, Thomas T, Effler PV, Mak DB (2017) Antenatal influenza and pertussis vaccine uptake among Aboriginal mothers in Western Australia. Australian and New Zealand Journal of Obstetrics and Gynaecology;Early view(https://doi.org/10.1111/ajo.12739)
- Moberley SA, Lawrence J, Johnston V, Andrews RM (2016) Influenza vaccination coverage among pregnant Indigenous women in the Northern Territory of Australia. Communicable Diseases Intelligence;40(23):E340-E346
- Naidu L, Chiu C, Habig A, Lowbridge C, Jayasinghe S, Wang H, McIntyre P, Menzies R (2013) Vaccine preventable diseases and vaccination coverage in Aboriginal and Torres Strait Islander people, Australia 2006–2010. Communicable Diseases Intelligence;37(December 2013 supplement):S1-S92
- Overton K, Webby R, Markey P, Krause V (2016) Influenza and pertussis vaccination coverage in pregnant women in the Northern Territory in 2015 – new recommendations to be assessed. The Northern Territory Disease Control Bulletin;23(4):1-8
- Srám RJ, Binková B, Dejmek J, Bobak M (2005) Ambient air pollution and pregnancy outcomes: a review of the literature. Environmental Health Perspectives;113(4):375-382
- Chakraborty J, Green D (2014) The relationship between industrial air pollution and social disadvantage in Australia: national and regional inequities. Air Quality and Climate Change;48(4):35-38
- Johnston FH, Bailie RS, Pilotto LS, C. H (2007) Ambient biomass smoke and cardio-respiratory hospital admissions in Darwin, Australia. BMC Public Health 7.
- Beckhaus AA, Garcia-Marcos L, Forno E, Pacheco-Gonzalez RM, Celedón JC, Castro-Rodriguez JA (2015) Maternal nutrition during pregnancy and risk of asthma, wheeze, and atopic diseases during childhood: a systematic review and meta-analysis. Allergy;70(12):1588-1604
- Pacheco-González RM, García-Marcos L, Morales E (2018) Prenatal vitamin D status and respiratory and allergic outcomes in childhood: a meta-analysis of observational studies. Pediatric Allergy and Immunology;29(3):243-253
- Binks MJ, Smith-Vaughan HC, Marsh R, Chang AB, Andrews RM (2016) Cord blood vitamin D and the risk of acute lower respiratory infection in Indigenous infants in the Northern Territory. Medical Journal of Australia;204(6):238e1-238e7
- Weetra D, Glover K, Buckskin M, Ah Kit J, Leane C, Mitchell A, Stuart-Butler D, Turner M, Yelland J, Gartland D, Brown SJ (2016) Stressful events, social health issues and psychological distress in Aboriginal women having a baby in South Australia: implications for antenatal care. BMC Pregnancy and Childbirth 16.
- Mah B, Weatherall L, Burrows J, Blackwell CC, Gwynn J, Wadhwa P, Lumbers ER, Smith R, Rae KM (2017) Post-traumatic stress disorder symptoms in pregnant Australian Indigenous women residing in rural and remote New South Wales: A cross-sectional descriptive study. Royal Australian and New Zealand College of Obstetricians and Gynaecologists;57(5):520-525
- Prandl KJ (2017) Stress and pregnancy in Western Australian Aboriginal women. Curtin University, Perth
- Cheng TL, Johnson SB, Goodman E (2016) Breaking the intergenerational cycle of disadvantage: the three generation approach. Pediatrics 137.
- Tegethoff M, Greene N, Olsen J, Schaffner E, Meinlschmidt G (2011) Stress during pregnancy and offspring pediatric disease: a national cohort study. Environmental Health Perspectives;119(11):1647-1652
- Sania A, Brittain K, Phillips TK, Zerbe A, Ronan A, Myer L, Abrams EJ (2017) Effect of alcohol consumption and psychosocial stressors on preterm and small-for-gestational-age births in HIV-infected women in South Africa: a cohort study. BMJ Open 7.
- Martino D, Prescott S (2011) Epigenetics and prenatal influences on asthma and allergic airways disease. Chest;139(3):640-647
- Trueba AF, Ritz T (2013) Stress, asthma, and respiratory infections: pathways involving airway immunology and microbial endocrinology. Brain, Behavior, and Immunity;29:11-27
- Smejda K, Polanska K, Merecz-Kot D, Krol A, Hanke W, Jerzynska J, Stelmach W, Majak P, Stelmach I (2018) Maternal stress during pregnancy and allergic diseases in children during the first year of life. Respiratory Care;63(1):70-76
- DiGiacomo M, Davidson PM, Davison J, Moore L, Abbott P (2007) Stressful life events, resources, and access: key considerations in quitting smoking at an Aboriginal Medical Service. Australian and New Zealand Journal of Public Health;31(2):174-176
- Wood L, France K, Hunt K, Eades S, Slack-Smith L (2008) Indigenous women and smoking during pregnancy: knowledge, cultural contexts and barriers to cessation. Social Science & Medicine;66(11):2378-2389
- Australian Government Department of Health (2018) Clinical practice guidelines: pregnancy care. Canberra: Australian Government Department of Health
- Apte K, Salvi S (2016) Household air pollution and its effects on health. F1000Research 5.
- Mendell MJ (2007) Indoor residential chemical emissions as risk factors for respiratory and allergic effects in children: a review. Indoor Air;17(4):259-277
- Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J (2011) Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environmental Health Perspectives;119(6):748-756
- Australian Bureau of Statistics (2016) National Aboriginal and Torres Strait Islander Social Survey, 2014-15. Canberra: Australian Bureau of Statistics
- Vanker A, Gie RP, Zar HJ (2017) The association between environmental tobacco smoke exposure and childhood respiratory disease: a review. Expert Review of Respiratory Medicine;11(8):661-673
- Prietsch SO, Fischer GB, César JA, Lempek BS, Barbosa LVJ, Zogbi L, Cardoso OC, Santos AM (2008) Acute lower respiratory illness in under-five children in Rio Grande, Rio Grande do Sul State, Brazil: prevalence and risk factors. Cadernos de Saúde Pública;24(6):1429-1438
- Howie SR, Schellenberg J, Chimah O, Ideh RC, Ebruke BE, Oluwalana C, Mackenzie G, Jallow M, Njie M, Donkor S, Dionisio KL, Goldberg G, Fornace K, Bottomley C, Hill PC, Grant CC, Corrah T, Prentice AM, Ezzati M, Greenwood BM, Smith PG, Adegbola RA, Mulholland K (2016) Childhood pneumonia and crowding, bed-sharing and nutrition: a case-control study from The Gambia. International Journal of Tuberculosis and Lung Disease;20(10):1405-1415
- Australian Institute of Health and Welfare (2017) National Social Housing Survey: detailed results 2016. Canberra: Australian Institute of Health and Welfare
- Kamper-Jørgensen M, Benn CS, Simonsen J, Thrane N, Wohlfahrt J (2010) Clustering of acute respiratory infection hospitalizations in childcare facilities. Acta Paediatrica;99(6):877-882
- Sarna M, Ware RS, Sloots TP, Nissen MD, Grimwood K, Lambert SB (2016) The burden of community-managed acute respiratory infections in the first 2-years of life. Pediatric Pulmonology;51(12):1336-1346
- Chen Y, Williams E, Kirk M (2014) Risk factors for acute respiratory infection in the Australian community. PLOS ONE 9.
- Martin ET, Fairchok MP, Stednick ZJ, Kuypers J, Englund JA (2013) Epidemiology of multiple respiratory viruses in childcare attendees. The Journal of Infectious Diseases;207(6):982-989
- Sacri AS, De S, G.,, Quach C, Boulianne N, Valiquette L, Skowronski DM (2014) Transmission of acute gastroenteritis and respiratory illness from children to parents. The Pediatric Infectious Disease Journal;33(6):583-588
- Cardoso AM, Coimbra CEJ, Werneck GL (2013) Risk factors for hospital admission due to acute lower respiratory tract infection in Guarani Indigenous children in southern Brazil: a population-based case-control study. Tropical Medicine & International Health;18(5):596-607
- Dockery DW, Pope CA (1994) Acute respiratory effects of particulate air pollution. Annual Review of Public Health;15(1):107-132
- Neas LM, Dockery DW, Ware JH, Spengler JD, Ferris BG, Speizer FE (1994) Concentration of indoor particulate matter as a determinant of respiratory health in children. American Journal of Epidemiology;139(11):1088-1099
- Clifford H, Teo T, Kirkham L-A, Thornton R, Zosky G, Pickering J (2016) Dust exposure impacts haemophilus influenzae attachment and invasion of human airway epithelial cells. European Respiratory Journal;48(Suppl 60):PA4266
- Horton R (2009) Where are we now with Indigenous health? The Lancet;374(9683):2
- Human Rights and Equal Opportunity Commission (1997) Bringing them home: report of the National Inquiry into the Separation of Aboriginal and Torres Strait Islander Children from their Families. Sydney: Human Rights and Equal Opportunity Commission
- Petchkovsky L, San Roque C (2002) Tjunguwiyanytja, attacks on linking: forced separation and its psychiatric sequelae in Australia’s ‘stolen generations’. Transcultural Psychiatry;39(3):345-366
- Thomas DP, Briggs V, Anderson IPS, Cunningham J (2008) The social determinants of being an Indigenous non-smoker. Australian and New Zealand Journal of Public Health;32(2):110-116
- Fast E, Collin-Vézina D (2010) Historical trauma, race-based trauma and resilience of Indigenous peoples: a literature review. First Peoples Child & Family Review;5(1):126-136
- Hall KK, Chang AB, Anderson J, Dunbar M, Arnold D, O’Grady KF (2017) Characteristics and respiratory risk profile of children aged less than 5 years presenting to an urban, Aboriginal-friendly, comprehensive primary health practice in Australia. Journal of Paediatrics and Child Health;53(7):636-643
- Australian Bureau of Statistics (2013) Australian Aboriginal and Torres Strait Islander health survey: first results, Australia, 2012-13. (ABS Catalogue no. 4727.0.55.001) Canberra: Australian Bureau of Statistics
- Smith G, White V (2010) Use of tobacco, alcohol, and over-the-counter and illicit substances among Indigenous students participating in the Australian Secondary Students Alcohol and Drug Survey 2008. Canberra: Department of Health and Ageing, Australia
- National Academies of Sciences Engineering and Medicine (2017) Respiratory disease: chapter 7. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, DC: National Academies Press:486
- Lee KSK, Conigrave KM, Patton GC, Clough AR (2009) Cannabis use in remote Indigenous communities in Australia: endemic yet neglected [editorial]. Medical Journal of Australia;190(5):228-229
- Iede MA, Nunn K, Milne B, Fitzgerald DA (2017) The consequences of chronic cannabis smoking in vulnerable adolescents. Paediatric Respiratory Reviews;24:44-53
- Paaso EM, Jaakkola MS, Lajunen TK, Hugg TT, Jaakkola JJ (2013) The importance of family history in asthma during the first 27 years of life. American Journal of Respiratory and Critical Care Medicine;188(5):624-626
- Hersh CP, Hokanson JE, Lynch DA, Washko GR, Make BJ, Crapo JD, Silverman EK, COPDGene Investigators (2011) Family history is a risk factor for COPD. Chest;140(2):343-350
- Gao Y, Goldstein AM, Consonni D, Pesatori AC, Wacholder S, Tucker MA, Caporaso NE, Goldin L, Landi MT (2009) Family history of cancer and nonmalignant lung diseases as risk factors for lung cancer. International Journal of Cancer;125(1):146-152
- Kowal E, Rouhani L, Anderson I (2011) Genetic research in Aboriginal and Torres Strait Islander communities: beginning the conversation: discussion paper. Canberra: Lowitja Institute
- Millman AJ, Finelli L, Bramley AM, Peacock G, Williams DJ, Arnold SR, Grijalva CG, Anderson EJ, McCullers JA, Ampofo K, Pavia AT, Edwards KM, Jain S (2016) Community-acquired pneumonia hospitalization among children with neurologic disorders. The Journal of Pediatrics 173.
- Chan M, Park JJ, Shi T, Martinón-Torres F, Bont L, Nair H, Respiratory Syncytial Virus Network (ReSViNET) (2017) The burden of respiratory syncytial virus (RSV) associated acute lower respiratory infections in children with Down syndrome: A systematic review and meta-analysis. Journal of Global Health;7(2):020413
- Serel Arslan S, Demir N, Karaduman AA (2016) Both pharyngeal and esophageal phases of swallowing are associated with recurrent pneumonia in pediatric patients. Clinical Respiratory Journal;12(2):767-771
- Walker CL, Perin J, Katz J, Tielsch JM, Black RE (2013) Diarrhea as a risk factor for acute lower respiratory tract infections among young children in low income settings. Journal of Global Health;3(1):1-8
- Shukla SD, Budden KF, Neal R, Hansbro PM (2017) Microbiome effects on immunity, health and disease in the lung. Clinical & Translational Immunology;6(3):1-12
- Canani RB, Cirillo P, Roggero P, Romano C, Malamisura B, Terrin G, Passariello A, Manguso F, Morelli L, Guarino A (2006) Therapy with gastric acidity inhibitors increases the risk of acute gastroenteritis and community-acquired pneumonia in children. Pediatrics;117(5):817-820
- Cheung DS, Grayson MH (2012) Role of viruses in the development of atopic disease in pediatric patients. Current Allergy and Asthma Reports;12(6):613-620
- Martorano LM, Grayson MH (2018) Respiratory viral infections and atopic development: from possible mechanisms to advances in treatment. European Journal of Immunology;48(3):407-414
- Homaira N, Briggs N, Pardy C, Hanly M, Oei JL, Hilder L, Bajuk B, Lui K, Rawlinson W, Snelling T, Jaffe A. (2017) Association between respiratory syncytial viral disease and the subsequent risk of the first episode of severe asthma in different subgroups of high-risk Australian children: a whole-of-population-based cohort study. BMJ Open 7.
- McCallum GB, Chatfield MD, Morris PS, Chang AB (2016) Risk factors for adverse outcomes of Indigenous infants hospitalized with bronchiolitis. Pediatric Pulmonology;51(6):613-623
- Johnson RC, Schoeni RF (2011) Early-life origins of adult disease: national longitudinal population-based study of the United States. American Journal of Public Health;101(12):2317-2324
- Lee A, Ride K (2018) Review of nutrition among Aboriginal and Torres Strait Islander people. Perth, WA: Australian Indigenous HealthInfoNet
- Poulain M, Doucet M, Major GC, Drapeau V, Sériès F, Boulet LP, Tremblay A, Maltais F (2006) The effect of obesity on chronic respiratory diseases: pathophysiology and therapeutic strategies. Canadian Medical Association Journal;174(9):1293-1299
- Australian Government Department of Health (2014) Australia’s physical activity and sedentary behaviour guidelines. Canberra: Australian Government Department of Health
- Australian Bureau of Statistics (2014) Australian Aboriginal and Torres Strait Islander health survey: physical activity, 2012–13. (ABS cat. no. 4727.0.55.004) Canberra: Australian Bureau of Statistics
- Moore HC, Jacoby P, Taylor A, Harnett G, Bowman J, Riley TV, Reuter K, Smith DW, Lehmann D (2010) The interaction between respiratory viruses and pathogenic bacteria in the upper respiratory tract of asymptomatic Aboriginal and non-Aboriginal children. Pediatric Infectious Disease Journal;29(6):540-545
- O’Grady KF, Hall KK, Sloots TP, Anderson J, Chang AB (2017) Upper airway viruses and bacteria in urban Aboriginal and Torres Strait Islander children in Brisbane, Australia: a cross-sectional study. BMC Infectious Diseases 17.
- Chang AB, Smith-Vaughan H, Sloots TP, Valery PC, Whiley D, Beissbarth J, Torzillo PJ (2015) Upper airway viruses and bacteria detection in clinical pneumonia in a population with high nasal colonisation do not relate to clinical signs. Pneumonia;6(1):48-56
- O’Grady K-A, F.,, Whiley DM, Torzillo PJ, Sloots TP, Lambert SB (2013) Mailed versus frozen transport of nasal swabs for surveillance of respiratory bacteria in remote Indigenous communities in Australia. BMC Infectious Diseases 13.
- Leach AJ, Wigger C, Beissbarth J, Woltring D, Andrews R, Chatfield MD, Smith-Vaughan H, Morris PS (2016) General health, otitis media, nasopharyngeal carriage and middle ear microbiology in Northern Territory Aboriginal children vaccinated during consecutive periods of 10-valent or 13-valent pneumococcal conjugate vaccines. International Journal of Pediatric Otorhinolaryngology;86:224-232
- O’Grady KA, Torzillo PJ, Rockett RJ, Whiley DM, Nissen MD, Sloots TP, Lambert SB (2011) Successful application of a simple specimen transport method for the conduct of respiratory virus surveillance in remote Indigenous communities in Australia. Tropical Medicine & International Health;16(6):766–772
- Moore HC, de Klerk N, Richmond P, Keil AD, Lindsay K, Plant A, Lehmann D (2009) Seasonality of respiratory viral identification varies with age and Aboriginality in metropolitan Western Australia. Pediatric Infectious Disease Journal;28(7):598-603
- Chang AB, Smith-Vaughan H, Sloots T, Valery PC, Whiley D, Beissbarth J, Torzillo P (2015) Upper airway viruses and bacteria detection in clinical pneumonia in a population with high nasal colonisation do not relate to clinical signs. . Pneumonia;21(6):48-56
- Annamalay AA, Khoo SK, Jacoby P, Bizzintino J, Zhang G, Chidlow G, Lee WM, Moore HC, Harnett GB, Smith DW, Gern JE, Le Souef PN, A Laing I, Lehmann D (2012) Prevalence of and risk factors for human rhinovirus infection in healthy Aboriginal and non-Aboriginal Western Australian children. Pediatric Infectious Disease Journal;31(7):673–679
- Leach AJ, Boswell JB, Asche V, Nienhuys TG, Mathews JD (1994) Bacterial colonization of the nasopharynx predicts very early onset and persistence of otitis media in Australian Aboriginal infants. Pediatric Infectious Disease Journal;13(11):983-9
- Sun W, Jacoby P, Riley TV, Bowman J, Leach AJ, Coates H, Weeks S, Cripps A, Lehmann D (2012) Association between early bacterial carriage and otitis media in Aboriginal and non-Aboriginal children in a semi-arid area of Western Australia: a cohort study. BMC Infectious Diseases 12.
- Watson K, Carville K, Bowman J, Jacoby P, Riley TV, Leach AJ, Lehmann D (2006) Upper respiratory tract bacterial carriage in Aboriginal and non-Aboriginal children in a semi-arid area of Western Australia. Pediatric Infectious Disease Journal;25(9):782-790
- Kearns T, Clucas D, Connors C, Currie BJ, Carapetis JR, Andrews RM (2013) Clinic attendances during the first 12 months of life for Aboriginal children in five remote communities of Northern Australia. PLOS ONE 8.
- Johanson RP, Hill P (2011) Indigenous health – a role for private general practice. Australian Family Physician;40(1/2):16-19
- Hayman NE, White NE, Spurling GK (2009) Improving Indigenous patients’ access to mainstream health services: the Inala experience. Medical Journal of Australia;190(10):604-606
- Davy C, Harfield S, McArthur A, Munn Z, Brown A (2016) Access to primary health care services for Indigenous peoples: a framework synthesis. International Journal for Equity in Health 15.
- Ou L, Chen J, Garrett P, Hillman K (2010) Ethnic and Indigenous access to early childhood healthcare services in Australia: parents’ perceived unmet needs and related barriers. Australian and New Zealand Journal of Public Health;35(1):30-37
- Anderson A, Crengle S, Kamaka ML, Chen T, Palafox N, Jackson-Pulver L (2006) Indigenous health in Australia, New Zealand, and the Pacific. The Lancet;367(9524):1775-1785
- Britt H, Miller GC, Henderson J, Charles J, Valenti L, Harrison C, Bayram C, Zhang C, Pollack AJ, O’Halloran J, Pan Y (2012) General practice activity in Australia 2011-12. (General practice series no.31) Sydney: Sydney University Press
- Britt H, Miller GC, Bayram C, Henderson J, Valenti L, Harrison C, Pan Y, Charles J, Pollack AJ, Chambers T, Gordon J, Wong C (2016) A decade of Australian general practice activity 2006-07 to 2015-16. (General practice series no.41) Sydney: Sydney University Press
- Australian Institute of Health and Welfare (2013) Aboriginal and Torres Strait Islander health performance framework 2012: detailed analyses. (AIHW Cat. no. IHW 94) Canberra: Australian Institute of Health and Welfare
- Ou L, Chen J, Ken Hillman K, Eastwood J (2010) The comparison of health status and health services utilisation between Indigenous and non-Indigenous infants in Australia. Australian and New Zealand Journal of Public Health;34(1):50-56
- Pyett P, Waples-Crowe P, van der Sterren A (2009) Engaging with Aboriginal communities in an urban context: some practical suggestions for public health researchers. Australian and New Zealand Journal of Public Health;33(1):51-54
- Clucas DB, Carville KS, Connors C, Currie B, Carapetis J, Andrews R (2008) Disease burden and health-care clinic attendances for young children in remote Aboriginal communities of northern Australia. Bulletin of the World Health Organization;86(4):275-281
- Goldfeld SR, Wright M, Oberklaid F (2003) Parents, infants and health care: utilization of health services in the first 12 months of life. Journal of Paediatrics and Child Health;39(4):249-253
- Hall KK, Chang AB, Anderson J, Arnold D, Otim Ml, O’Grady KF (2018) Health service utilisation amongst urban Aboriginal and Torres Strait Islander children aged younger than 5 years registered with a primary health-care service in South-East Queensland. Journal of Paediatrics and Child Health;Early view(https://doi.org/10.1111/jpc.13812)
- O’Grady K-AF, Chang AB (2010) Lower respiratory infections in Australian Indigenous children. Journal of Paediatrics and Child Health;46(9):461-465
- Moore HC, de Klerk N, Jacoby P, Richmond P, Lehmann D (2012) Can linked emergency department data help assess the out-of-hospital burden of acute lower respiratory infections? A population-based cohort study. BMC public health 12.
- O’Grady K-AF, Torzillo PJ, Chang AB (2010) Hospitalisation of Indigenous children in the Northern Territory for lower respiratory illness in the first year of life. Medical Journal of Australia;192(10):586-590
- Janu EK, Annabattula BI, Kumariah S, Zajaczkowska M, Whitehall JS, Edwards MJ, Lujic S, Masters IB (2014) Paediatric hospitalisations for lower respiratory tract infections in Mount Isa. Medical Journal of Australia;200(10):591-594
- Moore H, Burgner D, Carville K, Jacoby P, Richmond P, Lehmann D (2007) Diverging trends for lower respiratory infections in non-Aboriginal and Aboriginal children. Journal of Paediatrics and Child Health;43(6):451-457
- Bailey EJ, Maclennan C, Morris PS, Kruske SG, Brown N, Chang AB (2009) Risks of severity and readmission of Indigenous and non-Indigenous children hospitalised for bronchiolitis. Journal of Paediatrics and Child Health;45(10):593–597
- Duncan C, Williams K, Nathanson D, Thomas S, Cottier C, O’Meara M, Zwi K (2013) Emergency department presentations by Aboriginal children: issues for consideration for appropriate health services. Journal of Paediatrics and Child Health;49(9):E448–E450
- Chang AB, Bell SC, Torzillo PJ, King PT, Maguire GP, Byrnes CA, Holland AE, O’Mara P, Grimwood K (2015) Chronic suppurative lung disease and bronchiectasis in children and adults in Australia and New Zealand Thoracic Society of Australia and New Zealand guidelines. Medical Journal of Australia;202(1):21-23
- Chang AB, Upham JW, Masters IB, Redding GR, Gibson PG, Marchant JM, Grimwood K (2016) Protracted bacterial bronchitis: the last decade and the road ahead. Pediatric Pulmonology;51(3):225-242
- Wurzel DF, Marchant JM, Yerkovich ST, Upham JW, Petsky HL, Smith-Vaughan H, Masters B, Buntain H, Chang AB (2016) Protracted bacterial bronchitis in children: natural history and risk factors for bronchiectasis. Chest;150(5):1101-1108
- Chang AB, Redding GJ, Everard ML (2008) Chronic wet cough: protracted bronchitis, chronic suppurative lung disease and bronchiectasis. Pediatric Pulmonology;43(6):519-531
- Singleton RJ, Valery PC, Morris P, Byrnes CA, Grimwood K, Redding G, Torzillo PJ, McCallum G, Chikoyak L, Mobberly C, Holman RC, Chang AB (2014) Indigenous children from three countries with non-cystic fibrosis chronic suppurative lung disease/bronchiectasis. Pediatric Pulmonology;49(2):189–200
- National Asthma Council Australia (2016) Australian asthma handbook. Melbourne: National Asthma Council Australia
- Australian Institute of Health and Welfare (2015) Premature mortality in Australia 1997-2012. Retrieved 7 October 2015 from https://www.aihw.gov.au/reports/life-expectancy-death/premature-mortality-in-australia-1997-2012/contents/summary
- Chang AB, Grimwood K, Mulholland EK, Torzillo PJ (2002) Bronchiectasis in Indigenous children in remote Australian communities. Medical Journal of Australia;177(4):200-204
- Chang AB, Masel JP, Boyce NC, Torzillo PJ (2003) Respiratory morbidity in central Australian Aboriginal children with alveolar lobar abnormalities. Medical Journal of Australia;178(10):490-494
- O’Grady K, Torzillo P, Chang A (2010) Hospitalisation of Indigenous children in the Northern Territory for lower respiratory illness in the first year of life. Med J Aust;192(10):586-90
- McCallum GB, Morris PS, Grimwood K, Maclennan C, White AV, Chatfield MD, Sloots TP, Mackay IM, Smith-Vaughan H, McKay CC, Versteegh L, ,, Jacobsen N, Mobberley C, Byrnes CA, Chang AB (2015) Three-weekly doses of azithromycin for indigenous infants hospitalized with bronchiolitis: a multicentre, randomized, placebo-controlled trial. Frontiers in Pediatrics;3(32):1-9
- Lung Foundation Australia (2016) Lung Foundation Australian launches Australian Bronchiectasis Registry. Retrieved 18 February 2016 from https://lungfoundation.com.au/lung-foundation-australia-launches-australian-bronchiectasis-registry/
- Chang AB, Robertson CF, Van Asperen PP, Glasgow NJ, Mellis CM, Masters B, Teoh L, Tjhung I, Morris PS, Petsky HL, Willis C, Landau LI (2012) A multicentre study on chronic cough in children: burden and etiologies based on a standardized management pathway. Chest Journal;142(4):943 – 950
- Rothstein J, Heazlewood R, Fraser M (2007) Health of Aboriginal and Torres Strait Islander children in remote Far North Queensland: findings of the Paediatric Outreach Service. Medical Journal of Australia;186(10):519-521
- Jenkins CR, Chang AB, Poulos LM, Marks GB (2009) Asthma in Indigenous Australians: so much yet to do for Indigenous lung health (mind the gap – editorial). Medical Journal of Australia;190(10):530-531
- Morey MJ, Cheng AC, McCallum GB, Chang AB (2013) Accuracy of cough reporting by carers of Indigenous children. Journal of Paediatrics and Child Health;49(3):E199–E203
- Valery PC, Masters IB, Taylor B, Laifoo Y, O’Rourke PK, Chang AB (2010) An education intervention for childhood asthma by Aboriginal and Torres Strait Islander health workers: a randomised controlled trial. Medical Journal of Australia;192(10):574-579
- O’Grady KF, Revell A, Maguire G, Millonig R, Newman M, Reid D, Hill DC, Chang AB (2010) Lung health services for Aboriginal and Torres Strait Islander peoples in Queensland. Brisbane: Queensland Health
- Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M (2010) Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. Journal of Epidemiology & Community Health;64(4):284-291
- Chang AB, Marsh RL, Upham JW, Hoffman LR, Smith-Vaughan H, Holt D, Toombs M, Byrnes C, Yerkovich ST, Torzillo PJ, O’Grady KA, Grimwood K (2015) Toward making inroads in reducing the disparity of lung health in Australian Indigenous and New Zealand Māori children. Pediatric Pulmonology 3.
- Chang AB, Brown N, Toombs M, Marsh RL, Redding GJ (2014) Lung disease in Indigenous children. Paediatric Respiratory Reviews;15(4):325–332
- Chang AB, Robertson CF, van Asperen PP, Glasgow NJ, Masters IB, Teoh L, Mellis CM, Landau LI, Marchant JM, Morris PS (2013) A cough algorithm for chronic cough in children: a multicenter, randomized controlled study. Pediatrics;131(5):e1576-e1583
- O’Grady KF, Drescher BJ, Goyal V, Phillips N, Acworth J, Marchant JM, Chang AB (2017) Chronic cough postacute respiratory illness in children: a cohort study. Archives of Disease in Childhood;102:1044-1048
- Chang AB, Oppenheimer JJ, Weinberger M, Weir K, Rubin BK, Irwin RS (2016) Use of management pathways or algorithms in children with chronic cough: systematic reviews. Chest;149(1):106-119
- Chang AB, Oppenheimer JJ, Weinberger MM, Rubin BK, Weir K, Grant CC, Irwin RS, CHEST Expert Cough Panel (2017) Use of management pathways or algorithms in children with chronic cough: CHEST guideline and expert panel report. Chest;151(4):875-883
- Douros K, Alexopoulou E, Nicopoulou A, Anthracopoulos MB, Fretzayas A, Yiallouros P, Nicolaidou P, Priftis KN (2011) Bronchoscopic and high-resolution CT scan findings in children with chronic wet cough. Chest;140(2):317-323
- Goyal V, Grimwood K, Marchant J, Masters IB, Chang AB (2016) Pediatric bronchiectasis: no longer an orphan disease. Pediatric Pulmonology;51(5):450-469
- Hare KM, Singleton RJ, Grimwood K, Valery PC, Cheng AC, Morris PS, Leach AJ, Smith-Vaughan HC, Chatfield M, Redding G, Reasonover AL, McCallum GB, Chikoyak L, McDonald MI, Brown N, Torzillo PJ, Chang AB (2013) Longitudinal nasopharyngeal carriage and antibiotic resistance of respiratory bacteria in Indigenous Australian and Alaska native children with bronchiectasis. PLOS ONE;8(8):e70478
- Valery PC, Whop LJ, Morseu-Diop N, Garvey G, Masters IB, Chang AB (2016) Carers’ perspectives on an effective Indigenous health model for childhood asthma in the Torres Strait. Australian Journal of Rural Health;24(3):170-175
- Chang AB, Taylor B, Masters IB, Laifoo Y, Brown AD (2010) Indigenous healthcare worker involvement for Indigenous adults and children with asthma (review). Cochrane Database of Systematic Reviews;2010(5):1-25
- Valery PC, Whop LJ, Morseu-Diop N, Garvey G, Masters IB, Chang AB (2015) Carers’ perspectives on an effective Indigenous health model for childhood asthma in the Torres Strait. Australian Journal of Rural Health;Early view(http://dx.doi.org/10.1111/ajr.12257)
- Oeseburg B, Wynia K, Middel B, Reijneveld SA (2009) Effects of case management for frail older people or those with chronic illness: a systematic review. Nursing Research;58(3):201-210
- Chang AB, Bell SC, Torzillo PJ, King PT, Maguire GP, Byrnes CA, Holland AE, O’Mara P, Grimwood K, extended voting g (2015) Chronic suppurative lung disease and bronchiectasis in children and adults in Australia and New Zealand Thoracic Society of Australia and New Zealand guidelines. Med J Aust;202(1):21-3
- Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, Siminerio LM, Weinger K, Weiss MA (2012) National standards for diabetes self-management education. Diabetes Care;35(Suppl 1):S101-S108
- O’Grady KF, Revell A, Maguire GP, Millonig R, Newman MA, Reid DW, Hill DC, Chang AB (2011) Lung health care for Aboriginal and Torres Strait Islander Queenslanders: breathing easy is not so easy. Australian Health Review;35(4):512-519
- Mckay CC, Chang AB, Versteegh LA, McCallum GB (2015) Culturally appropriate flipcharts improve the knowledge of common respiratory conditions among Northern Territory Indigenous families. Health Promotion Journal of Australia;26(2):150-153
- Medlin LG, Chang AB, Fong K, Jackson R, Bishop P, Dent A, Hill DC, Vincent S, O’Grady KAF (2014) Indigenous Respiratory Outreach Care: the first 18 months of a specialist respiratory outreach service to rural and remote Indigenous communities in Queensland, Australia. Australian Health Review;38(4):447-453
- Asthma Australia (2018) Spacers. Retrieved 4 February 2018 from https://www.asthmaaustralia.org.au/national/about-asthma/manage-your-asthma/spacers
- Australian Government Department of Health (2016) Medicare health assessment for Aboriginal and Torres Strait Islander people (MBS item 715). Canberra: Australian Government Department of Health
- Australian Government Department of Health and Ageing (2013) The Australian immunisation handbook: 10th edition 2013. 10th ed. Canberra: Australian Government Department of Health and Ageing
- Regan AK, Mak DB, Thomas T, Effler PV (2016) Seasonal influenza vaccination in Aboriginal children in Western Australia in 2015. Australian Family Physician;45(10):641-642
- Royle J, Lambert SB (2015) Fifty years of immunisation in Australia (1964-2014): the increasing opportunity to prevent diseases. Journal of Paediatrics and Child Health;51(1):16-20
- Lovie-Toon YG, Hall KK, Chang AB, Anderson J, O’Grady KF (2016) Immunisation timeliness in a cohort of urban Aboriginal and Torres Strait Islander children. BMC Public Health 16.
- Australian Government Department of Health (2015) Implementation plan for the National Aboriginal and Torres Strait Islander Health Plan 2013–2023. Canberra: Australian Government Department of Health
- Council of Australian Governments (2009) Investing in the early years – a national early childhood development strategy. Canberra: Commonwealth of Australia
- O’Grady K-AF, Taylor-Thomson DM, Chang AB, Torzillo PJ, Morris PS, Mackenzie GA, Wheaton GR, Bauert PA, De Campo MP, De Campo JF, Ruben AR (2010) Rates of radiologically confirmed pneumonia as defined by the World Health Organization in Northern Territory Indigenous children. Medical Journal of Australia;192(10):592-595
[1] A limitation of Ou et al’s study was its clustered sampling design of postcodes, which excluded remote postcodes, postcodes on Aboriginal and Torres Strait Islander lands, and postcodes with a population in which more than 50% of children were Aboriginal and Torres Strait Islander.